J Educ Community Health. 11(2):67-74.
doi: 10.34172/jech.2781
Original Article
Human Papillomavirus Vaccination Status and its Associated Factors Among Female Medical College Students in Hubei, China: A Cross-sectional Study
Huan Yang 1  , Suneerat Yangyuen 1, *
, Suneerat Yangyuen 1, *  , Kemika Sombateyotha 1
, Kemika Sombateyotha 1 
Author information:
1Faculty of Public Health, Mahasarakham University, Thailand
Abstract
Background: Despite the introduction of the human papillomavirus (HPV) vaccine in China in 2016, the uptake rates of HPV vaccination were low. This study aimed to assess the status of HPV vaccination and identify associated factors influencing HPV vaccination among female medical college students in Hubei province.
Methods: Using a multistage sampling method, this was a cross-sectional study conducted in six colleges in Hubei province in 2023. The data were collected by web-based online software. Multiple logistic regression was applied to explore factors associated with the uptake of the HPV vaccine.
Results: Overall, 1148 female medical college students were enrolled in this study. Approximately 13.9% of participants reported receiving the HPV vaccine. About 85.5% of unvaccinated participants showed high levels of intention to receive an HPV vaccine in the future, and 89.1% of the participants had accessed information about the HPV vaccine from the Internet. Multiple logistic regression demonstrated that knowledge pertaining to HPV and the HPV vaccine, factors aligned with the protection motivation theory (PMT), and socio-variables such as the mother’s educational background and the presence of vaccinated family members were associated with the uptake of the HPV vaccine.
Conclusion: Our findings revealed that the HPV vaccination was associated with the knowledge, perceived susceptibility, perceived response efficacy, and self-efficacy of HPV and the HPV vaccine among female college students. Therefore, increasing HPV and HPV vaccine knowledge within the framework of PMT may serve as an effective strategy to promote HPV vaccination rates among college students.
Keywords: Human papillomavirus viruses, Vaccination coverage, Medical students, Protection motivation theory
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Yang H, Yangyuen S, Sombateyotha K. Human papillomavirus vaccination status and its associated factors among female medical college students in Hubei, China: a cross-sectional study. J Educ Community Health. 2024; 11(2):67-74. doi:10.34172/jech.2781
Introduction
Human papillomavirus (HPV) is one of the most common sexually transmitted viruses. Most infections are generally asymptomatic and can be spontaneously resolved by the immune system within a few years, but persistent infections can result in anogenital wards and cancers (1). Globally, it is estimated that 4.5% of new cancer cases were linked to HPV infection, with cervical cancer alone contributing to 83% of these cases (2). A high prevalence of HPV was found in young adults, peaking at < 25 years old, similar to that reported in Brazil, where the HPV prevalence among adolescents aged 16–25 years old was 53.6% (3). In China, the highest HPV prevalence was also observed in the young age group, with infection rates of 55.7–37.6% in the 18–25-year-old age group (4,5). Hence, traditional college-age students (18–25 years old) are at an increased risk of acquiring HPV. To prevent HPV infection, the Center for Disease Control and Prevention’s Advisory Committee on Immunization Practices recommends that college students under 26 years old complete the HPV vaccine series (6).
However, the current status of HPV vaccine uptake rates among Chinese college students remains low, far behind the World Health Organization’s goal of achieving 90% HPV vaccination coverage (7). According to a study conducted in 136 colleges in China, only 11.0% of college students reported being vaccinated against HPV nationwide, and 53.5% of unvaccinated college students expressed an intention to initiate the HPV vaccine (8). Even in Beijing, the capital city of China, the HPV vaccination rate among female college students was only 9.5% (9). Accordingly, elevating HPV vaccination rates among Chinese college students is crucial.
HPV vaccines have proved to be the most effective primary prevention strategy for reducing HPV infection and HPV-associated disease (10). Although four kinds of HPV vaccines are now commercially available in China, none of them have been included in the national immunization program (11). This may be one of the reasons for the low rate of HPV vaccination among college students in China (12). In addition, previous research revealed factors influencing HPV vaccination, including limited knowledge regarding HPV, a family history of infection-related diseases, cost, HPV infection prevention awareness, a lack of risk perception for HPV infection, and a lack of recommendations from a healthcare provider (12,13). Of these, the most influential factor in the successful delivery of HPV vaccination is likely an effective recommendation from a healthcare provider (14). Healthcare providers’ attitudes toward vaccination and recommendations play a significant role in the general population’s trust in vaccination and their HPV vaccination intention (15). As future healthcare providers, medical students play an important role in promoting the spread of correct information and the availability of HPV vaccines. However, one study found that more than 60.0% of the medical college students themselves reported hesitancy about the HPV vaccine (16), and only 9% of female medical college students received an HPV vaccine in China (17).
