J Educ Community Health. 11(1):57-66.
doi: 10.34172/jech.2702
Review Article
Non-pharmacological Management of Hypertension in Arab Countries: A Scoping Review
Nasir Matani 1  , Intan Idiana Hassan 1, *, AJ Rohana 2, Mohammad Nazzal 3
, Intan Idiana Hassan 1, *, AJ Rohana 2, Mohammad Nazzal 3
Author information:
1School of Health Sciences, Universiti Sains Malaysia16150 Health Campus, Kubang Kerian, Kelantan, Malaysia
2Department of Community Medicine, School of Medical Sciences, Universiti Sains Malaysia16150 Health Campus, Kubang Kerian, Kelantan, Malaysia
3Occupational Therapy Department of Rehabilitation Sciences, Faculty of Applied Medical Sciences, Jordan University of Science and Technology Irbid, Jordan
Abstract
Background: Non-pharmacological interventions, such as healthy dietary approaches and physical activity, have always been a crucial part of hypertension (HTN) control in clinical practice. These non-pharmacological interventions, however, have never been reviewed in the literature of Arab countries. This review has quantified and evaluated non-pharmacological interventional studies conducted in Arab countries until 2023.
Methods: Medline, Web of Science, PubMed, the Cochrane Library, Embase, Science Direct, Scopus, ERIC, ProQuest, Springer, Google Scholar, and CINAHL were explored from database inception until September 2023. Articles of relevance were screened based on their titles and abstracts for selection criteria. Eligible studies were reviewed, and information was retrieved. Jadad scores and the Downs and Black checklist were used to evaluate randomized controlled trials (RCTs) and quasi-experimental studies, respectively.
Results: A total of 12 RCTs and 5 quasi-experimental studies met the selection criteria. The studied interventions were eHealth applications, educational programs, wet cupping, physical exercise, adherence therapy, green tea, lifestyle interventions, dietary approaches to stop HTN, motivational interviewing, and cold hibiscus beverages. The most commonly used outcome measure was blood pressure. Nine studies scored high quality. The low and neutral quality scores were mainly due to loss of blindness, poor reporting of participants’ characteristics, loss of follow-up, and failure to account for potential confounders.
Conclusion: There is a scarcity of HTN non-pharmacological interventional studies, aside from the low or modest quality of nearly 50% of them. Hence, it is recommended that further high-quality interventional studies focus on the areas of dietary approaches (especially DASH), exercise, theory-based education, and behavioral counseling in Arab countries.
Keywords: Hypertension, Interventions, Arabs, Scoping review
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Matani N, Hassan II, Rohana AJ, Nazzal M. Non-pharmacological management of hypertension in Arab countries: a scoping review. J Educ Community Health. 2024; 11(1):57-66. doi:10.34172/jech.2702
Introduction
Hypertension (HTN) is a major health problem that affects people all over the world, with a high prevalence of mortality and morbidity, particularly in low- and middle-income countries (1). Globally, around 1.28 billion individuals aged 30–79 suffer from HTN, the majority of whom (two-thirds) live in low- and middle-income countries (2). Despite the advances and development of antihypertensive medication, the prevalence of HTN complications remains high (1). The most recent American guidelines on HTN management establish a lower blood pressure (BP) cut-off point of 130/80 mm Hg for a diagnosis of HTN. However, the American guidelines do not recommend pharmacological therapy for such individuals; instead, it is specifically stated that lifestyle changes should continuously be implemented at this point (3).
In the literature, non-drug management of HTN usually includes physical activity, dietary restrictions and modifications, weight loss, alcohol intake reduction, smoking cessation, dietary supplements, meditation, stress reduction, adequate sleep patterns, acupuncture, BP home monitoring, behavioral counseling support, and lifestyle change maintenance (3-5).
Literature on HTN management always highlights the importance of lifestyle modification, especially dietary habits. In 1992, the U.S. National Institutes of Health invested a lot of effort to figure out what would be the best dietary pattern to control HTN or decrease BP. A landmark feeding study that compared different types of diets found that one that was high in vegetables and fruits contained reduced-fat dairy products, was lower in saturated fat and overall fat, and had more protein and fiber than the other diets—the dietary approach to stop the HTN “DASH diet”—was the most effective one (6). The Mediterranean diet has also demonstrated effectiveness in lowering BP and the risk of cardiovascular diseases, but less so than the DASH diet (3,7). Exercise has been shown to lower both ambulatory and office BP in individuals with HTN (5,8). Bruno et al (9) concluded that maintaining a healthy body weight or losing weight, limiting alcohol consumption, limiting sodium intake, managing stress, and exercising exhibit efficacy in reducing BP levels in both hypertensive and normotensive people. Self-measured and monitored BP was found effective in reducing BP in hypertensive individuals, either alone or combined with other supportive services, including counseling or education (3,9,10).
Other non-pharmacological strategies have shown positive effects on HTN management, however, indirectly, less effectively, or inconsistently. Despite the plenty of positive health outcomes of smoking cessation in the prevention of cardiovascular and many other diseases, research studies reveal an inconsistent relationship between smoking or smoking cessation and BP readings (9), favoring non-smoking status. Dietary supplements such as garlic, cocoa, potassium salts, and Omega-3 fatty acids were beneficial in reducing BP but with less effectiveness than DASH or regular aerobic exercise (10-12).
It is worth mentioning that most of the literature that tested or reviewed non-pharmacological interventions in managing HTN was conducted in non-Arabic countries and on non-Arabic participants. Considering that changing or modifying lifestyles is influenced by culture, traditions, values, beliefs, and other social aspects, it is necessary to examine these interventions in different people with different cultural backgrounds. Thus, a scoping review is a suitable approach for surveying the existing body of literature pertaining to this particular subject, enabling the identification of research gaps prior to embarking on further investigations or undertaking alternative types of studies such as clinical trials or systematic reviews. The Arab world encompassed 22 developing countries and territories with a total population of 444.81 million in 2021 (13). The countries were Egypt, Bahrain, Oman, Djibouti, Algeria, Iraq, Jordan, Saudi Arabia, Lebanon, Libya, Yemen, Morocco, Comoros, Palestine territory (West Bank and Gaza Strip), Qatar, Kuwait, Somalia, Sudan, the United Arab Emirates, Tunisia, Syria, and Mauritania (Figure 1). Despite socioeconomic variations, Arab states exhibit linguistic, cultural, and religious similarities that greatly influence the development and execution of population-based health promotion and preventive care initiatives. These approaches are crucial in tackling the morbidity and mortality associated with HTN. Thus, the aim of this scoping review is to search, find, quantify, and evaluate interventional studies that have so far been conducted in Arab countries aiming at managing or controlling HTN among Arab populations.
