J Educ Community Health. 9(3):123-132.
doi: 10.34172/jech.2022.28
Original Article
Educational Intervention in Promoting Fatty Liver Preventive Behaviors in Women: Using the Protection Motivation Theory
Nader Sharifi 1  , Masoumeh Hashemian 2
, Masoumeh Hashemian 2  , Zahra Rahimi 3, Hamid Joveini 2, *
, Zahra Rahimi 3, Hamid Joveini 2, *  , Ali Mehri 2
, Ali Mehri 2  , Reza Shahrabadi 2
, Reza Shahrabadi 2  , Vahid Rahmanian 4
, Vahid Rahmanian 4 
Author information:
1Department of Public Health, Khomein University of Medical Sciences, Khomein, Iran
2Department of Health Education, Faculty of Health, Sabzevar University of Medical Sciences, Sabzevar, Iran
3Student Research Committee, Sabzevar University of Medical Sciences, Sabzevar, Iran
4Research Center for Social Determinants of Health, Jahrom University of Medical Sciences, Jahrom, Iran
Abstract
Background: The aim of this study was to determine the effect of educational intervention on improving the preventive behaviors of fatty liver in women referring to comprehensive health service centers in Bardaskan using the protection motivation theory (PMT).
Methods: This quasi-experimental study was conducted on women aged 18-59 in Bardaskan in 2020. The sample size was determined as 128 according to the suggestion (Cohen), including 64 experimental and 64 control samples. The participants completed a researcher-made questionnaire consisting of three parts (demographic variables, constructs of PMT, and fatty liver prevention behaviors). The educational intervention for the experimental group was performed in 12 one-hour sessions over 4 weeks using lectures, group discussions, questions and answers, brainstorming, substitution experiences, and delivery of the designed educational booklet. Two months after the completion of the educational intervention, the questionnaire was completed again by all participants. The obtained data were analyzed by SPSS 21 using descriptive statistics, Chi-square test, independent t test, paired t test, ANCOVA test, and linear regression test.
Results: There was a significant difference between the mean scores of perceived susceptibility (P<0.001), perceived severity (P=0.002), perceived external and internal rewards (P=0.010), response efficiency (P=0.010), perceived cost (P<0.001), and behavior (P=0.028) between the experimental and control groups after the educational intervention.
Conclusion: Educational intervention based on PMT led to behavior modifications to promote the preventive behaviors of the fatty liver.
Keywords: Non-alcoholic Fatty Liver Disease, Behavior, Women, Protection Motivation Theory
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Sharifi N, Hashemian M, Rahimi Z, Joveini H, Mehri A, Shahrabadi R, et al. Educational intervention in promoting fatty liver preventive behaviors in women: using the protection motivation theory. J Educ Community Health. 2022; 9(3):123-132. doi:10.34172/jech.2022.28
Introduction
Non-alcoholic fatty liver disease (NAFLD) is a condition in which triglycerides accumulate in the liver cells of non-alcoholic individuals (1). NAFLD is one of the most common types of chronic liver disease in the world and its prevalence is still increasing (2). This condition is known as the presence of steatosis in > 5% of hepatocytes (3). Evidence suggests a complex, two-way relationship between NAFLD and heart disease (4). It seems that the increase in its prevalence is due to lifestyle changes (high-fat and high-calorie diet, low physical activity, central obesity, and type 2 diabetes mellitus), increasing age, and genetics (5). The prevalence of NAFLD in the United States, as well as in Europe and Asia, is reported to be between 10 and 30%. The highest prevalence of this disease was observed in the Middle East (31.79%) and South America (30.45%), while the lowest prevalence was found in Africa (13.48%) (6), which is expected to increase in the Middle East due to increased risk factors (7). In Iran, the prevalence of this disease is estimated at 21.5-31.5% (8); further, the results of a study in the northern region of Iran demonstrated the prevalence of the disease as 44.2% and 40.1% in men and women, respectively (9). No effective treatment has so far been identified for NAFLD, and therapies typically focus on how to treat fatty liver-related conditions such as obesity and hyperlipidemia (10). Therefore, the treatment of this disease mainly focuses on behavioral and lifestyle modification interventions, including diet, increased physical activity, and weight loss (11). Studies in Iran on preventing NAFLD have not simultaneously considered nutritional behaviors and physical activities. In addition, these studies have not used behavior change models (12-14). Due to the complexity of these behaviors, the theories or patterns of behavior change should be employed to create healthy behaviors (15). The protection motivation theory (PMT) is used to understand and predict health intentions and behaviors that protect a person from harmful events (Figure 1) (16-18). The latest version of the PMT was developed by Ronald Rogers in 1983 to better understand why people respond to potential health threats. According to this theory, both individual and environmental factors can encourage or discourage engagement in protective behaviors, and the impact of these factors is mediated by individual cognitive processes (19). PMT includes the constructs of perceived susceptibility, perceived severity, perceived external and internal rewards, perceived self-efficacy, response efficiency, perceived cost, protection motivation, and fear. Coping appraisal and threatening appraisal are also its two main cognitive processes (20,21) The people of Bardaskan, like other parts of Iran, are at risk of developing fatty liver, and people’s awareness of fatty liver prevention behaviors is low due to the lack of nutrition experts and knowledgeable sources in this field (22). Due to the major role of women in the management of the family food basket (23), it is predicted that this group can play an important role in promoting preventive behaviors of fatty liver. Thus, this study aimed to determine the effect of educational intervention on improving the preventive behaviors of fatty liver in women referring to comprehensive health service centers in Bardaskan using the PMT.