In Hubei Province, China, previous research reported that the highest prevalence of HPV infection (22.65%) was also found in the age group below 25 years (18). Thus, college-age youths in Hubei province were considered at high risk of HPV infection and HPV-related disease. However, only 58.7% of the college students at this age had heard of the HPV vaccine, and 34.7% considered taking the HPV vaccine in Hubei province (19). Further, there are a few reports about the HPV vaccination status, and the evidence for factors contributing to HPV vaccination among female medical students in Hubei remains limited. Thus, this study sought to explore the HPV vaccination status and its potential associated factors among unvaccinated female medical college students in Hubei Province, China, which will help us understand factors influencing HPV vaccination and provide evidence for health decision-makers to plan or implement effective strategies to optimize uptake of the HPV vaccine.
Materials and Methods
Study Design and Setting
A cross-sectional study was conducted in six colleges in Hubei province, China, from January to May 2023.
Study Population and Sampling
The eligible participants were female medical college students aged 18–26 who could speak Mandarin and were willing to participate, although they were excluded if they provided an incomplete answer or showed a lack of interest in participation. The sample size estimation was calculated using Daniel’s (20) formula
, with an estimator of the percentage of female college students’ intention to initiate the HPV vaccine in the central part of China being 46.2% (10), a 95% confidence interval, and 3% maximum allowable error. This accounted for 1033 participants, plus 10% compensation for nonresponses or dropouts. The final sample size was 1148. The female college students who met the eligible criteria were enrolled using the multistage sampling method. First, the selection of six colleges was conducted through a lottery method among all 21 colleges with medical majors in Hubei province. Second, the six faculties of each college were chosen using the lottery method from a predefined list. Finally, the student selection process took place within each college, employing a systematic random sampling approach.
Data Collection Tool and Technique
The structured questionnaires in Chinese were developed based on a literature review, which consisted of six parts as follows:
Part 1: Sociodemographic factors included age, academic year, parents’ education background, family yearly household income, history of sexual intercourse, vaccinated family members, willingness to pay for the vaccine, vaccination status, and sources of information about the HPV vaccine.
Part 2: The intention to initiate HPV vaccination was measured using one item developed by Huang et al (21). The participants were asked to “please rate your intention to get HPV vaccination in the future” from 1 (totally no intention) to 10 (extremely high intention). A higher score on the item indicates a higher willingness to receive vaccinations afterward. This variable was also dichotomized for analysis by median. Participants were coded as having low intention if they responded 5 or less; otherwise, they were coded as having high intention.
Part 3: The knowledge of HPV was assessed using a 15-item HPV knowledge scale (e.g., people with HPV have visible signs or symptoms of the infection; close skin-to-skin touching will infect HPV) adapted from existing published measures (22), with all items judged as true or false. The participants received one point for a correct response, with a higher total score indicating a greater level of knowledge of HPV.
Part 4: The knowledge of the HPV vaccine was measured using an 11-item HPV knowledge scale modified from the student HPV survey (23). Knowledge of the HPV vaccine (e.g., the nine-valent HPV vaccine is recommended for females aged 9‒26 years in China; sexually active females cannot benefit from the vaccine) is also gained by judging whether it is true or false. Participants received one point for a correct response, with a higher total score implying a greater level of knowledge of HPV.
Part 5: HPV infection prevention awareness was adapted from a former study (24). The questionnaire consisted of three subscales, including HPV infection risk factors (6 items; e.g., non-use of a condom during intercourse is the HPV infection risk factor,or alcohol consumption is the HPV infection risk factor). The other subscales were transmitted ways (3 items; e.g., HPV is transmitted during vaginal or anal sex, or HPV is transmitted through cough) and HPV infection prevention (7 items; e.g., the HPV vaccine can prevent the HPV infection, or condoms can prevent HPV infection). All items were judged as true or false. Participants received one point for a correct response, with a higher total score representing a greater level of awareness of HPV infection prevention.
