J Educ Community Health. 10(1):1-7.
doi: 10.34172/jech.2023.2214
Original Article
Relationship Between Medication Literacy, Health Literacy, and Medication Behavior Among Medical School Students: A Cross-sectional Study
Chengyu An 1  , Yujia Wang 2, Bojunhao Feng 3, Jingbo Zhang 2, Ruyi Hou 4, Xincheng Huang 5, Zhu Zhu 6, Xinying Sun 7
, Yujia Wang 2, Bojunhao Feng 3, Jingbo Zhang 2, Ruyi Hou 4, Xincheng Huang 5, Zhu Zhu 6, Xinying Sun 7  , Yibo Wu 7, *
, Yibo Wu 7, * 
Author information:
1Department of Clinical Sciences, China Medical University, Shenyang, China
2School of Humanities and Social Sciences, Harbin Medical University, Harbin, China
3School of Medicine, Macau University of Science and Technology, Macau, China
4Department of Humanities, Arts and Media, Changzhi Medical School, Changzhi,China
5School of Economics and Management, Beijing Institute of Graphic Communication, Beijing, China
6Department of Pharmacy, Peking Union Medical school Hospital, Chinese Academy of Medical Sciences, Beijing, China
7School of Public Health, Peking University, Beijing, China
Abstract
Background: Nowadays, college students are more accessible and susceptible to being exposed to mixed information than ever, which results in a growing concern about their health problems and medication behaviors. This study aimed to investigate the correlation between medication literacy, health literacy, and medication behavior among medical school students.
Methods: A cluster random sampling method was used to select 1324 undergraduate students from a medical school in China as participants for the questionnaire survey in 2020. After quality control, 1183 valid questionnaires were collected (an effective rate of 89.4%). Descriptive statistics analysis, chi-square test, binary logistic regression analysis, and path analysis were conducted using SPSS 25.0.
Results: Of the 1183 respondents whose mean age was 19.06, 164 (13.9%) were considered to have good medication literacy, 150 (12.7%) had good health literacy, and 497(42.0%) exhibited good medication behaviors. Lower grades, higher health literacy levels, and higher medication literacy levels were effective in better performance on medication use behavior (P<0.001). Poor self-assessment of health status was correlated with worse medication behavior (P<0.05). it was concluded that medication literacy may be an intermediate variable linking health literacy and medication use behavior.
Conclusion: Students in the medical college showed much higher rates of rational medication use when they have medication and health literacy. There was an indirect positive relationship between health literacy and medication behavior through medication literacy (P<0.001). Therefore, health literacy and medication literacy can be an essential part of medication safety education for college students as well as an ideal indicator for educational outcome evaluation.
Keywords: Health literacy, Drug misuse, Health education, Cross-sectional studies
Copyright and License Information
© 2023 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: An C, Wang Y, Feng B, Zhang J, Hou R, Huang X, et al. Relationship between medication literacy, health literacy, and medication behavior among medical school students: a cross-sectional study. J Educ Community Health. 2023; 10(1):1-7. doi:10.34172/jech.2023.2214
Introduction
Health literacy is the ability of individuals to access and understand the use of health information and services to make sound decisions to maintain and promote their health. It has been further divided into three levels: functional health literacy, interactive health literacy, and critical health literacy. Functional health literacy refers to an individual’s ability to read and understand basic health-related information, while interactive health literacy is a more advanced cognitive and literacy skill that can be used to actively participate in daily activities, extract information, gain meaning from different forms of communication, and apply new information to a changing environment. Critical health literacy refers to the ability of individuals to critically think, analyze, and apply health information to better control the impact of life events and different situations on health (1). Medication literacy refers to an individual’s ability to appropriately access, understand, and use essential medication information to make correct evaluations and decisions (2).Since medication information is a part of health information, it can be inferred that medication literacy is a manifestation of health literacy in medication (3).
Studies demonstrated that people with health literacy behaved better regarding medication consultation, information acquisition, and information processing (4,5). There is also a positive relationship between health literacy and medication compliance (6,7). People with no health literacy reported more significant side effects and overuse concerns (8). Improving medication literacy and health literacy is key to managing medical conditions, improving medication compliance, and promoting self-medication safety (9-11).