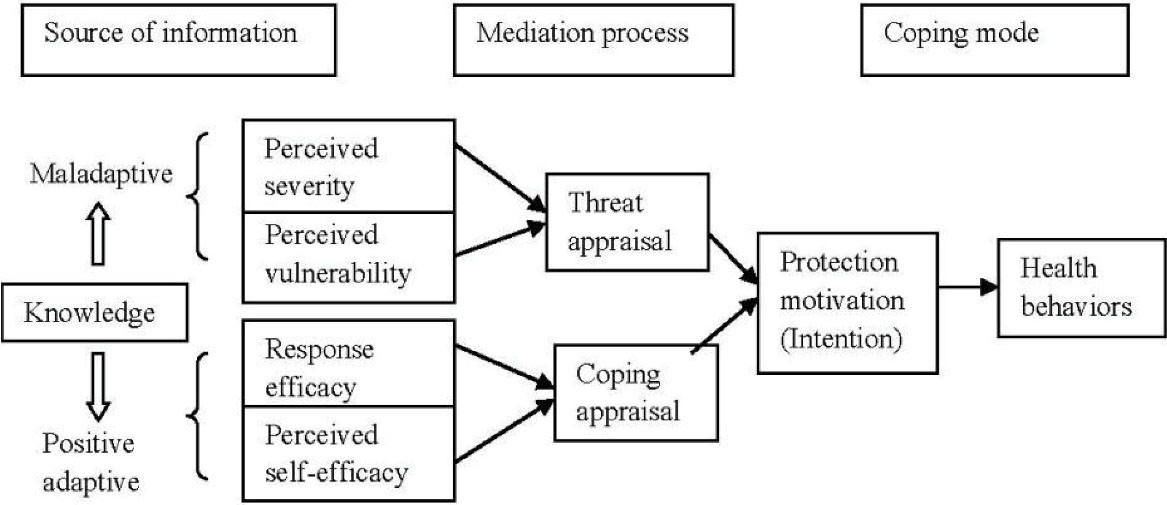
Figure 1.
Conceptual Framework Modified From Protection Motivation Theory of Rogers(24)
.
Conceptual Framework Modified From Protection Motivation Theory of Rogers(24)
Materials and Methods
This quasi-experimental study was conducted on women aged 18-59 in Bardaskan, Khorasan Razavi province (northeast of Iran) in 2020. The sample size was determined as 128 people based on the suggestion (Cohen) for the effect size of 0.5 and the study power (0.8); in general, 64 people were included in each group (experimental and control) (25). In the two-stage random sampling method, 2 centers were selected by lot from the urban comprehensive health service centers of Bardaskan to select the control and experimental group, respectively. Then, based on the electronic health record, individuals were selected by systematic random sampling and called to enter the study. The inclusion criteria included being women of the age group of 18-59 years, living in Bardaskan, and having an active health record in comprehensive health service centers, while the exclusion criteria were not signing the written consent form, not completing the questionnaire, having a history of the fatty liver according to the person’s own report, and not attending more than two training sessions for the experimental group.
The instrument used in this study was a researcher-made questionnaire consisting of three parts. The first part was related to the variables whose effects were considered in this study (age, height, weight, body mass index, waist, education, marital status, occupation, and family income, as well as the amount of physical activity, type of oil consumed, high blood pressure, diabetes, hyperlipidemia, and family history of the fatty liver). The second part was associated with the constructs of PMT (perceived susceptibility, perceived severity, perceived external and internal rewards, perceived self-efficacy, response efficiency, perceived cost, protection motivation, and fear). In total, this section of the questionnaire included 49 questions on a five-point Likert-type scale from strongly agree to strongly disagree. Depending on whether the question is positive or negative, they were awarded 0-4 points, divided into perceived susceptibility (7 questions, scores 0-28), perceived severity (n = 5, scores 0-20), perceived external and internal rewards (n = 4, scores 0-16; negative questions), and perceived self-efficacy (n = 6, scores 0-24). Additionally, the other questions were related to response efficiency (n = 5 scores 0-20), response costs (n = 7, scores 0-28; negative questions), protection motivation (n = 8, scores 0-32), and fear (n = 7, scores 0-28). The third section was related to fatty liver prevention behaviors in the field of lifestyle, including nutrition and physical activities in the form of 11 questions. This section had 4 answers (always, sometimes, rarely, and never), and a score of 0-3 was considered for each question.
A qualitative method was used to determine the face validity of the instrument. In the qualitative evaluation of face validity, the questionnaire was given to 30 women whose conditions were similar to those eligible for the study. Items such as the level of difficulty, comprehension of phrases and words, the degree of appropriateness, and the optimal relationship of phrases with the dimensions of the questionnaire were assessed, and both qualitative and quantitative methods were employed to determine content validity. In the qualitative section, the prepared pilot questionnaire was given to 10 health education and tool design specialists. They were asked to review the questionnaire based on the criteria of grammar, use of appropriate words, placement of items in the right place, appropriate scoring, and appropriateness of selected dimensions and questions related to constructs. At this stage, based on the evaluators’ suggestions, 5 and 4 questions were corrected and deleted, respectively. Both content validity ratio (CVR) and content validity index (CVI) were calculated in the quantitative evaluation of content validity. CVR values were accepted if they were higher than 0.62. At this stage, 4 questions were removed, and the minimum acceptable value for the CVI index was 0.79 (25). Items with a score of 0.7-0.79 were renegotiated with experts. Writing and conceptual deficiencies were corrected based on the evaluators’ suggestions. In the next stage, 5 questions were corrected, and the final questionnaire was organized accordingly.
The reliability of the questionnaire was determined using the test-retest method. In this way, the questionnaire was given to 30 women with similar conditions who were eligible for the study and was completed again by them after two weeks. The interclass correlation coefficient was calculated accordingly (Table 1).
Table 1.
The Validity and Reliability Values and Sample Questions of PMT Constructs
|
Construct
|
CVR
|
CVI
|
Interclass Correlation Coefficient
|
Sample Question
|
| Perceived susceptibility |
0.91 |
0.90 |
0.69 |
I am at risk for fatty liver. |
| Perceived severity |
0.88 |
0.91 |
0.86 |
Fatty liver increases the risk of liver cancer. |
| External and internal rewards |
0.71 |
0.79 |
0.6 |
Fast food (e.g., pizza, donuts, sausages, and the like) are highly tasty. |
| Perceived self-efficacy |
0.93 |
0.93 |
0.72 |
I can reduce the consumption of fast foods (e.g., pizza, donuts, sausages, and the like). |
| Response efficiency |
0.70 |
0.89 |
0.82 |
The risk of developing a fatty liver is reduced if I reduce my intake of high-fat and high-calorie foods. |
| Perceived cost |
0.83 |
0.88 |
0.69 |
My spouse/people around me prefer fast food. |
| Protection motivation |
0.92 |
0.91 |
0.78 |
I plan to prepare the food boiled and steamed instead of frying. |
| Fear |
0.94 |
0.93 |
0.94 |
I’m often worried about having fatty liver, similar to some of my fellow citizens. |
Note. CVR: Content validity ratio; CVI: Content validity index.