Part 6: The Protection Motivation Theory (PMT) was measured by the PMT scale adapted from previous research (25). The PMT questionnaire consisted of 4 subscales, including participants’ perceived susceptibility (3 items; e.g., HPV infection peak in older adults, not young people, or I am healthy, I will not contract HPV in my lifetime) and perceived severity (4 items; e.g., HPV infection can cause women to have cervical cancer, or HPV infection can cause women to have genital warts). The other subscales were perceived response efficacy (4 items; e.g., HPV vaccination can reduce the risk of HPV-related cancer, or HPV vaccination can reduce the risk of getting genital warts) and perceived self-efficacy (5 items; e.g., I will get the HPV vaccine even if it is not covered by health insurance, or I will complete the whole procedure of HPV vaccination once I get the first dose). The respondents were asked to rate their agreement on a five-point Likert-type scale, ranging from 1 (strongly disagree) to 5 (strongly agree). A higher score on each subscale indicated a stronger presence of the corresponding construct in the participants’ responses.
A pilot study was randomly conducted among 50 medical students studying in a college similar to our setting and meeting the inclusion criteria of the study. The Kuder-Richardson Formula 20 (KR-20) (26) was used to measure the internal consistency reliability of a test in which each question only has a right or wrong answer, such as the knowledge of HPV (KR-20 = 0.90) and HPV vaccine (KR-20 = 0.90), and HPV infection prevention awareness (KR-20 = 0.83). The Cronbach’s alpha coefficient was calculated for the internal consistency of the PMT scale. Cronbach’s alpha for PMT subscale perceived susceptibility, perceived severity, perceived response efficacy, and perceived self-efficacy were 0.94, 0.95, 0.97, and 0.96, respectively. The content validity of the measurement was determined by the index of item objective congruence (IOC) (27). The range of the index score for an item was -1 to 1. Accordingly, an expert evaluates each item by giving a rating of 1 for clearly measuring the objective, -1 for not clearly measuring, or 0 for the unclear objective. The IOC for knowledge of HPV, knowledge of HPV vaccine, PMT scale, intention to initiate HPV vaccination, and HPV infection prevention awareness was 0.92, 0.85, 1.00, 0.88, and 0.85, respectively.
Statistical Analysis
Descriptive statistics were performed for all variables. Chi-square tests were utilized for categorical variables, and independent sample t-tests were used for continuous variables to compare the differences between the groups with and without HPV vaccination. Binary logistic regression was employed to assess potential factors influencing the intention to initiate HPV vaccination. Variables that exhibited a significance level (P < 0.25) (28) during the bivariate analysis were incorporated into the multiple logistic regression model. The adjusted odds ratio was estimated from multiple logistic regression to determine the relationship between knowledge and awareness factors, PMT constructs, socio-demographic factors, and HPV vaccination status after adjusting for all other predictors. A series model was developed, such as in model 1, three knowledge awareness variables were added to the model to assess the association between these factors and HPV vaccination status only. Then, the PMT constructs were entered into Model 1 to investigate the relationship between knowledge and awareness factors, the PMT constructs, and HPV vaccination status after adjusting for each predictor. Finally, all sociodemographic factors were entered into Model 3 to examine the association between knowledge and awareness factors, the PMT constructs, and HPV vaccination status after adjusting for all sociodemographic variables. The level of statistical significance was set at P < 0.05 in both bivariate and multivariate analyses. All analyses were conducted using SPSS, version 19.0 (IBM Corporation, Armonk, NY, USA).
Results
In this study, a total of 1148 female medical college students initially participated, 13.9% of whom were ever vaccinated against HPV. The result of chi-square tests showed that there was a statistically significant difference between the vaccine and unvaccinated groups in place of birth, father’s education background, mother’s education background, vaccinated family members, willingness to pay, and vaccination intention (P< 0.05). The score of knowledge of HPV and the HPV vaccine and that of HPV infection prevention awareness were significantly higher in the vaccine group compared to the unvaccinated group. Female medical college students who received HPV vaccination posed a higher score of perceived susceptibility (5.5 ± 1.9), perceived severity (13.8 ± 3.6), perceived response efficacy (18.1 ± 2.2), and perceived self-efficacy (22.4 ± 2.8) (P< 0.05). More details are provided in Table 1.
Table 1.