Materials and Methods
Search Strategy
Related data were gathered from Medline, PubMed, Web of Science, Embase, the Cochrane Library, Science Direct, Scopus, ERIC, ProQuest, Springer, CINAHL, and Google Scholar since database inception until September 2023. Search terms included “Non-pharmacological” OR “Non-drug” OR “Behavioral” AND “management” OR “intervention” OR “control” AND “hypertension” OR “hypertensive” OR “Blood pressure” OR “Bahrain” OR “Algeria” OR “Djibouti” OR “Oman” OR “Iraq” OR “Comoros” OR “Jordan” OR “Kuwait”. The other terms were “Lebanon” OR “Egypt” OR “Libya” OR “Mauritania” OR “Palestine” OR “Gaza Strip” OR “West Bank” OR “Morocco” OR “Qatar” OR “Syria” OR “Somalia” OR “Sudan” OR “the United Arab Emirates” OR “Saudi Arabia” OR “Yemen” OR “Tunisia”. The retrieval processes were conducted autonomously by two researchers.
Selection Criteria
After eliminating duplicates, relevant publications were assessed based on their titles and abstracts. Studies were considered suitable for inclusion if they addressed a non-pharmacological intervention for the management of HTN in Arab countries. The remaining studies were subsequently scrutinized in their entirety to verify their eligibility.
The inclusion criteria were being an interventional study (a randomized controlled or quasi-experimental study) reporting a non-pharmacological intervention for the management of HTN, being conducted in an Arab country, and being published in English as an original article. On the other hand, the exclusion criteria included the unavailability of electronic full text, qualitative and observational studies, review papers, comments, letters, editorials, opinions, protocols, and guidelines. In addition, studies reporting a pharmacological intervention for HTN management and studies with inadequate outcome data were excluded from the review. Reference lists were cross-referenced, and related sources also underwent examination.
Data Extraction
Two authors, working independently, collected data from the eligible articles based on the specified criteria for inclusion and exclusion. The acquired information was recorded on a standardized data sheet, which comprised study information (author/s’ names and publication year), research design, country, study population, sample size, age of participants, type of intervention, outcome measure, and findings.
Quality Assessment of Studies
The Jadad score, which evaluates descriptions of randomization, blinding, and dropouts (withdrawals) in trials, was used to evaluate the methodological quality of the included randomized controlled trials (RCTs) (14). The level of quality ranges from 0 to 5, where a report is considered low-quality if it scores 2 or below or high-quality if it scores 3 or higher (15). The potential for bias was investigated for all other quasi-experimental study designs by employing the pertinent criteria from the Downs and Black checklist (16). Based on the ten-item criteria, studies were evaluated and assigned a positive rating if more than 50% of the criteria were satisfied, a neutral rating if exactly 50% of the criteria were met, or a negative rating if fewer than 50% of the criteria were met.
Results
Identification of Studies
The database search yielded 346 studies for screening, out of which 130 abstracts were deemed possibly eligible and subsequently retrieved for a thorough evaluation of the full text. The excluded studies were duplicate studies (n = 92), studies lacking full text (n = 74), not-English studies (n = 50), and papers considered irrelevant and meeting additional exclusion criteria (n = 113). Seventeen papers met the eligibility criteria and were included in this scoping review. The studies were identified according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (17). The flowchart is shown in Figure 2.
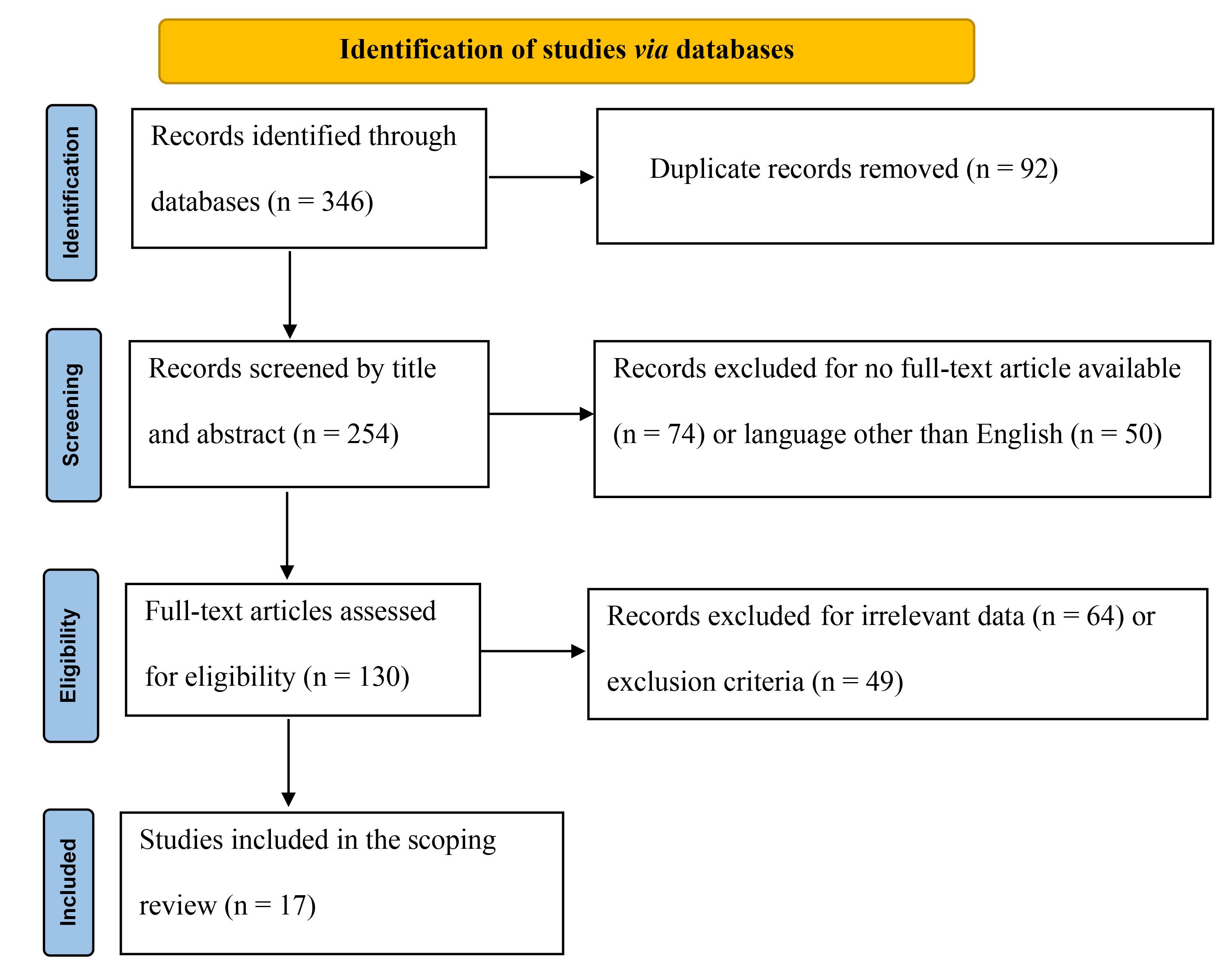
Figure 2.