After inviting the participants and holding a briefing session on the objectives of the research, as well as creating confidence in terms of data confidentiality and completing the written consent form, the questionnaire was completed by them. The questionnaire was completed as a self-report; in addition, for illiterate people, it was completed by the questioner.
The educational intervention program was designed based on the results of analyzing the data obtained from the questionnaires, the use of valid sources and texts (8,10,11,26), and according to the constructs of PMT. The educational intervention for the experimental group was performed in 12 one-hour sessions in 4 weeks (4 sessions for each person according to the division of people into groups of 16 or 32 people) using lectures, group discussions, questions and answers, brainstorming, substitution experiences, and delivery of the designed educational booklet. The control group received their routine training programs (routine nutrition and physical activity training provided by health care providers in the centers) through comprehensive health service centers (Table 2).
Table 2.
The Educational Program for Intervention Group
|
Sessions
|
Objectives
|
A Summary of Topics and Activities
|
Educational Time (min)
|
| The first session |
Increasing the perceived susceptibility and severity of fatty liver |
Topics:
- Providing an introduction and communication with people
- Familiarizing individuals with fatty liver and its risk factors
- Informing about the prevalence of fatty liver
- Discussing the complications of fatty liver
- Discussing diseases associated with fatty liver
Training method and teaching aids: Lecturing with questions and answers and group discussion using the educational booklet and a data projector |
60 |
| The second session |
Reducing the perceived rewards as a result of misbehavior and reducing the perceived costs in order to achieve the correct behavior |
Topics:
- Providing an introduction and communicating with individuals
- Discussing the rewards that a person receives if they do wrong (wrong lifestyle)
- Discussing the obstacles and problems to having a proper diet
- Discussing the obstacles and problems to having enough physical activities
Training method: Brainstorming, lectures with questions and answers, and use of the educational booklet and data projector |
60 |
| The third session |
Increasing the self-efficacy and response efficiency of fatty liver prevention behaviors |
Topics:
- Providing an introduction and communicating with individuals
- Reassuring people modify their diet
- Assuring people have the necessary ability for regular mobility and physical activities
- Assuring people have the necessary ability to maintain an ideal weight
- Assuring people that the expected result will be achieved if the right behavior is done
Training method and teaching aids: Substitution experiences, group discussion with lectures and questions and answers using the educational booklet, and data projector |
60 |
| The fourth session |
Increasing the motivation of people to perform preventive behaviors for fatty liver and increasing fear about the complications and consequences of fatty liver disease |
Topics:
- Providing an introduction and communicating with individuals
- Motivating people to improve their diet
- Motivating people to increase mobility and physical activity on a regular basis
- Motivating people to study more about healthy foods and healthier cooking
Providing information about the symptoms of fatty liver and its complications that lead to problems and limitations in a person’s life.
Training method and teaching aids: Group discussions and lectures with questions and answers using the educational booklet and a data projector |
60 |
Two months after the completion of the educational intervention (Figure 2), the questionnaire was completed again by all participants, and the obtained data were analyzed by SPSS software, version 21. The mean (standard deviation) and frequency report (percentage) were used to describe quantitative and qualitative variables, respectively.
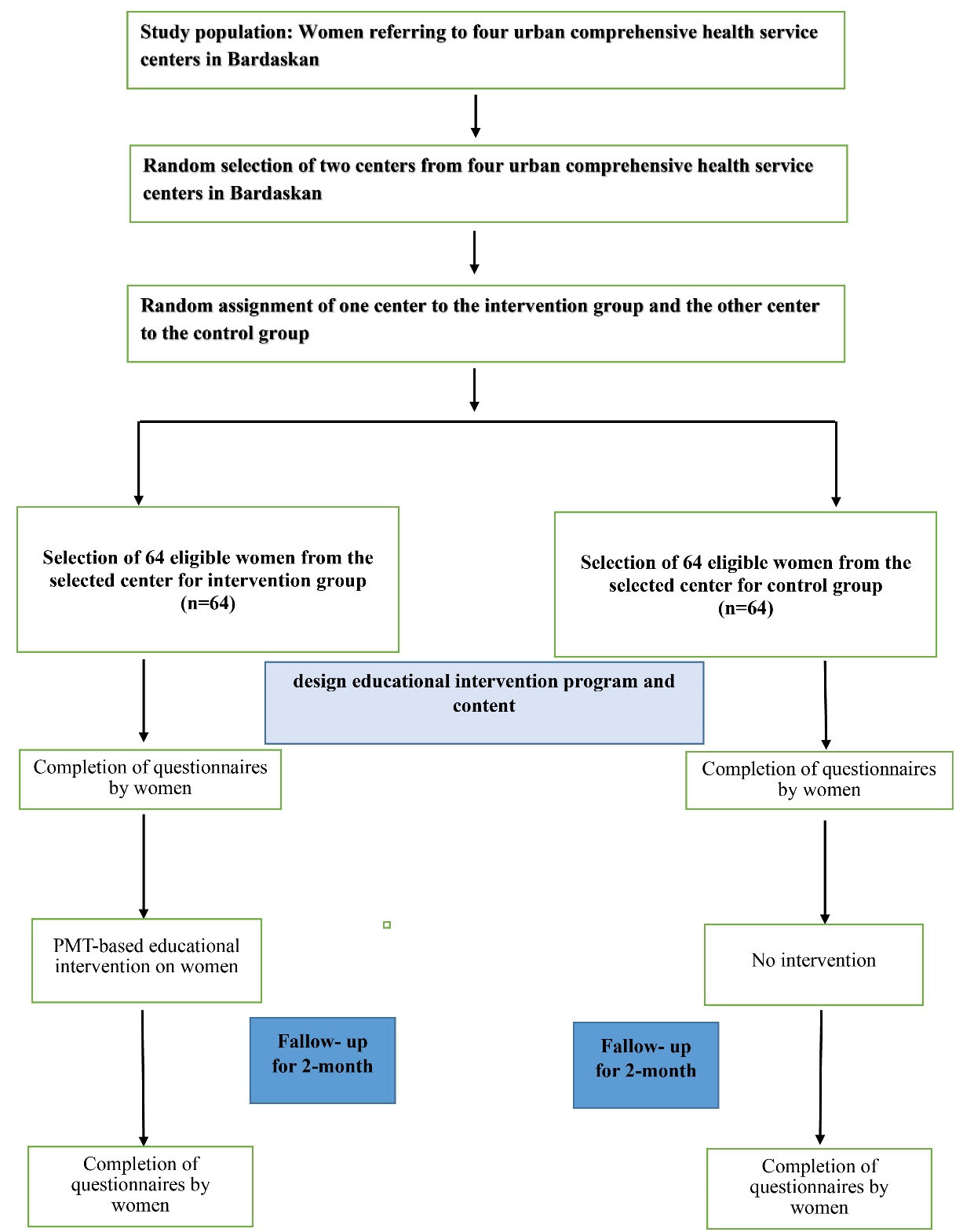
Figure 2.