Medication safety for college students is a severe topic worldwide. Irrational medication use behaviors include behaviors such as sharing and borrowing prescription drugs, taking drugs and alcohol in excessive doses, and taking drugs for relief (4,12,13). Although the relationship between health literacy, medication literacy, and medication use behavior has been demonstrated in patients, there are few reports on college students, most of which only focused on a specific medication such as antibiotics. Neither did they explore the three variables at the same time.
This study aimed to further explore the relationship between health literacy, medication literacy, and medication use behavior in medical undergraduate students to supplement existing studies and literature, to provide a theoretical basis and direction for the implementation of medication safety education, and to provide some suggestions for the evaluation of the implementation of educational activities.
The novelty of this study is that we selected a representative sample of undergraduate students from medical schools in Shaanxi, China, who seemed to have high health literacy and medication literacy which is appropriate for our study topic. We investigated medication use behaviors in general, not just for a specific medicine, to avoid the influence of medicine specificity on the study results. In addition, the direct and indirect effects of variables were measured and compared through path analysis to further reveal the nature of the relationship between the studied variables.
Materials and Methods
Participants
This is a cross-sectional survey of undergraduate students enrolled in a medical school whose ages were from 18 to 25 between March and December 2020 in China. A stratified whole-group sampling method was used to draw an equal proportional sample of 1183 students from 26 majors in 5 grades, including clinical medicine, nursing, bioengineering, medical imaging, pharmacy, stomatology, anesthesiology, medical laboratory science, psychiatry, and other medical and social related majors such as communication, musicology, psychology, information management, and information system.
Inclusion criteria included students who enrolled in a medical school and students who voluntarily completed the questionnaire. Exclusion criteria were part-time students, master’s degree students, and adult education students.
Questionnaire
The questionnaire consisted of four parts: a general demographic characteristics questionnaire, a 14-item medication literacy scale, a 14-item health literacy scale (HLS-14), and a medication behavior scale.
General Demographic Characteristics Questionnaire
The general demographic characteristics included the basic information of the respondents such as age, gender, profession, place of birth, and parent’s education level.
Medication Literacy Scale
The medication literacy scale is a self-made scale modeled on HLS-14, intended to comprehensively evaluate the medication literacy level of college students in three dimensions: functional medication literacy, communicative medication literacy, and critical medication literacy. The scale consists of 14 items and is scored on a 5-point Likert scale with a full score of 70. A score of 56 or above was considered “have medication literacy”, while a score of less than 56 was “not have medication literacy”. At the same time, if the score of a single dimension was greater than or equal to 80% of the total score of that dimension, it was considered “have medication literacy” in that dimension. The higher score indicates a higher medication literacy level.
In this study, Cronbach’s alpha coefficient for the medication literacy scale was 0.830 ( > 0.8), showing good reliability. All entries were supported by references, and 13 experts in medicine were invited to assess the content validity of the scale (14). The scale entries were subsequently adjusted and modified according to the purpose of the study, and the scale had good content validity. The Kaiser-Meyer-Olkin value of the exploratory factor analysis was 0.877 ( > 0.8), and the P value of Bartlett’s sphericity test was < 0.001. The factors corresponding to the questions were consistent with the expected assumptions, the factor loading coefficients of all items were greater than 0.69, and the cumulative variance explained by the factors was 67.614% ( > 60%).
Health Literacy Scale
This study used the Chinese version of the HLS-14 with 3 dimensions and 14 entries (15,16). The scale is based on a 5-point Likert scale with a score of 70 and is scored similarly to the medication literacy scale. The scale has a high internal consistency (Cronbach’s α coefficient of 0.891). The mean content validity index of the scale was 0.965, the confirmatory factor analysis was 0.976, the goodness of fit index was 0.953, the root-mean-square deviation was 0.059, and the model was acceptable. This scale is widely used in health literacy-related studies and enjoys good reliability and validity (17,18).