PRISMA Flowchart of the Eligibility of Interventional Studies Conducted in Arab Countries. Note. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
.
PRISMA Flowchart of the Eligibility of Interventional Studies Conducted in Arab Countries. Note. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Study Characteristics
The reviewed studies (n = 17) were published between 2012 and 2022 and distributed among 7 Arab countries, including Egypt (n = 6), Saudi Arabia (n = 3), Jordan (n = 3), Palestine (n = 2), Tunisia (n = 1), Sudan (n = 1), and Lebanon (n = 1). Among the 17 articles included in this scoping review, 12 were RCTs and 5 were quasi-experimental research. The sample size of the reviewed articles ranged from 18 to 2000 participants. The mean age of participants was > 40 years old. Among the 17 included studies, 11 interventions were investigated, including eHealth applications (n = 4), educational programs (n = 3), wet cupping (n = 3), physical exercise (n = 1), adherence therapy (n = 1), green tea (n = 1), lifestyle interventions (n = 1), DASH (n = 1), motivational interviewing (n = 1), and cold hibiscus beverages (n = 1). The predominant outcome measurements were systolic and diastolic blood pressure (SBP and DBP). The findings demonstrated that all interventions presented a significant improvement in HTN management. The characteristics of the reviewed studies are summarized in Table 1.
Table 1.
Key Attributes of Studies Incorporated in This Scoping Review
|
Study
|
Study Design
|
Country
|
Study Population
|
Sample Size
|
Age (Mean±SD)
|
Type of Intervention
|
Outcome Measure
|
Findings
|
| Abdelaal and Mohamad (18) |
RCT |
Egypt |
Obese diabetic hypertensive patients were randomly assigned to one of three groups, including aerobic exercise training (AET, n = 20), circuit weight training (CWT, n = 20), and control (n = 19). |
59 |
- CWT group: 52.2 ± 3.00
- Aerobic training group: 53.00 ± 3.5
- Control group: 52.00 ± 3.27 |
AET or CWT |
- SBP
- DBP
- BMI
- Waist circumference |
The SBP mean values showed a notable reduction of 3.09 ± 0.69% and 4.79 ± 1.69% in the CWT and AET groups, respectively, after 3 months of training compared to the pre-training period (P < 0.05). The DBP mean values exhibited a notable decline of 2.98 ± 1.07% and 6.02 ± 1.06% in the CWT and AET groups, respectively, after 3 months of training compared to the pre-training period (P < 0.05). |
| Abu-El-Noor et al (19) |
RCT |
Palestine |
Participants with HTN who had been prescribed at least one antihypertensive drug at the time of data collection (n = 97) and the control group (n = 94) |
191 |
- Intervention group: 57.5 ± 11.9
- Control group: 55.4 ± 10.9 |
Mobile phone app |
- Medication adherence
- Diet adherence
- Appointment adherence |
Both the intervention and control groups demonstrated significant improvements in their adherence levels, with the intervention group improving in the total score as well as all three domain scores, including medication adherence, diet adherence, and appointment keeping. |
| Ahmed et al (20) |
QER |
Egypt |
Patients with essential HTN should follow a treatment plan. |
120 |
48.50 ± 7.89 |
Educational program |
- SBP
- DBP
- BMI |
The intervention led to a considerable improvement in patients’ adherence to therapy regimens, as evidenced by a highly statistically significant difference with a P-value of 0.001. |
| Aleyeidi and Aseri (21) |
RCT (pilot study) |
Saudi Arabia |
The intervention group comprised hypertensive patients who underwent three sessions of wet cupping in addition to their regular anti-hypertensive treatment (n = 10), while the control group consisted of hypertensive patients who got only their regular anti-hypertensive treatment (n = 8). |
18 |
- Intervention group: 52 ± 7.2
- Control group: 49 ± 9.5 |
Wet cupping |
- SBP
- DBP
- Adverse events |
There was no statistically significant difference between the intervention and control groups in terms of the mean difference in SBP and DBP. No significant adverse effects of wet cupping were observed in this investigation. |
| Aleyeidi Aseri (22) |
RCT |
Saudi Arabia |
The intervention group (n = 40) received wet cupping in addition to conventional HTN treatment, while the control group (n = 40) received only conventional HTN treatment. |
80 |
- Intervention group: 52.0 ± 9.4
- Control group: 53.8 ± 9.5 |
Wet cupping |
- SBP
- DBP
- Adverse events |
Wet cupping resulted in an immediate decrease in SBP. After 4 weeks of follow-up, the mean SBP of the intervention group was 8.4 mmHg lower than that of the control group (P = 0.046). There were no significant differences in BP levels between the intervention and control groups after 8 weeks. This study found no significant adverse effects associated with wet cupping. |
| Hassan et al (23) |
RCT |
Egypt |
Patients with primary hypertension |
60 |
46.3 ± 4.2 years |
Wet cupping therapy |
- SBP
- DBP |
The treatment group (wet cupping therapy) had significant differences in SBP and DBP compared to the other groups, indicating a favorable outcome. |
| Alhalaiqa et al (24) |
RCT |
Jordan |
Non-adherent hypertensive patients were assigned to either AT (n = 68) or treatment as usual (TAU, n = 68). |
136 |
- AT group: 53.4 ± 10.7
- TAU group: 53.9 ± 11.7 |
AT |
- SBP
- DBP
- Adverse events
- Beliefs about Medicines Questionnaire |
At 11 weeks, AT reduced SBP by −23.11 mmHg (95% CI: −25.85, −20.36) and DBP by −15.18 mmHg (95% CI: −17.55, −12.80). The AT group demonstrated a 37% enhancement in adherence, as measured by pill consumption, in comparison to the TAU group. No notable adverse effects were reported. |
| Alsaqer and Bebis (25) |
RCT |
Jordan |
Participants with HTN were randomly assigned to either the interventional group (public nursing interventions with telehealth application, n = 37), control (telehealth application alone, n = 36), or standard care (n = 37). |
110 |
- Interventional group: 60.37 ± 5.60
- Mobile health applications alone group: 60 ± 6.89
- Standard care group: 61.45 ± 7.36 |
Public nursing interventions with telehealth application |
- SBP
- DBP
- Quality of life
- HTN self-care |
In comparison to the two control groups, the interventional group exhibited a significant decrease in SBP; however, there was no significant difference in DBP. Additionally, the interventional group showed better enhancements in self-care maintenance, monitoring, and confidence. Compared to the usual care group, there was a significant enhancement in role constraints caused by physical health and mental issues, pain, energy/fatigue, emotional well-being, and social functioning in terms of quality of life. |