Steps of Implementing the Research Plan
.
Steps of Implementing the Research Plan
A chi-square test was employed to compare qualitative factors between the studied groups. In addition, independent and paired t tests were used to compare the scores of PMT constructs in the experimental and control groups before and two months after the intervention. Further, the ANCOVA test was applied after the intervention to control the variables that led to a significant difference between the two groups before the intervention (pre-test).
Multiple linear regression by the ENTER technique was also used to investigate the relationship between the PMT constructs and behavior, and the significance level for all tests was less than 0.05.
Results
The number of participants was 128, and all of them were present until the end of the study. The results showed that most women were in the middle age (30-59 years) range (64.06%), had normal waist circumference (57.03%), and less than half of them had a normal body mass index (43.75%). The majority of participants had a diploma or higher degree (67.18%) and were married (92.18%) and housewives (67.18%). Most of them had unfavorable physical activity levels (86.71%), and the family income level was acceptable at 35.15%.
Chi-square test results demonstrated no significant difference between experimental and control groups in terms of demographic characteristics; however, regarding a family history of fatty liver, a significant difference was observed between the two groups (P = 0.024, Table 3).
Table 3.
Comparison of Frequency Distribution of Demographic Characteristics of Experimental and Control Groups
|
Variable
|
Grouping
|
Experimental Group No. (%)
|
Control Group No. (%)
|
P
Value
|
| Age |
Young (18-29) |
21 (32.8) |
25 (39.1) |
0.460 |
| Middle-aged (30-59) |
43 (67.2) |
39 (60.9) |
| BMI |
Underweight ( < 18.5) |
4 (6.2) |
3 (4.7) |
0.955 |
| Normal weight (18.5-24.9) |
28 (43.8) |
28 (43.8) |
| Overweight (25-29.9) |
21 (32.8) |
20 (31.2) |
| Obesity (30 or greater) |
11 (17.2) |
13 (20.3) |
| Waist circumference |
Abdominal obesity (90 cm or greater) |
24 (37.5) |
31 (48.4) |
0.731 |
| Normal ( < 90 cm) |
40 (62.5) |
33 (51.6) |
| Level of education |
Under diploma |
16 (25.0) |
26 (40.6) |
0.061 |
| Diploma and higher |
48 (75.0) |
38 (59.4) |
| Marital status |
Single |
1 (1.6) |
3 (4.7) |
0.640 |
| Married |
60 (93.8) |
58 (90.6) |
| Widow |
2 (3.1) |
1 (1.6) |
| Divorced |
1 (1.6) |
2 (3.1) |
| Job |
Housewife |
40 (62.5) |
46 (71.9) |
0.555 |
| Employee |
19 (29.7) |
12 (18.8) |
| Manual worker |
1 (1.6) |
1 (1.6) |
| Freelance |
4 (6.2) |
5 (7.8) |
| Family income |
Undergraduate |
8 (26.7) |
8 (26.7) |
0.081 |
| Weak |
30 (46.9) |
19 (29.7) |
| Medium |
17 (26.6) |
17 (26.6) |
| Good |
17 (26.6) |
28 (43.8) |
| Physical activity |
Unfavorable |
53 (82.8) |
58 (90.6) |
0.191 |
| Favorable |
11 (17.2) |
6 (9.4) |
| Type of oil consumed |
Only liquid oil |
27 (42.2) |
25 (39.1) |
0.931 |
| A combination of solid and liquid oils |
29 (45.3) |
30 (46.9) |
| Only solid oil |
8 (12.5) |
9 (14.1) |
| High blood pressure |
Yes |
6 (9.4) |
3 (4.7) |
0.302 |
| No |
58 (90.6) |
61 (95.3) |
| Type 2 diabetes |
Yes |
3 (4.7) |
4 (6.2) |
0.700 |
| No |
61 (95.3) |
60 (93.8) |
| Hyperlipidemia |
Yes |
3 (4.7) |
4 (6.2) |
0.700 |
| No |
61 (95.3) |
60 (93.8) |
| Family history of fatty liver |
Yes |
19 (29.7) |
8 (12.5) |
0.024 |
| No |
45 (70.3) |
56 (87.5) |
Note. BMI: Body mass index.
Based on the results, a significant difference was found between the mean scores of perceived susceptibility (P < 0.001), perceived severity (P = 0.002), perceived external and internal rewards (P = 0.01), response efficiency (P = 0.01), perceived cost (P < 0.001), and behavior (P = 0.028) between the experimental and control groups after the educational intervention, while there was no such difference before the intervention. According to the results, although there was a significant difference between the mean scores of experimental and control groups before the educational intervention in terms of protection motivation (P = 0.033) and fear (P = 0.045), this difference was much stronger with regard to protection motivation (P < 0.001) and fear (P < 0.001) after the intervention. A significant difference was found in the mean scores of the perceived self-efficacy construct in the experimental group before and after the educational intervention (P < 0.001); however, no significant difference was observed in the mean scores of this construct in the experimental and control groups after the educational intervention (Table 4).
Table 4.