Self-administered Medication Behavior Scale
The medication behavior scale consists of 5 items with no dimensions and adopts a 5-point Likert scale, with a score greater than or equal to 20 (80% of the total score) considered “good medication behavior”; otherwise, it is considered “poor medication behavior”.
In this study, Cronbach’s α coefficient of the scale was 0.887 ( > 0.8), suggesting good reliability. The scale was developed based on a large amount of literature (9,19-23), and 13 experts in medicine were invited to assess the scale’s content validity. Subsequently, the scale entries were adjusted and modified according to the purpose of the study, and the scale had good content validity.
Quality Control
The investigators were uniformly trained before the formal distribution of the questionnaires, and the questionnaires were distributed following the principles of scientific research design and statistical requirements to control possible bias during data collection. They were logically checked, and data were screened after recovery to fully ensure data quality. The exclusion criteria for invalid questionnaires were a filling time of less than 100 seconds, incomplete information, logical inconsistencies in the filled questionnaires, and duplicate questionnaires.
Statistical Methods
SPSS 25.0 software was used for statistical analysis. Frequency and proportion were used to describe the characteristics of demographic variables and scale scores. A chi-square test was used for one-way analysis to compare the differences in medication behaviors among students with different characters. The multiple linear regression model was used to exclude multicollinearity with “medication behavior” as the dependent variable, in which “always” was assigned a score of 1, and the other options were assigned a score of 0. After that, a binary logistic regression analysis was performed to test the relationship among medication literacy level, health literacy level, and medication behavior. Then, the bootstrap program was used to test the mediating effect of medication literacy on health literacy and medication use behavior.
Results
Table 1 shows that the respondents’ ages range from 18 to 25, with an average of 19.06 and a male-to-female ratio of about 1:2.4, and most students were in the clinical medicine group (52.4%) in terms of professional distribution. Of the 1183 respondents, only 164 (13.9%) had medication literacy, and 150 (12.7%) had health literacy.
Table 1.
General Demographic Characteristics of College School Students (N = 1183)
|
|
Number
|
Percent
|
| Gender |
1183 |
|
| Male |
347 |
29.3% |
| Female |
836 |
70.7% |
| Specialties |
1183 |
|
| Nursing |
233 |
19.7% |
| Clinical Medicine |
648 |
54.8% |
| Pharmacy |
75 |
6.3% |
| Other |
227 |
19.2% |
| Grade |
1183 |
|
| Freshman year |
459 |
38.8% |
| Sophomore |
330 |
27.9% |
| Junior and above |
394 |
33.3% |
| Place of origin |
1183 |
|
| Cities and towns |
471 |
39.8% |
| Rural |
712 |
60.2% |
| Father’s education level |
1183 |
|
| Secondary school and above |
499 |
42.2% |
| Junior high school and below |
684 |
57.8% |
| Mother’s education level |
1183 |
|
| Secondary school and above |
408 |
34.5% |
| Junior high school and below |
775 |
65.5% |
| Self-assessment of health status |
1183 |
|
| Below 8 points (poor or fair) |
450 |
38.0% |
| 8 points and above (good) |
733 |
62.0% |
| Self-assessment of academic achievement |
1183 |
|
| Less than 8 points (poorer) |
840 |
71.0% |
| 8 points and above (good) |
343 |
29.0% |
Table 2 depicts that lower grades, higher health literacy levels, and higher medication literacy levels were effective in better performance on medication use behavior (P < 0.001). Poor self-assessment health status was correlated to worse medication behavior (P < 0.05), and the collinear diagnosis results indicated no multicollinearity between medical use behavior determinants in Table 2.
Table 2.