| Al-Shafei and El‐Gendy (26) |
RCT |
Egypt |
Patients with HTN were randomly assigned to one of two groups: Grp1 (green tea) and Grp2 (hot water). |
200 |
53 ± 4 |
Regular green tea and hot water |
- SBP
- DBP
- Pulse pressure (PP)
- Left ventricular hypertrophy |
Four months of green tea treatment in Grp1, SBP, DBP, and PP had been reduced by 6.6%, DBP by 5.1%, and PP by 9.1%, respectively. However, this effect was not observed at the 4-month follow-up after stopping green tea and hot water consumption. Grp2 demonstrated no significant BP or PP improvement. |
| Al-Wehedy et al (27) |
QER |
Egypt |
The hypertensive individuals were split into two equal groups. The first group, known as the study group, consisted of 42 patients who underwent a lifestyle intervention to manage their BP. The second cohort consisted of 42 patients who were assigned to the control group and received only standard outpatient care. |
84 |
- Study group: 65.64 ± 4.88
- Control group: 65.11 ± 3.97 |
Lifestyle intervention |
- HTN knowledge
- Lifestyle patterns |
The lifestyle intervention program was effective in lowering BP by encouraging the adoption of healthy behaviors. |
| Dwairej and Ahmad (28) |
RCT |
Jordan |
A total of 57 participants with HTN were allocated to the intervention group, where they received an educational application intervention. Meanwhile, 59 participants were assigned to the control group, where they received conventional care. |
116 |
50 ± 6.2 |
Mobile application |
- SBP and DBP
- Self-care
- Self-efficacy
- Knowledge related to HTN |
After 8 weeks of receiving the study intervention, participants in the intervention group showed statistically significant improvements in self-care and knowledge scores compared to participants in the control group. In addition, a greater number of participants in the intervention group represented BP control compared to the control group. |
| Ead and Ali (29) |
QER |
Egypt |
Hypertensive patients were divided into two groups. One received DAS), and the other received DASH and walking exercise (n = 30 in each). |
60 |
- DASH group: 51.10 ± 8.40
- DASH and exercise group: 53.13 ± 7.10 |
Dietary approaches to stop HTN (DASH) |
- SBP
- DBP
- Hypertensive Patients Knowledge, Attitude Structured Questionnaire |
Patients who received DASH and walking exercises had a lower BP than patients who only received DASH. |
| Jarelnape et al (30) |
QER |
Sudan |
Patients with HTN were randomly assigned to either the intervention group (n = 75), who received a health education program about HTN and its management) or the control group (n = 75). |
150 |
- Intervention group: 41.46 ± 14.84
- Control group: 38.75 ± 15.03 |
Health education program about hypertension
and its management |
- Knowledge about HTN disease aspects
- Knowledge about HTN complications
- Knowledge about the HTN dietary program |
Patients’ knowledge of the definition of HTN, signs and symptoms of HTN and hypotension, adherence to drug types of treatment, dietary management, the importance of exercise, and HTN complications improved significantly (P = 0.001). |
| Khadoura et al (31) |
RCT |
Palestine |
A total of 173 participants received standard HTN care, while 182 received standard HTN care plus non-blinded motivational interviewing (MI) sessions for 3 months. |
355 |
- Intervention group: 56.1 ± 10.4
- Control group: 55.3 ± 11.0 |
MI |
- Medication adherence
- SBP
- DBP
- Self-efficacy |
MI is a client-centered approach that improves medication adherence, mean BP, self-efficacy, and intrinsic motivations in hypertensive patients. |
| Sahli et al (32) |
QER |
Tunisia |
Hypertensive patients were randomly allocated to either the intervention group (a community-based intervention program, n = 921) or control (n = 626). At pre-assessment (n = 940/940) and post-assessment (n = 1,001/976), hypertensive patients were randomly assigned to intervention (a community-based intervention program) and control groups. |
2000 |
- Intervention group: 38.22 ± 13.41
- Control group: 39.52 ± 13.84 |
Community-based intervention program |
- SBP
- DBP |
The prevalence of HTN decreased from 37.3% to 33.7% in the intervention group, but it was not significant (P = 0.1). This proportion increased from 31.1% to 33.4% in the control group without a significant difference (P = 0.28). |
| Saleh et al (33) |
RCT |
Lebanon |
The study encompassed a total of sixteen primary health care centers, with eight serving as controls and eight as interventions. These clinics were situated in rural areas and Palestinian refugee camps across Lebanon. Information on patients diagnosed with diabetes and HTN was collected from their medical records during both the pre- and post-intervention periods. The intervention group consisted of 1433 patients, whereas the control group consisted of 926 individuals. |
1547 |
> 40 years |
Mobile health |
- SBP
- DBP |
Based on a bivariate analysis of quality indicators, the intervention group demonstrated a noteworthy improvement in BP control (P = 0.03) and a considerable reduction in mean SBP (P = 0.02). |
| Salman et al (34) |
RCT |
Saudi Arabia |
Adult females who have normal baseline BP were randomly allocated to one of three groups: Cold (n = 100), boiled hibiscus (n = 100), or placebo (n = 100). |
300 |
39.20 ± 8.71 |
Cold hibiscus beverage |
- SBP
- DBP
- Heart rate |
A cold but not boiled hibiscus beverage lowers BP acutely and safely in adult females with normal baseline BP readings, but only for 15 minutes. |
Note. SDL Standard deviation; CI: Confidence interval; MI: Motivational interviewing; BP: Blood pressure; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; BMI: Body mass index; RCT: Randomized controlled trial; QER: Quasi-experimental research.
Quality Assessment of Studies
Eight RCT research reports were judged to be of high quality according to the Jadad scale (with total Jahad scores of 3 and 4 for five and three studies, respectively). However, four RCT studies were judged to be of low quality according to the Jadad scale. The reason for not earning a full-quality score was that the majority of studies were not double-blinded, and consequently, the method of blinding was not described (Table 2).
Table 2.