Distribution of Demographic Characteristics of the Study Population by Vaccine Status (N = 1148)
|
Variable
|
Vaccine Status
|
χ2/t
|
P
|
|
Total (N=1148)
|
Vaccine (n=160)
|
Unvaccinated (n=988)
|
|
n (%)
|
n (%)
|
n (%)
|
| Sociodemographic factors |
|
|
|
|
|
| Age (years) |
19.3 ± 1.1 |
19.5 ± 1.2 |
19.3 ± 1.1 |
3.28 |
0.070 |
| Place of birth |
|
|
|
|
|
| Village |
631 (55.0) |
54 (33.8) |
577 (58.4) |
34.65 |
0.000 |
| City |
517 (45.0) |
106 (66.2) |
411 (41.6) |
|
|
| Father’s education background |
|
|
|
|
|
| Less than high school |
705 (61.4) |
63 (39.4) |
642 (65.0) |
38.09 |
0.000 |
| High school and above |
443 (38.6) |
97 (60.6) |
346 (35.0) |
|
|
| Mather’s education background |
|
|
|
|
|
| Less than high school |
787 (68.6) |
74 (46.3) |
713 (72.2) |
42.9 |
0.000 |
| High school and above |
361 (31.4) |
86 (53.8) |
275 (27.8) |
|
|
| Family yearly household income |
|
|
|
|
|
| Less than 50,000 CNY |
780 (67.9) |
77 (48.1) |
703 (71.2) |
33.52 |
0.000 |
| 50,000 CNY and above |
368 (32.1) |
83 (51.9) |
285 (28.8) |
|
|
| Vaccinated family members |
|
|
|
|
|
| Yes |
525 (45.7) |
144 (90.0) |
479 (48.5) |
95.64 |
0.000 |
| No |
623 (54.3) |
16 (10.0) |
509 (51.5) |
|
|
| Willingness to pay |
|
|
|
|
|
| Yes |
957 (83.4) |
144 (90.0) |
813 (82.3) |
5.90 |
0.015 |
| No |
191 (16.6) |
16 (10.0) |
175 (17.7) |
|
|
| History of sexual intercourse |
|
|
|
|
|
| Yes |
66 (5.7) |
10 (6.3) |
56 (5.7) |
0.08 |
0.769 |
| No |
1,082 (94.3) |
150 (93.8) |
932 (94.3) |
|
|
| Vaccination intention |
|
|
|
|
|
| High level |
994 (86.6) |
143 (92.9) |
845 (85.5) |
6.845 |
0.008 |
| Low level |
154 (13.4) |
11 (7.1) |
143 (14.5) |
|
|
| Knowledge and awareness |
|
|
|
|
|
| Knowledge of HPV |
8.0 ± 3.0 |
9.4 ± 3.2 |
7.7 ± 3.0 |
33.15 |
0.000 |
| Knowledge of HPV vaccine |
7.0 ± 2.7 |
8.4 ± 3.1 |
6.7 ± 2.6 |
21.18 |
0.000 |
| HPV infection prevention awareness |
11.6 ± 1.9 |
12.7 ± 1.7 |
11.4 ± 1.9 |
5.57 |
0.018 |
| The PMT scale |
|
|
|
|
|
| Perceived susceptibility |
5.0 ± 2.1 |
5.5 ± 1.9 |
4.8 ± 2.2 |
30.12 |
0.000 |
| Perceived severity |
12.6 ± 5.4 |
13.8 ± 3.6 |
12.8 ± 5.1 |
61.60 |
0.000 |
| Perceived response efficacy |
16.1 ± 3.6 |
18.1 ± 2.2 |
15.7 ± 3.5 |
9.49 |
0.001 |
| Perceived self-efficacy |
19.8 ± 4.1 |
22.4 ± 2.8 |
19.3 ± 4.0 |
8.25 |
0.001 |
Note. Values are presented as numbers (%) or means ± standard deviations; CNY: Chinese Yuan; PMT: Protection Motivation Theory; HPV: Human papillomavirus.
In the context of sourcing information pertaining to the HPV vaccine, it is noteworthy that a substantial majority of the study’s participants (89.1%) have conveyed their reliance on the Internet as their primary information outlet. After the internet, the other predominant sources of information acquisition were personal connections, encompassing friends (50.4%) and teachers (44.9%), respectively (Figure 1).