The Comparison of Medication Use Behaviors of Students by Sociodemographic Characteristics
|
Item
|
Medication Behavior
|
|
Good, No. (%)
|
OR
|
95% Cl
|
| Grades |
|
|
|
| Freshmen year (control group) |
94 (20.5) |
|
|
| Sophomore year |
129 (39.1) |
0.766 |
(0.514, 1.41) |
| Junior year and above |
151 (38.3) |
0.419** |
(0.274, 0.639) |
| Father's education level |
|
|
|
| Junior high school and below (control group) |
261 (38.2) |
|
|
| Technical secondary school and above |
236 (47.3) |
0.917 |
(0.607, 1.386) |
| Mother's education level |
|
|
|
| Junior high school and below (control group) |
303 (39.1) |
|
|
| Technical secondary school and above |
194 (47.5) |
1.236 |
(0.81, 1.887) |
| Self-assessment of health status |
|
|
|
| Less than 8 points (poor or fair) (control group) |
146 (32.4) |
|
|
| 8 points and above (good) |
351 (47.9) |
1.472* |
(1.014, 2.138) |
| Self-assessment of academic achievement |
|
|
|
| Less than 8 points (poor or fair) (control group) |
330 (39.3) |
|
|
| 8 points and above (good) |
167 (48.7) |
1.133 |
(0.784, 1.638) |
| Medication literacy |
|
|
|
| Have no medication literacy (control group) |
114 (11.2) |
|
|
| Have medication literacy |
73 (44.5) |
4.52** |
(2.735, 7.47) |
| Health literacy |
|
|
|
| Have no health literacy (control group) |
125 (12.1) |
|
|
| Have health literacy |
62 (41.3) |
1.837* |
(1.082, 3.118) |
Note. OR: Odds ratio; CI: Confidence interval;*P < 0.05; **P < 0.001.
Table 3 illustrates that in the Model 1 test, health literacy had a significant influence on medication use behavior (β = 0.084, P < 0.001), indicating that the total effect was valid. In Model 2, health literacy had a significant effect on medication literacy (β = 0.848, P < 0.001), while in model 3, health literacy had a significant effect on medication use behavior (β = 0.052, P < 0.001), and medication literacy had a significant effect on medication use behavior (β = 0.037, P < 0.001). Therefore, the mediating effect of medication literacy in the model is valid and incomplete in Figure 1.
Table 3.
Direct and Indirect Effects of Health Literacy, Medication Literacy, and Medication Use Behavior
|
Model
|
Dependent Variable
|
Independent Variable
|
R
|
R-Squared
|
F
|
β
|
t
|
| Model 1 |
Medication use behavior |
Health literacy |
0.325 |
0.106 |
139.594 |
0.084 |
11.815*** |
| Model 2 |
Medication literacy |
Health literacy |
0.788 |
0.620 |
1929.223 |
0.848 |
43.923*** |
| Model 3 |
Medication use behavior |
Health literacy |
0.339 |
0.115 |
76.527 |
0.052 |
4.570*** |
| Medication literacy |
0.037 |
3.485*** |
Note.
*
P < 0.05; **P < 0.01; ***P < 0.001.
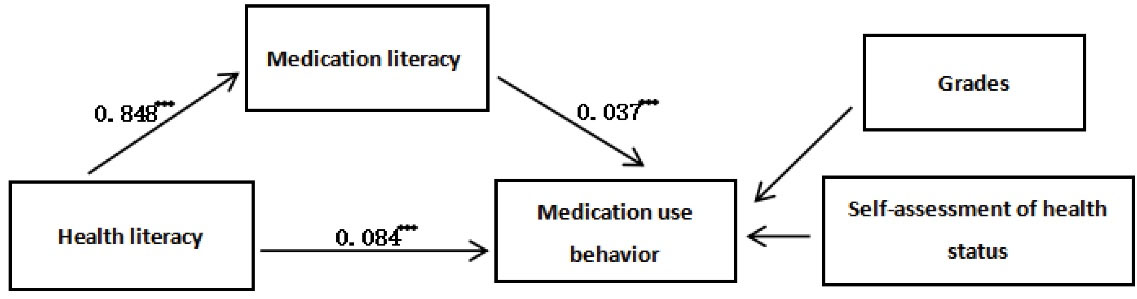
Figure 1.
The Relationship among Health Literacy, Medication Literacy, and Medication Use Behavior
.
The Relationship among Health Literacy, Medication Literacy, and Medication Use Behavior
Table 4 shows that the indirect effect value was 0.031 (P < 0.001); therefore, medication literacy played a significant mediating role in the model. Moreover, the direct effect value was 0.052 (P < 0.001), indicating that the direct effect is valid. Additionally, the proportion of responsibility for medication literacy is 38%.