Quality of Methodology in the Included Research Reports
|
Study
|
Jadad Scores
|
Total Score
|
|
1
|
2
|
3
|
4
|
5
|
|
| Abdelaal and Mohamad (18) |
1 |
1 |
1 |
0 |
1 |
4 |
| Abu-El-Noor et al (19) |
1 |
1 |
0 |
0 |
1 |
3 |
| Aleyeidi, Aseri (22) |
1 |
1 |
0 |
0 |
1 |
3 |
| Aleyeidi and Aseri (21) |
1 |
1 |
0 |
0 |
1 |
3 |
| Hassan et al (23) |
1 |
1 |
0 |
0 |
1 |
3 |
| Alhalaiqa et al (24) |
1 |
1 |
0 |
0 |
1 |
3 |
| Alsaqer and Bebis (25) |
1 |
1 |
0 |
1 |
1 |
4 |
| Al-Shafei and El‐Gendy (26) |
1 |
1 |
0 |
0 |
0 |
2 |
| Dwairej and Ahmad (28) |
1 |
1 |
0 |
0 |
0 |
2 |
| Khadoura et al (31) |
1 |
1 |
0 |
0 |
0 |
2 |
| Saleh et al (33) |
1 |
1 |
0 |
0 |
0 |
2 |
| Salman et al (34) |
1 |
1 |
1 |
1 |
0 |
4 |
Jadad scale (14) items assess each RCT for randomization, methods of randomization, double-blinding, method of blinding, and a description of dropouts and withdrawals.
Concerning the quasi-experimental research, four studies were deemed to have a neutral rating, while one study earned a positive rating in the assessment of bias risk. Unclear reporting made it difficult to determine whether the criteria were fulfilled in certain cases. More precisely, all the studies did not mention if the coders were kept unaware of the assessment time point, provided no details about the participants’ characteristics, had missing follow-up data, and considered no possible factors that could influence the results. In addition, the analyses did not account for variations in the duration of follow-up among participants. Conversely, all five investigations indicated that the subjects were selected from an identical population simultaneously. Furthermore, the statistical tests employed to evaluate the primary outcomes were suitable, adherence to the intervention(s) was consistent, and the applied key outcome measures were precise. However, only one study considered the patients who were no longer available for further observation (Table 3).
Table 3.
Quality Assessment of Quasi-experimental Studies
|
Study
|
Downs and Black Checklist
|
Rating
|
|
1
|
2
|
3
|
4
|
5
|
6
|
7
|
8
|
9
|
10
|
| Ahmed et al (20) |
0 |
0 |
0 |
1 |
1 |
1 |
1 |
1 |
0 |
0 |
Neutral |
| Al-Wehedy et al (27) |
0 |
0 |
0 |
1 |
1 |
1 |
1 |
1 |
0 |
0 |
Neutral |
| Ead and Ali (29) |
0 |
0 |
0 |
1 |
1 |
1 |
1 |
1 |
0 |
1 |
Positive |
| Jarelnape et al (30) |
0 |
0 |
0 |
1 |
1 |
1 |
1 |
1 |
0 |
0 |
Neutral |
| Sahli et al (32) |
0 |
0 |
0 |
1 |
1 |
1 |
1 |
1 |
0 |
0 |
Neutral |
The risk of bias items from the Downs and Black checklist (16) evaluate each research report for blinding, description of participants who were lost to follow-up, adjustment of analysis based on the length of follow-up, appropriateness of statistical tests employed, and reliability of the intervention component. The other criteria were validity and reliability of the primary outcome measurement, recruitment of participants from the same population, timing of participants’ recruitment, adjustment analysis of the main findings for confounding factors, and the number of participants who lost to follow-up.
Discussion
Given the high prevalence of HTN in middle- and low-income countries, including Arab countries, one would anticipate these countries to invest relatively in HTN management research, resulting in better HTN control outcomes. Such studies, however, have been limited, and HTN control is found to be extremely low (7.7%) in middle- and low-income countries (35,36). For example, even dietary descriptive research studies, as an essential part of HTN management, were found to be extremely limited, and only 7 studies (with varied quality) were counted in a scoping review (37) in the Gulf Cooperation Council countries—six countries— over 10 years (2009–2010). Furthermore, although the DASH diet has been extensively studied and examined in relation to BP control worldwide since the diet’s inception, this current review could retrieve only one study (29) performed in the Arab world. Similarly, only two research studies (18,23) examined the effect of exercise on HTN in the Arab world, despite the huge amount of exercise-related literature existing worldwide.
A higher proportion of the research studies retrieved for this review (25%) examined the use of eHealth strategies for managing HTN. eHealth is defined as an affordable and safe application of technology for communication and information in support of health-related services and other fields (38). Three of these studies used mobile applications, either newly developed for the purpose of the study (19,28) or already previously developed and freely downloaded for the use of the study (25). Saleh et al (33) utilized a telecommunications company to deliver SMS messages to the participants’ mobiles. Although discussed separately, these studies used mainly health education strategies in managing HTN using telecommunications. The most common topics included in these studies were HTN disease, diet, physical activity, BP monitoring, and treatment compliance. Counseling was also part of the intervention in one study using phone calls for communication (25). Three studies could reveal significant BP control by comparing BP measurements pre- and post-intervention. While one study (19) reported significant changes in adherence to medication, diet, and appointments among participants, BP was not an outcome measure. No doubt, health education is beneficial and should always be part of HTN management. However, interventions that combine health education, counseling, and management methods could be more effective (39). Moreover, health education and counseling should include theory- and evidence-based interventions that have been shown to be effective behavioral changes among people (40), which was not obvious or clearly determined in the aforementioned studies; in addition, two (50%) studies were rated as low quality. Similarly, Ahmed et al (20) and Jarelnape et al (30), in their studies, which are rated neutral quality, reported significant BP control among hypertensive patients after providing an educational program; however, the content of the education was not emphasized or elaborated in the report (20), and BP measurement was not an outcome (30). In contrast, Alhalaiqa et al (24) provided counseling therapy sessions called “adherence therapy” (AT), which is rooted in evidence-based practices of cognitive behavioral therapy and MI randomized trials (41). Seven sessions of AT in this high-quality study could lower systolic and diastolic BP significantly. Moreover, Khadoura (31) used MI counseling to increase medication adherence among Palestinian hypertensive patients. The results showed that MI was effective in improving medication adherence and could lower BP significantly.