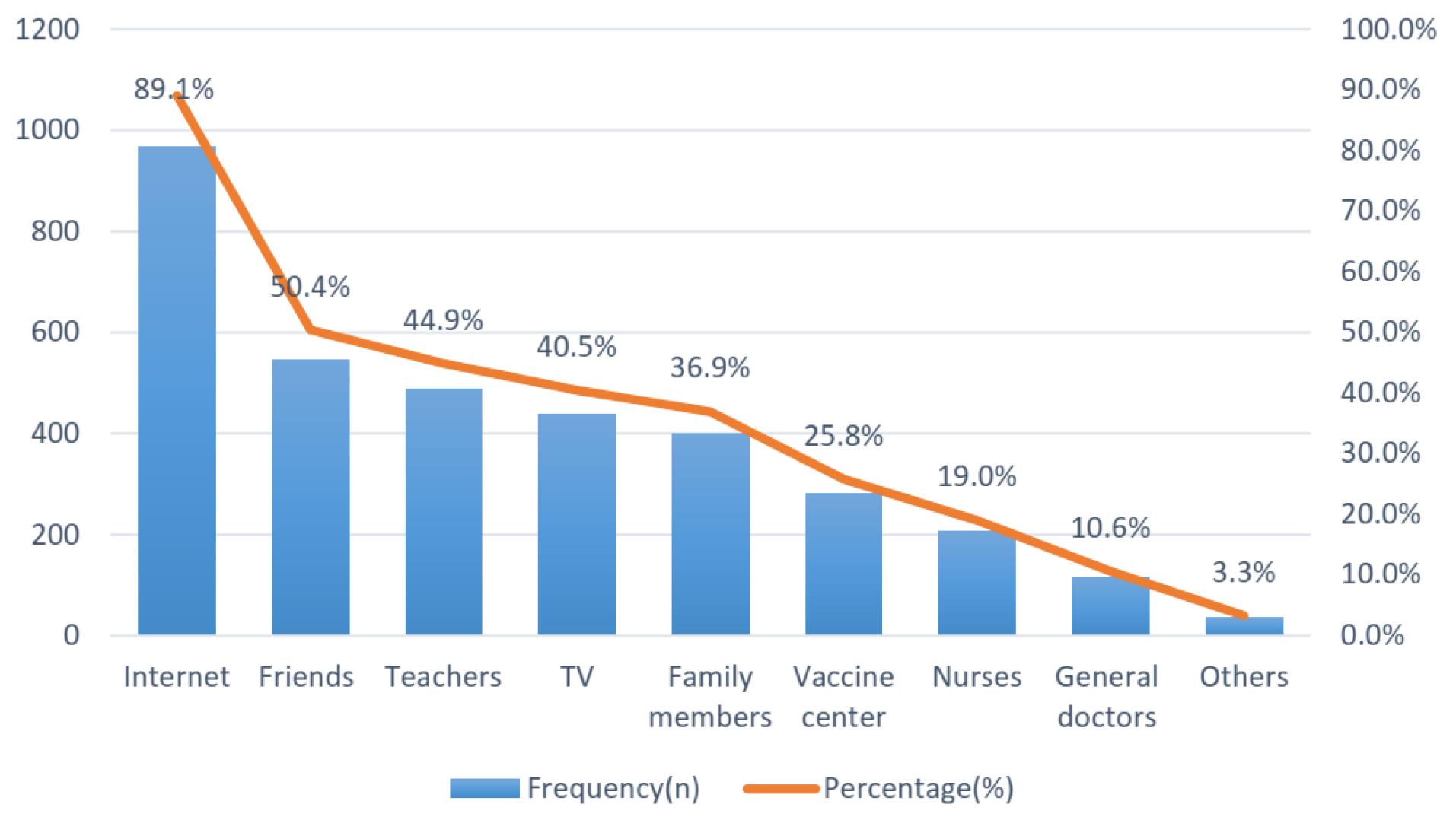
Figure 1.
Sources of Information About HPV Vaccines. Note. HPV: Human papillomavirus
.
Sources of Information About HPV Vaccines. Note. HPV: Human papillomavirus
In bivariate analyses, factors that were found statistically associated with HPV vaccination status at P < 0.05 were all three dimensions of knowledge and information-receiving factors, four factors grounded in PMT, and some sociodemographic factors. Among sociodemographic attributes, age, place of birth, parents’ educational background, yearly household income, vaccinated family members, and willingness to pay were contributors to HPV vaccination (Table 2).
Table 2.