Table 4.
Bootstrap Mediation Effect Analysis of the Relationship between Health Literacy and Medication Behavior
|
Effect
|
Effect Value
|
LLCI
|
ULCI
|
Ratio
|
| Total effect |
0.084 |
0.070 |
0.098 |
|
| Direct effect |
0.052 |
0.030 |
0.075 |
62% |
| Indirect effect |
0.031 |
0.012 |
0.050 |
38% |
Note. LLCI: Lower limit confidence interval; ULCI: Upper limit confidence interval.
Discussion
Health literacy and medication literacy influenced medication behavior, and the influence is diversified. It is not only reflected in medication knowledge reserve and comprehension, medication advice, service acquisition, and medication compliance but also is closely related to students’ health awareness and health standards. Medication literacy might be an intermediate variable linking health literacy and medication use behavior. Further, medication environment and education played an important role in guiding children’s medication behavior. In this section, we explored this potential relationship in depth and discussed implications for medication education. Finally, we summarized the highlights and limitations of the study to provide references for follow-up research.
Understanding disease and medication information correctly is a prerequisite for effective medication treatment (24). A study in South Korea found that health literacy is positively associated with reading drug labels and accurately understanding prescription instructions (25). Inadequate or biased understanding of medication information, labeling information, and precautions led patients to take medications incorrectly and created potential risks (26,27). Health literacy was also significantly associated with the amount of medication knowledge acquired (28). Therefore, health literacy level impacted medication behavior not only in terms of medication use, access to and understanding of medication information but also regarding medication storage and a dozen of other aspects. Patients with high medication literacy levels are more aware of how to use medications and the consequences of not taking medications as prescribed, so they can use medications proficiently, take them on time, and maintain good medication habits over time (5). Medication literacy is a manifestation of health literacy in medication behavior and is more precisely and closely related to medication behavior, so in a sense, medication literacy has a more direct and profound impact on medication behavior than health literacy. It may suggest that the development of medication literacy education is more relevant and timely to improving students’ medication behaviors.
However, it is not advisable to completely replace health literacy with medication literacy to predict medication use behavior. The results of pathway analysis showed that although health literacy could indirectly affect medication use behavior by influencing medication literacy, the mediating effect of medication literacy was incomplete, and the indirect effect was not as significant as the direct effect. Therefore, both health literacy and medication literacy play an irreplaceable role in medication use behavior.
College students with higher medication literacy and health literacy had more complete medicine knowledge, fuller awareness of safe medication use, and better medication use habits. Thus, they are more likely to make appropriate medication decisions and adhere to healthy behaviors. Students who lack health literacy have limited ability to understand medical and health information and communicate effectively with healthcare professionals; furthermore, they have insufficient knowledge about diseases and medications, leading to decreased medication compliance (29).
Health education in schools is fundamental to fostering health literacy among citizens (30,31). Both insufficient medication literacy and health literacy in school students and the subjective demand for health information suggest the urgent need for health education (12,32-34). Moreover, health education oriented toward improving health literacy and medication literacy will better meet the needs of college students, which was applied to medication education in Taiwan and proved to be effective (35).
The target of the present study is medical school students. Even after receiving education regarding professional knowledge and skills, there are still non-standard medication behaviors. On certain items, juniors and seniors performed even worse than freshmen, which illustrates that the essence of health literacy is a kind of ability, and its formation and enhancement will be a long-term process. Health education should be carried out to disseminate knowledge and skills and promote the transformation from information to action (34). It suggests that we should not only transmit knowledge but also foster students’ ability to communicate and think rationally and discursively to make correct decisions while carrying out health science and advocacy work (36).
The innovation of this study is the selection of the research population and the research perspective. The subjects of this study are medical school students. As a population with easy access to health information, their medication literacy level, health literacy level, and medication behavior can represent the level of the college student population to some extent, that is, the sample has good activeness (37). In terms of innovations from a research perspective, we investigated medication use behaviors in general, not just for a specific drug, to avoid the influence of drug specificity on the study results. For the study content, we included health literacy and medication literacy as independent variables and discussed their correlations with medication use behaviors to further explore their impact on implementing and evaluating safe medication education.