Noticeably, five (29.45%) of the retrieved studies in this review examined the effect of home remedies or folk practices on BP. Three studies investigated the impact of wet cupping on BP. Wet cupping—called Hijama in Arabic—is a highly common folk practice worldwide, including in Arab countries, and has been used to treat many health problems, especially those associated with pain (42). It showed no specific or significant effect on lowering BP (21-23). Despite the promising health effects (especially musculoskeletal symptoms) of wet cupping (43), no evidence has been found regarding its effect on HTN (44). The other two studies examined the effect of green tea (26,34) and hibiscus drinks (34) on BP. The results were significant; consumption of green tea and cold hibiscus was effective in lowering both SBP and DBP. In accordance with these results, recent systematic reviews and meta-analyses (45,46) confirmed the effect of green tea on lowering BP; however, longer and larger trials were recommended to draw clear evidence. In contrast, a more recent systematic analysis and meta-analysis could not observe this effect on SBP but on DBP (47). Hibiscus drinks were also found to have antihypertensive effects similar to drugs (48,49); however, it is recommended that further studies be conducted to determine the dosages and duration of consumption (49).
Community-based interventions, including education and health promotion, revealed improvements in BP control (50,51). Sahli et al (32) reported the impact of a 3-year community-based intervention project on decreasing the prevalence of elevated BP among adults in Tunisian neighborhoods. The intervention included health education and promotion in dietary practice, physical activity, and smoking prevention. Although there was no substantial difference in the prevalence of HTN between the intervention and control groups, a remarkable reduction in BP was noted in the intervention group. The results might support targeting hypertensive patients with such interventions. Similarly, lifestyle modification interventions were effective in decreasing the BP among hypertensive patients attending medical hospital clinics in Egypt (27), in addition to improving their health promotion profiles. However, the report did not provide details on the program components and framework.
There is strong evidence supporting the adoption of the dietary approach to stop HTN (DASH) and exercise in preventing, managing, and controlling HTN (8,52-54). Ead and Ali (29) examined the effect of DASH and walking exercises on BP in Egyptian participants with HTN. They compared DASH alone with DASH and exercise for BP. DASH alone could lower BP; however, DASH and exercise had a significant antihypertensive effect. Abdelaal and Mohamad (18) studied and compared the impact of aerobic exercise and circuit weight training on the BP of obese Egyptians with HTN. Both types of exercise were effective in BP and weight control; however, aerobic exercise showed a significantly higher positive effect. Even when Hassan et al (23) reported that wet cupping combined with aerobic exercise could lower BP, readers can easily recognize that the reduced BP was mainly due to exercise rather than wet cupping.
Conclusion
Considering that the goal of scoping reviews is to provide breadth rather than depth of information on a specific topic, they have inherent limitations. As a result, this scoping review did not include a meta-analysis that usually assesses the strength of evidence present in a disease or treatment. Moreover, the included studies were limited to ones that were published in English. Finally, the authors of this scoping review acknowledge their efforts in studying and investigating non-drug interventions and their effects on HTN control in Arab countries. The interventions that encompassed health education and behavioral counseling, dietary modification, physical activity, medication adherence, and HTN management showed significant effects on lowering BP and controlling HTN. Other interventions, such as hibiscus tea consumption, demonstrated promising findings. However, this review obviously revealed scarcity in these studies, aside from the low or modest (neutral) quality of nearly 50% of them. Therefore, further high-quality interventional research projects and updated studies are recommended in the areas of dietary approaches (especially DASH), exercise, theory-based education, and behavioral counseling in Arab countries and among Arab people. Researchers are encouraged to conduct more studies on home remedies that are common and highly believed by Arab people to have a positive effect on BP, such as hibiscus tea and garlic consumption (55,56), for further evidence and valid findings.
Authors’ Contribution
Conceptualization: Nasir Matani.
Data curation: Nasir Matani, Mohammad Nazzal.
Formal analysis: Nasir Matani, Mohammad Nazzal.
Investigation: Nasir Matani, Mohammad Nazzal.
Methodology: Nasir Matani, Mohammad Nazzal.
Supervision: Intan Idiana Hassan, AJ Rohana.
Validation: Intan Idiana Hassan, AJ Rohana.
Writing–original draft: Nasir Matani.
Writing–review & editing: Intan Idiana Hassan, AJ Rohana, Mohammad Nazzal.
Competing Interests
None.
Ethical Approval
This scoping review is registered in Open Science Framework registries with the same title under DOI: https://doi.org/10.17605/OSF.IO/RFSTQ.
Funding
No external funding.
References
- Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol 2020; 16(4):223-37. doi: 10.1038/s41581-019-0244-2 [Crossref] [ Google Scholar]
- World Health Organization (WHO). Hypertension. 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/hypertension.
- Verma N, Rastogi S, Chia YC, Siddique S, Turana Y, Cheng HM. Non-pharmacological management of hypertension. J Clin Hypertens (Greenwich) 2021; 23(7):1275-83. doi: 10.1111/jch.14236 [Crossref] [ Google Scholar]
- Mahmood S, Shah KU, Khan TM, Nawaz S, Rashid H, Baqar SWA. Non-pharmacological management of hypertension: in the light of current research. Ir J Med Sci 2019; 188(2):437-52. doi: 10.1007/s11845-018-1889-8 [Crossref] [ Google Scholar]
- Valenzuela PL, Carrera-Bastos P, Gálvez BG, Ruiz-Hurtado G, Ordovas JM, Ruilope LM. Lifestyle interventions for the prevention and treatment of hypertension. Nat Rev Cardiol 2021; 18(4):251-75. doi: 10.1038/s41569-020-00437-9 [Crossref] [ Google Scholar]
- Steinberg D, Bennett GG, Svetkey L. The DASH diet, 20 years later. JAMA 2017; 317(15):1529-30. doi: 10.1001/jama.2017.1628 [Crossref] [ Google Scholar]
- Cowell OR, Mistry N, Deighton K, Matu J, Griffiths A, Minihane AM. Effects of a Mediterranean diet on blood pressure: a systematic review and meta-analysis of randomized controlled trials and observational studies. J Hypertens Suppl 2021; 39(4):729-39. doi: 10.1097/hjh.0000000000002667 [Crossref] [ Google Scholar]
- Saco-Ledo G, Valenzuela PL, Ruiz-Hurtado G, Ruilope LM, Lucia A. Exercise reduces ambulatory blood pressure in patients with hypertension: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc 2020; 9(24):e018487. doi: 10.1161/jaha.120.018487 [Crossref] [ Google Scholar]
- Bruno CM, Amaradio MD, Pricoco G, Marino E, Bruno F. Lifestyle and hypertension: an evidence-based review. J Hypertens Manag 2018; 4(1):1-10. doi: 10.23937/2474-3690/1510030 [Crossref] [ Google Scholar]
- Oza R, Garcellano M. Nonpharmacologic management of hypertension: what works?. Am Fam Physician 2015; 91(11):772-6. [ Google Scholar]
- Fu J, Liu Y, Zhang L, Zhou L, Li D, Quan H. Nonpharmacologic interventions for reducing blood pressure in adults with prehypertension to established hypertension. J Am Heart Assoc 2020; 9(19):e016804. doi: 10.1161/jaha.120.016804 [Crossref] [ Google Scholar]
- Zhang X, Ritonja JA, Zhou N, Chen BE, Li X. Omega-3 polyunsaturated fatty acids intake and blood pressure: a dose-response meta-analysis of randomized controlled trials. J Am Heart Assoc 2022; 11(11):e025071. doi: 10.1161/jaha.121.025071 [Crossref] [ Google Scholar]
- Arab Developmental Portal. Demography. 2021. Available from: https://www.arabdevelopmentportal.com/indicator/demography.