Comparison of PMT Constructs in Experimental and Control Groups (Before and After Intervention)
|
Variable
|
Experimental (M±SD)
|
Control (M±SD)
|
P
Value
a
|
| Perceived susceptibility |
Before intervention |
16.82 ± 4.35 |
17.25 ± 4.81 |
0.600 |
| After intervention |
20.71 ± 3.18 |
17.06 ± 4.67 |
< 0.001 |
|
P valueb |
< 0.001 |
0.32 |
|
| Perceived severity |
Before intervention |
12.70 ± 2.80 |
13.59 ± 3.82 |
0.146 |
| After intervention |
15.01 ± 2.29 |
13.20 ± 3.92 |
0.002 |
|
P valueb |
< 0.001 |
0.42 |
|
| Perceived external and internal rewards |
Before intervention |
9.10 ± 3.14 |
8.98 ± 3.60 |
0.305 |
| After intervention |
7.57 ± 2.46 |
9.07 ± 3.55 |
0.010 |
|
P valueb |
< 0.001 |
0.56 |
|
| Perceived self-efficacy |
Before intervention |
18.31 ± 3.67 |
19.21 ± 3.56 |
0.163 |
| After intervention |
19.79 ± 2.88 |
19.17 ± 3.73 |
0.299 |
|
P valueb |
< 0.001 |
0.70 |
|
| Response efficiency |
Before intervention |
16.76 ± 3.13 |
17.14 ± 2.61 |
0.464 |
| After intervention |
18.09 ± 2.27 |
16.92 ± 2.69 |
0.010 |
|
P valueb |
< 0.001 |
0.15 |
|
| Perceived cost |
Before intervention |
12.01 ± 4.64 |
11.32 ± 5.72 |
0.464 |
| After intervention |
8.39 ± 3.20 |
11.64 ± 5.42 |
< 0.001 |
|
P valueb |
< 0.001 |
0.09 |
|
| Protection motivation |
Before intervention |
23.51 ± 5.13 |
25.40 ± 4.59 |
0.033 |
| After intervention |
26.06 ± 3.86 |
25.17 ± 4.42 |
< 0.001 |
|
P valueb |
< 0.001 |
0.18 |
|
| Fear |
Before intervention |
17.40 ± 6.05 |
19.70 ± 6.22 |
0.045 |
| After intervention |
21.42 ± 3.63 |
19.71 ± 6.01 |
< 0.001 |
|
P valueb |
< 0.001 |
0.93 |
|
| Behavior |
Before intervention |
17.17 ± 3.67 |
17.78 ± 3.49 |
0.345 |
| After intervention |
18.71 ± 3.21 |
17.35 ± 3.53 |
0.028 |
|
P valueb |
< 0.001 |
0.41 |
|
Note. PMT: Protection motivation theory; M: Mean; SD: Standard deviation.
a Independent t test; b Paired t test.
The ANCOVA test was applied to compare the means of variables in the two groups after adjusting covariates (Pre-test). The results represented a significant difference between the adjusted means in the groups in the post-test, highlighting the effectiveness of the intervention (Table 5).
Table 5.
Comparison of Means of PMT Constructs in Experimental and Control Groups After the Intervention by Adjusting the Effect of the Score Before the Intervention (Pre-test) Using ANCOVA Analysis
|
Variable
|
Mean Square
|
df
|
F
|
P
Value
|
Partial Eta Squared
|
| Perceived susceptibility |
Before intervention |
1472.66 |
1 |
337.13 |
< 0.001 |
0.730 |
| Group |
503.44 |
1 |
115.25 |
< 0.001 |
0.480 |
| Perceived severity |
Before intervention |
1111.13 |
1 |
737.97 |
< 0.001 |
0.855 |
| Group |
212.62 |
1 |
141.21 |
< 0.001 |
0.530 |
| Perceived external and internal rewards |
Before intervention |
1004.34 |
1 |
722.04 |
< 0.001 |
0.852 |
| Group |
129.65 |
1 |
93.20 |
< 0.001 |
0.427 |
| Perceived self-efficacy |
Before intervention |
1153.12 |
1 |
571.21 |
< 0.001 |
0.193 |
| Group |
60.19 |
1 |
28.82 |
< 0.001 |
0.193 |
| Response efficiency |
Before intervention |
576.79 |
1 |
328.21 |
< 0.001 |
0.724 |
| Group |
66.80 |
1 |
38.61 |
< 0.001 |
0.236 |
| Perceived cost |
Before intervention |
2082.49 |
1 |
617.61 |
< 0.001 |
0.832 |
| Group |
456.75 |
1 |
135.46 |
< 0.001 |
0.520 |
| Protection motivation |
Before intervention |
1751.51 |
1 |
519.62 |
< 0.001 |
0.806 |
| Group |
168.50 |
1 |
49.99 |
< 0.001 |
0.286 |
| Fear |
Before intervention |
2354.33 |
1 |
388.13 |
< 0.001 |
0.756 |
| Group |
340.68 |
1 |
56.16 |
< 0.001 |
0.310 |
| Behavior |
Before intervention |
1305.19 |
1 |
1213.23 |
< 0.001 |
0.907 |
| Group |
115.44 |
1 |
107.31 |
< 0.001 |
0.462 |
Note. PMT: Protection motivation theory; Adjusted variables: Perceived susceptibility, perceived severity, perceived external and internal rewards, perceived self-efficacy, response efficiency, perceived cost, protection motivation, fear, and behavior (Pre-test).
Based on the results of multiple linear regression, for one unit of change in the perceived self-efficacy, the average behavior score increased to 0.264 (P = 0.018, Table 6).
Table 6.
Factors Affecting Behavior Using Multivariable Linear Regression Model
|
Variable
|
B
|
SE
|
Standardized Coefficients Beta
|
P
value
|
| Perceived susceptibility |
0.125 |
0.107 |
0.160 |
0.048 |
| Perceived severity |
0.031 |
0.132 |
0.030 |
0.815 |
| Perceived external and internal rewards |
-0.009 |
0.097 |
-0.009 |
0.922 |
| Perceived self-efficacy |
0.264 |
0.110 |
0.257 |
0.018 |
| Response efficiency |
-0.033 |
0.152 |
-0.025 |
0.827 |
| Perceived cost |
-0.072 |
0.076 |
-0.098 |
0.350 |
| Protection motivation |
0.0108 |
0.090 |
0.131 |
0.229 |
| Fear |
-0.099 |
0.076 |
-0.145 |
0.0198 |
| Family history of fatty liver Yes/No |
0.342 |
1.21 |
0.024 |
0.780 |
Note. SE: Standard error; Model based on 128 observations, adjusted R-squared = 14.1%, P= 0.001.
Discussion
The results of the study revealed that the implementation of the PMT-based educational intervention in the experimental group was effective in improving all PMT constructs, protection motivation, and preventive behaviors of fatty liver. However, no change was observed in the control group receiving routine nutrition and physical activity training provided by health care providers in the centers.