At the same time, there are some limitations to this study. First, the nature of the cross-sectional survey limits the analysis of the effects of medication behavior interventions. Second, since the innovation of the questionnaire places a greater emphasis on the subjectivity of the place of response, there are differences in the individual’s understanding of the questions. Third, the sample’s representativeness is still questionable due to its single source.
Conclusion
The findings of this study revealed that grade, self-rated health status, health literacy, and medication literacy all significantly affected the medication use behavior of students. Further, medication literacy might be an intermediate variable linking health literacy and medication use behavior. Despite receiving more professional education and training, irrational medication use behaviors were common among medical school students. Health literacy and medication literacy, especially the latter, can be considered important contents of medication safety education for college students. It can also serve as an effective indicator to measure educational outcomes and progress.
Acknowledgments
The authors would like to thank all the students who participated in the study.
Authors’ Contribution
Conceptualization: Yibo Wu, Xinying Sun.
Formal analysis: Chengyu An.
Funding acquisition: Yibo Wu.
Methodology: Yibo Wu, Xinying Sun.
Project administration: Yibo Wu, Yujia Wang.
Investigation: Ruyi Hou.
Visualization: Chengyu An, Jingbo Zhang.
Writing-original draft: Chengyu An, Xincheng Huang.
Writing-review, & editing: Chengyu An, Yujia Wang, Bojunhao Feng, Jingbo Zhang, Ruyi Hou, Xincheng Huang, Zhu Zhu, Xinying Sun, Yibo Wu.
Competing Interests
The authors have no conflict of interests associated with the material presented in this paper.
Ethical Approval
The study was approved by the Medical Ethics Committee of Key Research Base of Philosophy and Social Sciences in Shaanxi Province, Health Culture Research Center of Shaanxi (ID: JKWH-2020-01) and was conducted according to the guidelines of the Declaration of Helsinki. All participants participated in the study voluntarily and filled out the informed consent ethics approval.
Funding
The authors received financial support for research from the Annual Project of Shaanxi Provincial Social Science Foundation in 2022 (Grant: 2022M020).
References
- Frings D, Sykes S, Ojo A, Rowlands G, Trasolini A, Dadaczynski K. Differences in digital health literacy and future anxiety between health care and other university students in England during the COVID-19 pandemic. BMC Public Health 2022; 22(1):658. doi: 10.1186/s12889-022-13087-y [Crossref] [ Google Scholar]
- DeWalt DA, Broucksou KA, Hawk V, Brach C, Hink A, Rudd R. Developing and testing the health literacy universal precautions toolkit. Nurs Outlook 2011; 59(2):85-94. doi: 10.1016/j.outlook.2010.12.002 [Crossref] [ Google Scholar]
- King SR, McCaffrey DJ, Bouldin AS. Health literacy in the pharmacy setting: defining pharmacotherapy literacy. Pharm Pract (Granada) 2011; 9(4):213-20. doi: 10.4321/s1886-36552011000400006 [Crossref] [ Google Scholar]
- O’Connor S, McCaffrey N, Whyte E, Moran K, Lacey P. Nonsteroidal anti-inflammatory drug use, knowledge, and behaviors around their use and misuse in Irish collegiate student-athletes. Phys Sportsmed 2019; 47(3):318-22. doi: 10.1080/00913847.2018.1553468 [Crossref] [ Google Scholar]
- Miller MJ, Nutbeam D. Advancing international understanding of health literacy in pharmacy: current trends and future directions. Res Social Adm Pharm 2018; 14(9):v-vi. doi: 10.1016/j.sapharm.2018.07.018 [Crossref] [ Google Scholar]