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary?. Control Clin Trials 1996; 17(1):1-12. doi: 10.1016/0197-2456(95)00134-4 [Crossref] [ Google Scholar]
- Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses?. Lancet 1998; 352(9128):609-13. doi: 10.1016/s0140-6736(98)01085-x [Crossref] [ Google Scholar]
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998; 52(6):377-84. doi: 10.1136/jech.52.6.377 [Crossref] [ Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 2009; 151(4):W65-94. doi: 10.7326/0003-4819-151-4-200908180-00136 [Crossref] [ Google Scholar]
- Abdelaal AA, Mohamad MA. Obesity indices and haemodynamic response to exercise in obese diabetic hypertensive patients: randomized controlled trial. Obes Res Clin Pract 2015; 9(5):475-86. doi: 10.1016/j.orcp.2014.11.001 [Crossref] [ Google Scholar]
- Abu-El-Noor NI, Aljeesh YI, Bottcher B, Abu-El-Noor MK. Impact of a mobile phone app on adherence to treatment regimens among hypertensive patients: a randomised clinical trial study. Eur J Cardiovasc Nurs 2021; 20(5):428-35. doi: 10.1177/1474515120938235 [Crossref] [ Google Scholar]
- Ahmed BI, Taha NM, Ali EE, Abd El-Razi BG. Effect of an educational program on compliance of patients with essential hypertension toward therapeutic regimen. Zagazig Nurs J 2017; 13(1):84-101. doi: 10.21608/znj.2017.38266 [Crossref] [ Google Scholar]
- Aleyeidi N, Aseri K. The efficacy of wet cupping on blood pressure among hypertension patients in Jeddah, Saudi Arabia: a randomized controlled trial pilot study. Altern Integr Med 2015; 4(1):183. doi: 10.4172/2327-5162.1000183 [Crossref] [ Google Scholar]
- Aleyeidi NA, Aseri KS, Matbouli SM, Sulaiamani AA, Kobeisy SA. Effects of wet-cupping on blood pressure in hypertensive patients: a randomized controlled trial. J Integr Med 2015; 13(6):391-399. doi: 10.1016/S2095-4964(15)60197-2 [Crossref] [ Google Scholar]
- Hassan AM, Kamel SM, Torad A, Hazzaa A, Salama AM. Effect of wet cupping therapy on reducing blood pressure in primary hypertensive patients: a preliminary study. SVU Int J Med Sci 2023; 6(1):476-83. doi: 10.21608/svuijm.2022.175851.1453 [Crossref] [ Google Scholar]
- Alhalaiqa F, Deane KH, Nawafleh AH, Clark A, Gray R. Adherence therapy for medication non-compliant patients with hypertension: a randomised controlled trial. J Hum Hypertens 2012; 26(2):117-26. doi: 10.1038/jhh.2010.133 [Crossref] [ Google Scholar]
- Alsaqer K, Bebis H. Self-care of hypertension of older adults during COVID-19 lockdown period: a randomized controlled trial. Clin Hypertens 2022; 28(1):21. doi: 10.1186/s40885-022-00204-7 [Crossref] [ Google Scholar]
- Al-Shafei AIM, El-Gendy OAA. Regular consumption of green tea improves pulse pressure and induces regression of left ventricular hypertrophy in hypertensive patients. Physiol Rep 2019; 7(6):e14030. doi: 10.14814/phy2.14030 [Crossref] [ Google Scholar]
- Al-Wehedy A, Abd Elhameed SH, Abd El-Hameed D. Effect of lifestyle intervention program on controlling hypertension among older adults. J Educ Pract 2014; 5(5):61-71. [ Google Scholar]
- Dwairej L, Ahmad M. Hypertension and mobile application for self-care, self-efficacy and related knowledge. Health Educ Res 2022; 37(3):199-212. doi: 10.1093/her/cyac012 [Crossref] [ Google Scholar]
- Ead AY, Ali GA. Effect of diet and walking exercise on blood pressure in hypertensive patients. Int J Novel Res Healthc Nurs 2020; 7(1):347-60. [ Google Scholar]
- Jarelnape AA, Abdullah NT, Yousif KI, El-Rufai E. The effect of health educational program on patients’ knowledge about hypertension and its’ management (in Sudan-White Nile State). Int J Prev Med Res 2016; 2(4):17-22. [ Google Scholar]
- Khadoura KJ, Shakibazadeh E, Mansournia MA, Aljeesh Y, Fotouhi A. Effectiveness of motivational interviewing on medication adherence among Palestinian hypertensive patients: a clustered randomized controlled trial. Eur J Cardiovasc Nurs 2021; 20(5):411-20. doi: 10.1093/eurjcn/zvaa015 [Crossref] [ Google Scholar]
- Sahli J, Maatoug J, Harrabi I, Ben Fredj S, Dendana E, Ghannem H. Effectiveness of a community-based intervention program to reduce hypertension prevalence among adults: results of a quasiexperimental study with control group in the region of Sousse, Tunisia. Glob Heart 2016; 11(1):131-7. doi: 10.1016/j.gheart.2016.01.001 [Crossref] [ Google Scholar]
- Saleh S, Farah A, Dimassi H, El Arnaout N, Constantin J, Osman M. Using mobile health to enhance outcomes of noncommunicable diseases care in rural settings and refugee camps: randomized controlled trial. JMIR Mhealth Uhealth 2018; 6(7):e137. doi: 10.2196/mhealth.8146 [Crossref] [ Google Scholar]
- Salman A, Abdullah I, Saib I, Abdulaziz B, Abdullah K, Yahya K. Acute effect of drinking cold Hibiscus beverage on blood pressure in adult females: a randomized controlled trial. Int J Acad Sci Res 2017; 5(1):26-34. [ Google Scholar]
- Akl C, Akik C, Ghattas H, Obermeyer CM. The cascade of care in managing hypertension in the Arab world: a systematic assessment of the evidence on awareness, treatment and control. BMC Public Health 2020; 20(1):835. doi: 10.1186/s12889-020-08678-6 [Crossref] [ Google Scholar]
- Correia JC, Lachat S, Lagger G, Chappuis F, Golay A, Beran D. Interventions targeting hypertension and diabetes mellitus at community and primary healthcare level in low- and middle-income countries: a scoping review. BMC Public Health 2019; 19(1):1542. doi: 10.1186/s12889-019-7842-6 [Crossref] [ Google Scholar]
- Hoque R, Strotheide E, Saquib J, Saquib N. Assessment of nationally representative dietary studies in the Gulf Cooperation Council: a scoping review. PeerJ 2020; 8:e10163. doi: 10.7717/peerj.10163 [Crossref] [ Google Scholar]
- World Health Organization (WHO). eHealth. WHO; 2023. Available from: https://www.emro.who.int/health-topics/ehealth/.