The results also indicated that perceived susceptibility in the experimental group improved as a result of the educational intervention. In other words, individuals became more sensitive to fatty liver disease after the educational intervention. The results of Ebadi Fardazar et al showed that educational intervention, based on PMT on mothers’ behaviors, is effective in improving perceived susceptibility (27). Furthermore, the findings of Maseudi et al (28), Shobeiri et al (29), Ghahremani et al (30), Dehdari et al (31), and Fouda & Elkazeh (32) are consistent with those of the present study. Therefore, the level of the perceived susceptibility of individuals to make necessary changes in behavior can be improved by purposeful educational interventions.
Perceived severity improved after the educational intervention in the experimental group, while the score of this construct represented a significant decrease in the control group; in other words, the perception of the severity of the problem decreased among the control group, indicating the need for using theories and frameworks for better education. In Maseudi and colleagues study on male students, the results are similar in the control group, and the perceived severity score after the intervention has decreased as in the present study. In contrast to the current study, perceived severity did not improve as a result of the educational intervention (28). The findings of the present study conform to those of Pirzadeh and Amidi Mazaheri (33), Shobeiri et al (29), Bebis et al (34), and Fouda & Elkazeh (32). However, it contradicts the results of studies by Park et al (35), Dehdari et al (31, and Demirtas & Acikgoz (36), which can be related to the number of training sessions and the time spent on training, and finally how training has been effective. It seems that in the implementation of educational interventions, perceived severity should receive special attention, and appropriate programs should be designed and implemented to improve it.
The perceived external and internal reward scores in the experimental group significantly decreased after the educational intervention; in other words, after the educational intervention, individuals reviewed and corrected the preferences and rewards that they perceived and received in order to perform fatty liver-causing behaviors. This result is consistent with that of Maseudi et al, confirming the effectiveness of theory-based education (28). It should be mentioned that with effective education, one can influence the rewards that people perceive and receive for wrong behavior. After perceiving the severity and susceptibility of fatty liver disease, individuals seem to have reviewed and corrected the preferences and rewards they received for performing fatty liver-causing behaviors.
The perceived self-efficacy construct in the experimental group improved after the educational intervention; in other words, individuals became more confident in their ability to perform fatty liver prevention behaviors after the educational intervention. However, the perceived self-efficacy score in the experimental group was not significantly different from that of the control group after the intervention. In the study of Evenson, however, the educational intervention was not successful in improving self-efficacy (37). In other studies by Ebadi Fardazar et al (27) and Khiyali et al (38), perceived self-efficacy in women improved as a result of educational intervention based on PMT. Moreover, in the study of Ebadi Fardazar et al, similar to the present study, perceived self-efficacy decreased in the control group (27). These contradictory results show the high sensitivity of individuals’ self-efficacy and the importance of paying close attention to this construct in educational planning. The individuals’ belief in their ability to perform fatty liver prevention behaviors will gradually decrease if effective educational programs are not planned and implemented in the community.
Response efficiency in the experimental group improved after the educational intervention, thus people realized the effectiveness of the recommended behaviors in the prevention of fatty liver after the educational intervention. This result is consistent with the findings of Ebadi Fardazar et al (27) and Maseudi et al (28). These results confirm the effective role of the theory-based educational program to individuals in creating a sense of response efficiency.
The results indicated that the perceived cost in the experimental group significantly decreased after the educational intervention; in other words, people thought and took action to remove barriers to prevent fatty liver behaviors after the educational intervention. In studies performed by Ebadi Fardazar et al (27) and Khiyali et al (38) on women, the perceived cost score in the experimental group increased after the educational intervention, which is not consistent with the results of the present study. This discrepancy could be related to the education method and the ability of the educator to portray the benefits of the recommended behavior compared to perceived response costs.
The educational intervention improved protection motivation, thus people are more motivated to perform fatty liver prevention behaviors. These results are in line with those of Babazadeh et al (39), Maseudi et al (28), and Khiyali et al (38) studies. Therefore, using PMT-based education can improve people’s motivation to adopt behaviors to prevent fatty liver disease. It seems that when perceived susceptibility, perceived severity, and self-efficacy are at a higher level, they become more motivated to control risk and accept the recommended answers.
Fear in the experimental group improved after the educational intervention; more precisely, people’s fear of fatty liver disease and its possible complications increased after the educational intervention, which conforms to the findings of Ghahremani et al (30) and Khiyali et al (38). Conversely, in the study by Dehdari et al (31), the educational intervention was not effective on the fear structure in women to Pap test practice. It is emphasized that to succeed in achieving effective improvements in PMT constructs, it is necessary to design and implement training programs accurately and according to the characteristics of each construct.
The score of fatty liver prevention behaviors in the experimental group improved after the educational intervention, thus people attempted and acted to change the behavior as a result of the educational intervention based on the PMT. Similar results were obtained in the study by Ebadi Fardazar et al on women using the PMT (27). It should be noted that the PMT-based educational intervention to improve its constructs is effective in encouraging people to adopt behaviors to prevent fatty liver.
Perceived susceptibility and perceived self-efficacy were significant in linear regression, implying that these variables were good predictors of fatty liver preventive behaviors. In the above-mentioned study, perceived severity, self-efficacy, perceived response efficiency, and perceived cost had the power to predict behavior (27).
The large number of questions according to the studied variables and the number of PMT constructs can affect the accuracy of people’s answers. Considering that the study group included young and middle-aged women, problems were created due to the interference of data collection and implementation of educational interventions with the daily life of these people. To solve this problem, it was attempted to hold classes and collect data as much as possible at agreed times with the opinion of the participants. The final stages of the study coincided with the beginning of COVID-19 restrictions in the community, which the researchers followed in accordance with the health protocols of these stages, including the re-completion of questionnaires.
The strengths of this study were the design and development of an effective training program to promote preventive behaviors based on PMT and the presence of all participants until the end of the study.
Conclusion
Educational intervention based on PMT led to the improvement of PMT constructs and thus behavior modification to promote the preventive behaviors of fatty liver. Due to the low cost of preventive activities and the effectiveness of health education and promotion programs in comparison with therapeutic activities for fatty liver disease, it is necessary to generalize such educational programs and expand them to change health-related behaviors in the community. It is suggested that similar studies be performed on other age groups and men. The adoption of fatty liver prevention behaviors should also be followed for a longer period of time.