Odds Ratios and 95% Confidence Intervals From Logistic Regression for HPV Vaccination Status
|
Variables
|
Bivariate
|
Model 1
|
Model 2
|
Model 3
|
Unadjusted OR
(95% CI)
|
P
Value
|
Adjusted OR
(95% CI)
|
P
Value
|
Adjusted OR
(95% CI)
|
P
Value
|
Adjusted OR
(95% CI)
|
P
Value
|
| Knowledge and awareness |
|
|
|
|
|
|
|
|
| Knowledge of HPV |
1.28 (1.19-1.38) |
< 0.001 |
1.27 (1.14-1.41) |
< 0.001 |
1.14 (1.04-1.24) |
0.005 |
1.18 (1.08-1.29) |
0.012 |
| Knowledge of HPV vaccine |
1.37 (1.25-1.49) |
< 0.001 |
1.18 (1.08-1.29) |
< 0.001 |
1.12 (1.01-1.25) |
0.032 |
1.04 (0.94-1.04) |
0.303 |
| HPV infection prevention awareness |
1.46 (1.32-1.61) |
< 0.001 |
1.36 (1.23-1.51) |
< 0.001 |
1.37 (1.24-1.54) |
< 0.001 |
1.22 (1.09-1.37) |
< 0.001 |
| The PMT theory |
|
|
|
|
|
|
|
|
| Perceived susceptibility |
1.12 (1.05-1.20) |
0.001 |
- |
- |
1.14 (1.14-1.23) |
0.002 |
1.01 (0.91-1.13) |
0.002 |
| Perceived severity |
1.04 (1.02-1.08) |
0.004 |
- |
- |
0.99 (0.95-1.02) |
0.455 |
1.06 (1.01-1.11) |
0.375 |
| Perceived response efficacy |
1.29 (1.21-1.38) |
< 0.001 |
- |
- |
1.09 (1.01-1.20) |
0.030 |
1.10 (1.03-1.17) |
0.026 |
| Perceived self-efficacy |
1.27 (1.20-1.34) |
< 0.001 |
- |
- |
1.19 (1.11-1.27) |
< 0.001 |
1.09 (1.00-1.16) |
0.001 |
| Sociodemographic factors |
|
|
|
|
|
|
|
|
| Age (year) |
1.23 (1.06 -1.41) |
0.006 |
- |
- |
- |
- |
0.86 (0.68-1.07) |
0.810 |
| Place of birth (Ref.: village) |
2.76 (1.94~3.92) |
< 0.001 |
- |
- |
- |
- |
0.78 (0.43-1.40) |
0.311 |
| Father went high school and above (Ref.: less than high school) |
0.35 (0.25-0.49) |
< 0.001 |
- |
- |
- |
- |
0.70 (0.40-1.23) |
0.233 |
| Mother went high school and above (Ref.: less than high school) |
3.01 (2.14-4.23) |
0.001 |
- |
- |
- |
- |
1.02 (0.56-1.86) |
0.019 |
| Yearly household income (Ref.: less than 50,000) |
2.66 (1.89 -3.73) |
< 0.001 |
- |
- |
- |
- |
0.16 (0.08-0.30) |
0.137 |
| History of sexual intercourse |
0.90 (0.45-1.81) |
0.769 |
- |
- |
- |
- |
1.46 (0.48-4.45) |
0.365 |
| Vaccinated family members |
0.11 (0.61-0.17) |
< 0.001 |
- |
- |
- |
- |
1.07 (1.51-2.25) |
< 0.001 |
| Willingness to pay |
0.34 (0.18-0.64) |
< 0.001 |
- |
- |
- |
- |
0.16 (0.09-0.28) |
0.866 |
Note. OR: Odds ratio; CI: Confidence interval; Ref: Reference group; CNY: Chinese Yuan; HPV: Human papillomavirus.
In multiple logistic regression analyses, Model 1 revealed that factors related to knowledge and information acquisition were positively associated with HPV vaccination, which is consistent with the results obtained from the univariate model. Model 2 extended upon Model 1 by incorporating additional factors from the PMT factors. Notably, the presence of knowledge regarding HPV and awareness of HPV infection prevention remained significantly associated with HPV vaccination. Moreover, three out of the four PMT constructs, which were perceived susceptibility, perceived response efficacy, and perceived self-efficacy, showed a positive association with HPV vaccination. Further expanding upon Model 2, Model 3 introduced socio-demographic factors. Within this model, two knowledge and information acquisition factors and three PMT constructs continued to exhibit a significant association with HPV vaccination. After accounting for the influence of other predictors, it was determined that only the vaccinated family member and mother’s education background factors, among the socio-demographic factors, were related to HPV vaccination (Table 2).
Discussion
In this study, HPV vaccine uptake was 13.0% among female college students in Hubei province, the central division in China, which was higher than that of a prior study in Beijing (9.5%) (29) and Guangzhou (3.1%) (30) among college students in 2018. However, it is still lower than that in countries such as the United States (75%) (31), Ethiopia (61.2%) (32), and Melaka Malaysia (77.9%) (33). It was even lower than the global coverage of the first dose of HPV vaccination (21%) in 2022 (34). This may be because, in comparison to other countries, China has not yet included the HPV vaccine in the national immunization program, so the HPV vaccination rates have remained rather low. According to the evidence, if 50% of eligible females were HPV vaccinated, HPV type 16 and 18 infections would decrease by almost 70% in countries (35). Our study findings demonstrated that the majority of the participants (94.3%) had never had sexual intercourse, and all of them were less than 26 years old, so catch-up vaccination can provide unvaccinated college students with substantial benefits. Thus, to improve HPV vaccination rates, this age group should receive special attention.