- Zhang NJ, Terry A, McHorney CA. Impact of health literacy on medication adherence: a systematic review and meta-analysis. Ann Pharmacother 2014; 48(6):741-51. doi: 10.1177/1060028014526562 [Crossref] [ Google Scholar]
- Rothman RL, Yin HS, Mulvaney S, Co JP, Homer C, Lannon C. Health literacy and quality: focus on chronic illness care and patient safety. Pediatrics 2009; 124 Suppl 3:S315-26. doi: 10.1542/peds.2009-1163H [Crossref] [ Google Scholar]
- Visscher BBB, Steunenberg BB, Zwikker HH, Heerdink ERR, Rademakers JJ. The impact of health literacy on beliefs about medication in a Dutch medication-using population. Eur J Clin Pharmacol 2021; 77(8):1219-24. doi: 10.1007/s00228-021-03105-0 [Crossref] [ Google Scholar]
- Zheng F, Ding S, Lai L, Liu X, Duan Y, Shi S. Relationship between medication literacy and medication adherence in inpatients with coronary heart disease in Changsha, China. Front Pharmacol 2019; 10:1537. doi: 10.3389/fphar.2019.01537 [Crossref] [ Google Scholar]
- Shi S, Shen Z, Duan Y, Ding S, Zhong Z. Association between medication literacy and medication adherence among patients with hypertension. Front Pharmacol 2019; 10:822. doi: 10.3389/fphar.2019.00822 [Crossref] [ Google Scholar]
- Wei Y, Chen Y, Zhao Y, Rothman R, Ming J, Wang L. Health literacy and exercise interventions on clinical outcomes in Chinese patients with diabetes: a propensity score-matched comparison. BMJ Open Diabetes Res Care 2020; 8(1):e001179. doi: 10.1136/bmjdrc-2020-001179 [Crossref] [ Google Scholar]
- Goulding E, Murphy M, Di Blasi Z. Sharing and borrowing prescription medication: a survey of Irish college students. Ir J Med Sci 2011; 180(3):687-90. doi: 10.1007/s11845-011-0698-0 [Crossref] [ Google Scholar]
- Smith JM, Mader J, Szeto ACH, Arria AM, Winters KC, Wilkes TCR. Cannabis use for medicinal purposes among Canadian university students. Can J Psychiatry 2019; 64(5):351-5. doi: 10.1177/0706743718818420 [Crossref] [ Google Scholar]
- Cheng JF, Zheng GJ. Investigation on knowledge and behavior of drug safety among college students. Zhejiang Journal of Preventive Medicine 2014; 26(9):962-4. [ Google Scholar]
- Zhang XF, Di HJ, Li XW, Yu H, Liu C, Liu XJ. Functional communication and evaluation of sexual health literacy scale in Chinese and its reliability and validity analysis. Chinese Journal of Modern Nursing 2018; 24(18):2136-40. [ Google Scholar]
- Suka M, Odajima T, Kasai M, Igarashi A, Ishikawa H, Kusama M. The 14-item health literacy scale for Japanese adults (HLS-14). Environ Health Prev Med 2013; 18(5):407-15. doi: 10.1007/s12199-013-0340-z [Crossref] [ Google Scholar]
- Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007; 60(1):34-42. doi: 10.1016/j.jclinepi.2006.03.012 [Crossref] [ Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling 1999; 6(1):1-55. doi: 10.1080/10705519909540118 [Crossref] [ Google Scholar]
- Wu YX, Wang EH, Zhao XJ, Han FX, Zhang JG, Cui L. Knowledge, attitude, and practice of medication among Haikou residents. Ann Palliat Med 2021; 10(6):6883-91. doi: 10.21037/apm-21-1295 [Crossref] [ Google Scholar]
- Yaghoubifard S, Rashidian A, Kebriaeezadeh A, Majdzadeh R, Hosseini SA, Akbari Sari A. Developing a conceptual framework and a tool for measuring access to, and use of, medicines at household level (HH-ATM tool). Public Health 2015; 129(5):444-52. doi: 10.1016/j.puhe.2015.01.026 [Crossref] [ Google Scholar]
- Li X, Qin JX, Wang YN. Investigation and analysis of common sense and behavior of drug use among 9 non-medical college students in Beijing. China Pharmacy 2018; 29(8):1131-5. [ Google Scholar]