- Xia T, Zhao F, Nianogo RA. Interventions in hypertension: systematic review and meta-analysis of natural and quasi-experiments. Clin Hypertens 2022; 28(1):13. doi: 10.1186/s40885-022-00198-2 [Crossref] [ Google Scholar]
- World Health Organization (WHO). Health Education: Theoretical Concepts, Effective Strategies and Core Competencies: A Foundation Document to Guide Capacity Development of Health Educators. 2012. Available from: https://applications.emro.who.int/dsaf/EMRPUB_2012_EN_1362.pdf.
- Gray R, Bressington D, Ivanecka A, Hardy S, Jones M, Schulz M. Is adherence therapy an effective adjunct treatment for patients with schizophrenia spectrum disorders? A systematic review and meta-analysis. BMC Psychiatry 2016; 16:90. doi: 10.1186/s12888-016-0801-1 [Crossref] [ Google Scholar]
- Al-Qahtani SG, Alsulami BA. Prevalence and predictors of use of cupping among patients attending a primary care center in Riyadh, Saudi Arabia. J Family Med Prim Care 2023; 12(2):376-82. doi: 10.4103/jfmpc.jfmpc_1615_22 [Crossref] [ Google Scholar]
- Al Bedah AM, Khalil MK, Posadzki P, Sohaibani I, Aboushanab TS, AlQaed M. Evaluation of wet cupping therapy: systematic review of randomized clinical trials. J Altern Complement Med 2016; 22(10):768-77. doi: 10.1089/acm.2016.0193 [Crossref] [ Google Scholar]
- Lu S, Du S, Fish A, Tang C, Lou Q, Zhang X. Wet cupping for hypertension: a systematic review and meta-analysis. Clin Exp Hypertens 2019; 41(5):474-80. doi: 10.1080/10641963.2018.1510939 [Crossref] [ Google Scholar]
- Mahdavi-Roshan M, Salari A, Ghorbani Z, Ashouri A. The effects of regular consumption of green or black tea beverage on blood pressure in those with elevated blood pressure or hypertension: a systematic review and meta-analysis. Complement Ther Med 2020; 51:102430. doi: 10.1016/j.ctim.2020.102430 [Crossref] [ Google Scholar]
- Xu R, Yang K, Ding J, Chen G. Effect of green tea supplementation on blood pressure: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 2020; 99(6):e19047. doi: 10.1097/md.0000000000019047 [Crossref] [ Google Scholar]
- Zamani M, Rezaei Kelishadi M, Ashtary-Larky D, Amirani N, Goudarzi K, Torki IA. The effects of green tea supplementation on cardiovascular risk factors: a systematic review and meta-analysis. Front Nutr 2022; 9:1084455. doi: 10.3389/fnut.2022.1084455 [Crossref] [ Google Scholar]
- Ellis LR, Zulfiqar S, Holmes M, Marshall L, Dye L, Boesch C. A systematic review and meta-analysis of the effects of Hibiscus sabdariffa on blood pressure and cardiometabolic markers. Nutr Rev 2022; 80(6):1723-37. doi: 10.1093/nutrit/nuab104 [Crossref] [ Google Scholar]
- García-Muñoz AM, García-Guillén AI, Victoria-Montesinos D, Abellán-Ruiz MS, Alburquerque-González B, Cánovas F. Effect of the combination of Hibiscus sabdariffa in combination with other plant extracts in the prevention of metabolic syndrome: a systematic review and meta-analysis. Foods 2023; 12(11):2269. doi: 10.3390/foods12112269 [Crossref] [ Google Scholar]
- Ghammam R, Maatoug J, Harrabi I, Ben Fredj S, Zammit N, Laatikainen T, et al. Effectiveness of a 3-year community-based intervention for blood pressure reduction among adults: a repeated cross-sectional study with a comparison area. J Hum Hypertens. 2022. 10.1038/s41371-022-00672-2.
- Lu CH, Tang ST, Lei YX, Zhang MQ, Lin WQ, Ding SH. Community-based interventions in hypertensive patients: a comparison of three health education strategies. BMC Public Health 2015; 15:33. doi: 10.1186/s12889-015-1401-6 [Crossref] [ Google Scholar]
- Filippou CD, Tsioufis CP, Thomopoulos CG, Mihas CC, Dimitriadis KS, Sotiropoulou LI. Dietary approaches to stop hypertension (DASH) diet and blood pressure reduction in adults with and without hypertension: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr 2020; 11(5):1150-60. doi: 10.1093/advances/nmaa041 [Crossref] [ Google Scholar]
- Lari A, Sohouli MH, Fatahi S, Cerqueira HS, Santos HO, Pourrajab B. The effects of the dietary approaches to stop hypertension (DASH) diet on metabolic risk factors in patients with chronic disease: a systematic review and meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis 2021; 31(10):2766-78. doi: 10.1016/j.numecd.2021.05.030 [Crossref] [ Google Scholar]
- Saco-Ledo G, Valenzuela PL, Ruilope LM, Lucia A. Physical exercise in resistant hypertension: a systematic review and meta-analysis of randomized controlled trials. Front Cardiovasc Med 2022; 9:893811. doi: 10.3389/fcvm.2022.893811 [Crossref] [ Google Scholar]
- Jamrozik D, Borymska W, Kaczmarczyk-Żebrowska I. Hibiscus sabdariffa in diabetes prevention and treatment-does it work? An evidence-based review. Foods 2022; 11(14):2134. doi: 10.3390/foods11142134 [Crossref] [ Google Scholar]
- Karapetyan A. The Secret Weapon in Arab Food: Health Benefits of Garlic. Arab America; 2017. Available from: https://www.arabamerica.com/secret-weapon-arab-food-health-benefits-garlic/.