This study also revealed that knowledge played an important role in HPV vaccination among female medical college students. The students who had higher scores of knowledge of HPV and HPV infection prevention awareness were more likely to be vaccinated. This aligns with the findings of previous research by Mihretie et al (36) and Wu et al (37), indicating that having HPV vaccine knowledge was significantly associated with the uptake of this vaccine. One possible explanation is that gaining relevant knowledge may affect individuals by influencing their understanding of this virus (38). However, our results also represented that female medical college students only had a moderate knowledge level about HPV and HPV vaccines, which is consistent with the results of a previous study (37), implying that college students did not know much about HPV and HPV vaccines. To increase their knowledge about the HPV vaccine, providing more information from various sources will be helpful. In our study, participants stated that their primary three information sources about the HPV vaccine were the internet, friends, and teachers, respectively. The same results were also found in a previous study, which pointed out that the internet and teachers were the main sources of information about HPV and HPV vaccination (19). One data-driven computational model also revealed that peer influence is one of the key determinant factors for vaccine perception (39). This suggests that online health information-seeking behavior may have a potential positive correlation with college students’ intentions to get the HPV vaccine. This observation provides insight into the potential reliance on these avenues for HPV-related education in the future.
Based on our findings, HPV vaccine uptake was influenced by PMT-related factors, particularly perceived susceptibility, perceived response efficacy, and perceived self-efficacy. Thus, participants who perceived HPV infection as easy to get, believed in the effectiveness of the vaccine, and felt confident in their ability to receive and benefit from the vaccine were more inclined to get the HPV vaccine. Our results are consistent with those of previous studies by Huang et al (21) and Mohammad Nabizadeh et al (40). They postulated that individuals’ perceptions of threat and efficacy were significantly linked with health-related behaviors. However, our results showed that the perceived severity of HPV infection and HPV-associated diseases was not a predictor of HPV vaccination. This may be because participants perceive HPV as less severe or less personally threatening, leading to variations in vaccination decisions. Tailored education interventions to enhance participants’ understanding of the severity of HPV infection and its potential consequences are still necessary.
Furthermore, our findings revealed that the vaccinated family member and mother’s educational background were related to HPV vaccine uptake, which conforms to the findings of studies conducted in Turkey (41) and the USA (42), indicating that the mother’s HPV experience and knowledge were associated with daughters’ HPV vaccine uptake. Parents who had a strong belief that the HPV vaccine was safe in terms of adverse effects were 10 times more likely to decide to vaccinate their daughters against HPV (43). A recent study conducted by Dickinson et al (44) also pointed out that more than half of the parents had knowledge of HPV and the HPV vaccine, with 79.2% of them considering having their child vaccinated. Hence, ways to improve parents’ knowledge and awareness should be adopted to improve the acceptance of the HPV vaccine and then the vaccination status of college students.
Limitations and Recommendations
Several limitations must be acknowledged in this study. First, the cross-sectional design restricted our ability to establish causal relationships between the predictors and HPV vaccine uptake. Further longitudinal research would be beneficial in elucidating the temporal dynamics of these factors. Second, the study relied on self-reported data, which may introduce response biases. Future research could employ objective measures or utilize mixed-method approaches to enhance data validity. Additionally, the study was conducted among a specific population of female medical college students, which limits the generalizability of the findings to other populations.
Conclusion
Overall, our findings demonstrated that HPV vaccination coverage in Hubei province was still low among female medical students. The students in our study exhibited low levels of perceived susceptibility but a moderate level of perceived severity and knowledge and awareness of HPV and the HPV vaccine, as well as high levels of perceived response efficacy and self-efficacy toward HPV and the HPV vaccine. Knowledge about HPV and the HPV vaccine, three PMT constructs, and sociodemographic factors (mother’s educational background and familial vaccination history) were identified as factors for promoting HPV vaccination coverage. These results indicated that future interventions should aim to increase appropriate knowledge, enhanced perceived susceptibility, perceived response efficacy, and self-efficacy to promote HPV vaccination coverage among college students.
Acknowledgements
We would like to sincerely thank all study subjects from Wuhan City College, Huanggang Polytechnic College, Jingzhou College of Technology, Hubei College of Arts and Science, Hubei Engineering Vocational and Technical College, and Wuhan College of Foreign Language and Affairs for their participation.
Authors’ Contribution
Conceptualization: Huan Yang,Suneerat Yangyuen, Kemika Sombateyotha.
Data Curation: Huan Yang, Suneerat Yangyuen.