- Thapa S, Nielsen JB. Association between health literacy, general psychological factors, and adherence to medical treatment among Danes aged 50-80 years. BMC Geriatr 2021; 21(1):386. doi: 10.1186/s12877-021-02339-y [Crossref] [ Google Scholar]
- James DH, French DP. The development of the Self-Medicating Scale (SMS): a scale to measure people’s beliefs about self-medication. Pharm World Sci 2008; 30(6):794-800. doi: 10.1007/s11096-008-9227-2 [Crossref] [ Google Scholar]
- Li Y, Du LP, Mei D. Health literacy and medication management in patients with chronic noncommunicable diseases. Evaluation and Analysis of Drug-Use in Hospitals of China 2017; 17(6):858-860. [ Google Scholar]
- Song S, Lee SM, Jang S, Lee YJ, Kim NH, Sohn HR. Mediation effects of medication information processing and adherence on association between health literacy and quality of life. BMC Health Serv Res 2017; 17(1):661. doi: 10.1186/s12913-017-2598-0 [Crossref] [ Google Scholar]
- Keller DL, Wright J, Pace HA. Impact of health literacy on health outcomes in ambulatory care patients: a systematic review. Ann Pharmacother 2008; 42(9):1272-81. doi: 10.1345/aph.1L093 [Crossref] [ Google Scholar]
- Brown MT, Bussell JK. Medication adherence: WHO cares?. Mayo Clin Proc 2011; 86(4):304-14. doi: 10.4065/mcp.2010.0575 [Crossref] [ Google Scholar]
- Marks JR, Schectman JM, Groninger H, Plews-Ogan ML. The association of health literacy and socio-demographic factors with medication knowledge. Patient Educ Couns 2010; 78(3):372-6. doi: 10.1016/j.pec.2009.06.017 [Crossref] [ Google Scholar]
- Osborn CY, Paasche-Orlow MK, Davis TC, Wolf MS. Health literacy: an overlooked factor in understanding HIV health disparities. Am J Prev Med 2007; 33(5):374-8. doi: 10.1016/j.amepre.2007.07.022 [Crossref] [ Google Scholar]
- Davis TC, Wolf MS, Bass PF 3rd, Thompson JA, Tilson HH, Neuberger M. Literacy and misunderstanding prescription drug labels. Ann Intern Med 2006; 145(12):887-94. doi: 10.7326/0003-4819-145-12-200612190-00144 [Crossref] [ Google Scholar]
- Zhu Bin. Health literacy of Chinese citizens and integrated utilization of school health education resources. Chinese Journal of School Health 2009; 30(2):161-2. [ Google Scholar]
- Aldousari E, Al-Muomen N. Health information-seeking behavior of students at Kuwait University. International Information & Library Review 2021; 53(4):315-32. doi: 10.1080/10572317.2020.1849913 [Crossref] [ Google Scholar]
- Hsu WC. Undergraduate students’ online health information-seeking behavior during the COVID-19 pandemic. Int J Environ Res Public Health 2021; 18(24):13250. doi: 10.3390/ijerph182413250 [Crossref] [ Google Scholar]
- Zhang D, Zhan W, Zheng C, Zhang J, Huang A, Hu S. Online health information-seeking behaviors and skills of Chinese college students. BMC Public Health 2021; 21(1):736. doi: 10.1186/s12889-021-10801-0 [Crossref] [ Google Scholar]
- Lin LC, Huang CM, Hsu HP, Liao JY, Lin CY, Guo JL. Integrating health literacy into a theory-based drug-use prevention program: a quasi-experimental study among junior high students in Taiwan. BMC Public Health 2021; 21(1):1768. doi: 10.1186/s12889-021-11830-5 [Crossref] [ Google Scholar]
- Yu YH, Yan QY, X J. Research progress on health literacy of Chinese residents. Chinese Journal of Prevention and Control of Chronic Diseases 2021; 29(7):530-4. [ Google Scholar]
- Wang P, Li Y, Bai J. Cognition, use and education demand of antibiotics among college students in 5 universities in China. Pract Prev Med 2020; 27(8):919-22. [ Google Scholar]