Acknowledgments
This article is taken from an MS thesis approved by Sabzevar University of Medical Sciences with code 97248. We thank the staff of Bardaskan Comprehensive Health Service Centers and the participants of this study.
Authors’ Contributions
Conceptualization: NS, HJ; Methodology: MH, NS, AM, RS; Validation: MH, RS; Formal Analysis: NS, VR; Investigation: ZR, AM; Data Curation: ZR, VR; Writing—Original Draft Preparation: NS, HJ; Writing—Review and Editing: NS, HJ; Visualization: HJ, AM; Project Administration: MH, HJ.
Conflict of Interests
The authors declare that there is no conflict of interests.
Ethical Permissions
Participants were briefed on the objectives of the research and assured of data confidentiality, and then the written consent form was completed by all participants. This research was approved by the Ethics Committee of Sabzevar University of Medical Sciences (Code IR.MEDSAB.REC.1397.132).
Funding/Support
This study was funded by Sabzevar University of Medical Sciences, Sabzevar, Iran.
References
- Ye Q, Zou B, Yeo YH, Li J, Huang DQ, Wu Y. Global prevalence, incidence, and outcomes of non-obese or lean non-alcoholic fatty liver disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2020; 5(8):739-52. doi: 10.1016/s2468-1253(20)30077-7 [Crossref] [ Google Scholar]
- Mikolasevic I, Milic S, Turk Wensveen T, Grgic I, Jakopcic I, Stimac D. Nonalcoholic fatty liver disease-a multisystem disease?. World J Gastroenterol 2016; 22(43):9488-505. doi: 10.3748/wjg.v22.i43.9488 [Crossref] [ Google Scholar]
- Soto-Angona Ó, Anmella G, Valdés-Florido MJ, De Uribe-Viloria N, Carvalho AF, Penninx B. Non-alcoholic fatty liver disease (NAFLD) as a neglected metabolic companion of psychiatric disorders: common pathways and future approaches. BMC Med 2020; 18(1):261. doi: 10.1186/s12916-020-01713-8 [Crossref] [ Google Scholar]
- Lonardo A, Nascimbeni F, Mantovani A, Targher G. Hypertension, diabetes, atherosclerosis and NASH: cause or consequence?. J Hepatol 2018; 68(2):335-52. doi: 10.1016/j.jhep.2017.09.021 [Crossref] [ Google Scholar]
- Zhu K, Guo Y, Zhao C, Kang S, Li J, Wang J. Etiology exploration of non-alcoholic fatty liver disease from traditional Chinese medicine constitution perspective: a cross-sectional study. Front Public Health 2021; 9:635818. doi: 10.3389/fpubh.2021.635818 [Crossref] [ Google Scholar]
- Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016; 64(1):73-84. doi: 10.1002/hep.28431 [Crossref] [ Google Scholar]
- Motamed N, Khoonsari M, Panahi M, Rezaie N, Maadi M, Safarnezhad Tameshkel F. The incidence and risk factors of non-alcoholic fatty liver disease: a cohort study from Iran. Hepat Mon 2020; 20(2):e98531. doi: 10.5812/hepatmon.98531 [Crossref] [ Google Scholar]
- Bagheri Lankarani K, Ghaffarpasand F, Mahmoodi M, Lotfi M, Zamiri N, Heydari ST. Non alcoholic fatty liver disease in southern Iran: a population based study. Hepat Mon 2013; 13(5):e9248. doi: 10.5812/hepatmon.9248 [Crossref] [ Google Scholar]
- Motamed N, Sohrabi M, Ajdarkosh H, Hemmasi G, Maadi M, Sayeedian FS. Fatty liver index vs waist circumference for predicting non-alcoholic fatty liver disease. World J Gastroenterol 2016; 22(10):3023-30. doi: 10.3748/wjg.v22.i10.3023 [Crossref] [ Google Scholar]
- Kelishadi R, Farajian S, Mirlohi M. Probiotics as a novel treatment for non-alcoholic fatty liver disease; a systematic review on the current evidences. Hepat Mon 2013; 13(4):e7233. doi: 10.5812/hepatmon.7233 [Crossref] [ Google Scholar]
- Nseir W, Hellou E, Assy N. Role of diet and lifestyle changes in nonalcoholic fatty liver disease. World J Gastroenterol 2014; 20(28):9338-44. doi: 10.3748/wjg.v20.i28.9338 [Crossref] [ Google Scholar]
- Tehrani M, Baji Z, Shakerinejad G, Hajinajaf S, Jarvandi F, Saki M. Effects of nutrition education on anthropometric indices, biochemical and sonographic findings of patients with non-alcoholic fatty liver disease (NAFLD). Iran J Health Educ Health Promot 2017; 5(1):33-42. doi: 10.18869/acadpub.ihepsaj.5.1.33.[Persian] [Crossref] [ Google Scholar]
- Paknahad Z, Zeraei-Bidgoli H. Metabolic syndrome and nonalcoholic fatty liver disease: nutritional approach for prevention. J Isfahan Med Sch 2013;31(252):1461-80. [Persian].
- Moradi Kohnaki Z, Asadollahi K, Abangah G, Sayehmiri K. Risk factors of nonalcoholic fatty liver disease: a case-control study. Tehran Univ Med J 2016;74(9):645-56. [Persian].
- Kohpeima Jahromi V, Bahlouli Ghashghaei S, Sharifi N. Improvement of osteoporosis-related behaviors in female students based on trans theoretical model. J Educ Health Promot 2020; 9:221. doi: 10.4103/jehp.jehp_213_20 [Crossref] [ Google Scholar]
- Bubeck P, Wouter Botzen WJ, Laudan J, Aerts J, Thieken AH. Insights into flood-coping appraisals of protection motivation theory: empirical evidence from Germany and France. Risk Anal 2018; 38(6):1239-57. doi: 10.1111/risa.12938 [Crossref] [ Google Scholar]
- Wang J, Liu-Lastres B, Ritchie BW, Mills DJ. Travellers’ self-protections against health risks: an application of the full protection motivation theory. Ann Tour Res 2019; 78:102743. doi: 10.1016/j.annals.2019.102743 [Crossref] [ Google Scholar]
- Sommestad T, Karlzén H, Hallberg J. A meta-analysis of studies on protection motivation theory and information security behaviour. Int J Inf Secur Priv 2015; 9(1):26-46. doi: 10.4018/ijisp.2015010102 [Crossref] [ Google Scholar]
- Clubb AC, Hinkle JC. Protection motivation theory as a theoretical framework for understanding the use of protective measures. Crim Justice Stud 2015; 28(3):336-55. doi: 10.1080/1478601x.2015.1050590 [Crossref] [ Google Scholar]
- Sadeghi R, Mazloomy Mahmoodabad SS, Fallahzadeh H, Rezaeian M, Bidaki R, Khanjani N. Predictive factors for preventing hookah smoking and health promotion among young people based on the protection motivation theory. J Educ Health Promot 2019; 8:169. doi: 10.4103/jehp.jehp_78_19 [Crossref] [ Google Scholar]
- Wang PW, Ahorsu DK, Lin CY, Chen IH, Yen CF, Kuo YJ. Motivation to have COVID-19 vaccination explained using an extended protection motivation theory among university students in China: the role of information sources. Vaccines (Basel) 2021; 9(4):380. doi: 10.3390/vaccines9040380 [Crossref] [ Google Scholar]
- Mataji Amirrood M, Taghdisi MH, Gohari MR, Shidfar F. The role of eating attitude on obesity-related eating behavior in overweight and obese women of Urmia in 2012. J Payavard Salamt 2015;8(6):464-77. [Persian].
- Omidvar N. Proceedings of food and nutrition discussion forum: nutrition and sustainable development. Iran J Nutr Sci Food Technol 2018;13(1):125-216. [Persian].
- Chamroonsawasdi K, Chottanapund S, Tunyasitthisundhorn P, Phokaewsuksa N, Ruksujarit T, Phasuksathaporn P. Development and validation of a questionnaire to assess knowledge, threat and coping appraisal, and intention to practice healthy behaviors related to non-communicable diseases in the Thai population. Behav Sci (Basel) 2017; 7(2):20. doi: 10.3390/bs7020020 [Crossref] [ Google Scholar]
- Wuensch K. Cohen’s Conventions for Small, Medium, and Large Effect Sizes. East Carolina University; 2015.
- Wong VW, Chu WC, Wong GL, Chan RS, Chim AM, Ong A. Prevalence of non-alcoholic fatty liver disease and advanced fibrosis in Hong Kong Chinese: a population study using proton-magnetic resonance spectroscopy and transient elastography. Gut 2012; 61(3):409-15. doi: 10.1136/gutjnl-2011-300342 [Crossref] [ Google Scholar]
- Ebadi Fardazar F, Hashemi SS, Solhi M, Mansori K. The effect of educational intervention based on protection motivation theory on mothers’ behaviors about prevention of home accidents in children under 5 year old. J Health Res Commun 2016;1(4):37-44. [Persian].
- Maseudi GR, Hosseini EO, Mirzaei R, Shahrakipour M, Hosseini SA. The effect of education based on protection motivation theory on the harmful effects of solar rays on male students. Iran J Health Educ Health Promot 2014;2(4):322-30. [Persian].
- Shobeiri F, Taravati Javad M, Parsa P, Roshanaei G. Effects of group training based on the health belief model on knowledge and behavior regarding the pap smear test in Iranian women: a quasi-experimental study. Asian Pac J Cancer Prev 2016; 17(6):2871-6. [ Google Scholar]
- Ghahremani L, Khiyali Harami Z, Kaveh MH, Keshavarzi S. Investigation of the role of training health volunteers in promoting pap smear test use among Iranian women based on the protection motivation theory. Asian Pac J Cancer Prev 2016; 17(3):1157-62. [ Google Scholar]
- Dehdari T, Hassani L, Hajizadeh E, Shojaeizadeh D, Nedjat S, Abedini M. Effects of an educational intervention based on the protection motivation theory and implementation intentions on first and second pap test practice in Iran. Asian Pac J Cancer Prev 2014; 15(17):7257-61. doi: 10.7314/apjcp.2014.15.17.7257 [Crossref] [ Google Scholar]
- Fouda LM, Elkazeh EA. The impact of an educational intervention on women’s knowledge and perception regarding cervical cancer and human papillomavirus vaccines in Tanta city: applying health belief model. Life Sci J 2013; 10(12):997-1005. [ Google Scholar]
- Pirzadeh A, Amidi Mazaheri M. The effect of education on women’s practice based on the health belief model about pap smear test. Int J Prev Med 2012; 3(8):585-90. [ Google Scholar]
- Bebis H, Reis N, Yavan T, Bayrak D, Unal A, Bodur S. Effect of health education about cervical cancer and papanicolaou testing on the behavior, knowledge, and beliefs of Turkish women. Int J Gynecol Cancer 2012; 22(8):1407-12. doi: 10.1097/IGC.0b013e318263f04c [Crossref] [ Google Scholar]
- Park S, Chang S, Chung C. Effects of a cognition-emotion focused program to increase public participation in Papanicolaou smear screening. Public Health Nurs 2005; 22(4):289-98. doi: 10.1111/j.0737-1209.2005.220404.x [Crossref] [ Google Scholar]
- Demirtas B, Acikgoz I. Promoting attendance at cervical cancer screening: understanding the relationship with Turkish womens’ health beliefs. Asian Pac J Cancer Prev 2013; 14(1):333-40. doi: 10.7314/apjcp.2013.14.1.333 [Crossref] [ Google Scholar]
- Evenson AL, Sanders GF. Educational intervention impact on osteoporosis knowledge, health beliefs, self-efficacy, dietary calcium, and vitamin D Intakes in young adults. Orthop Nurs 2016; 35(1):30-6. doi: 10.1097/nor.0000000000000211 [Crossref] [ Google Scholar]
- Khiyali Z, Ghahremani L, Kaveh MH, Keshavarzi S. The effect of an educational program based on protection motivation theory on pap smear screening behavior among women referring to health centers in Fasa. J Educ Community Health 2017; 3(4):31-7. doi: 10.21859/jech.3.4.31.[Persian] [Crossref] [ Google Scholar]
- Babazadeh T, Kamran A, Dargahi A, Moradi F, Shariat F, Rezakhani Moghaddam H. Skin cancer preventive behaviors among rural farmers: An intervention based on protection motivation theory. Med J Islam Repub Iran 2016; 30:444. [ Google Scholar]