Formal analysis: Huan Yang, Suneerat Yangyuen, Kemika Sombateyotha.
Funding acquisition: Huan Yang, Suneerat Yangyuen, Kemika Sombateyotha.
Investigation: Huan Yang.
Methodology: Huan Yang, Suneerat Yangyuen.
Project administration: Huan Yang, Suneerat Yangyuen.
Resources: Huan Yang, Suneerat Yangyuen.
Software: Huan Yang, Suneerat Yangyuen.
Supervision: Suneerat Yangyuen, Kemika Sombateyotha.
Validation: Huan Yang, Suneerat Yangyuen.
Visualization: Huan Yang, Suneerat Yangyuen.
Writing–original draft: Huan Yang.
Writing–review & editing: Suneerat Yangyuen, Kemika Sombateyotha.
Competing Interests
None declared.
Ethical Approval
This study was reviewed and approved by the Review Ethics Boards of Mahasarakham University (Ref No. 090-045/2023). Written informed consent was obtained from the participants following the research information.
Funding
This research project was financially supported by the Faculty of Public Health, Mahasarakham University.
References
- Plotzker RE, Vaidya A, Pokharel U, Stier EA. Sexually transmitted human papillomavirus: update in epidemiology, prevention, and management. Infect Dis Clin North Am 2023; 37(2):289-310. doi: 10.1016/j.idc.2023.02.008 [Crossref] [ Google Scholar]
- de Martel C, Plummer M, Vignat J, Franceschi S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int J Cancer 2017; 141(4):664-70. doi: 10.1002/ijc.30716 [Crossref] [ Google Scholar]
- Wendland EM, Villa LL, Unger ER, Domingues CM, Benzaken AS. Prevalence of HPV infection among sexually active adolescents and young adults in Brazil: the POP-Brazil study. Sci Rep 2020; 10(1):4920. doi: 10.1038/s41598-020-61582-2 [Crossref] [ Google Scholar]
- Zhang W, Guo N, Li B, Shang E, Wang J, Zhang M. Prevalence and genotype distribution of human papillomavirus infections in Beijing, China between 2016 and 2020. Virol J 2023; 20(1):11. doi: 10.1186/s12985-023-01959-7 [Crossref] [ Google Scholar]
- Wang T, Luan L, Deng J, Liu N, Wu Q, Gong T. Prevalence and human papillomavirus (HPV) genotype distribution in Suzhou, China. Hum Vaccin Immunother 2023; 19(2):2241309. doi: 10.1080/21645515.2023.2241309 [Crossref] [ Google Scholar]
- Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination - updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep 2016; 65(49):1405-8. doi: 10.15585/mmwr.mm6549a5 [Crossref] [ Google Scholar]
- World Health Organization (WHO). Cervical Cancer Strategy. Cervical Cancer Elimination. Available from: https://www.who.int/initiatives/cervical-cancer-elimination-initiative/strategy. Accessed August 22, 2023.
- You D, Han L, Li L, Hu J, Zimet GD, Alias H. Human papillomavirus (HPV) vaccine uptake and the willingness to receive the HPV vaccination among female college students in China: a multicenter study. Vaccines (Basel) 2020; 8(1):31. doi: 10.3390/vaccines8010031 [Crossref] [ Google Scholar]
- Liu Y, Di N, Tao X. Knowledge, practice and attitude towards HPV vaccination among college students in Beijing, China. Hum Vaccin Immunother 2020; 16(1):116-23. doi: 10.1080/21645515.2019.1638727 [Crossref] [ Google Scholar]
- Rosenblum HG, Lewis RM, Gargano JW, Querec TD, Unger ER, Markowitz LE. Declines in prevalence of human papillomavirus vaccine-type infection among females after introduction of vaccine - United States, 2003-2018. MMWR Morb Mortal Wkly Rep 2021; 70(12):415-20. doi: 10.15585/mmwr.mm7012a2 [Crossref] [ Google Scholar]
- Zhao FH, Wu T, Hu YM, Wei LH, Li MQ, Huang WJ. Efficacy, safety, and immunogenicity of an Escherichia coli-produced human papillomavirus (16 and 18) L1 virus-like-particle vaccine: end-of-study analysis of a phase 3, double-blind, randomised, controlled trial. Lancet Infect Dis 2022; 22(12):1756-68. doi: 10.1016/s1473-3099(22)00435-2 [Crossref] [ Google Scholar]
- Dapari R, Li M, Chen X, Cui J, Ahmad Zamzuri MAI, Hassan MR. Factors influencing HPV vaccine acceptance among females in mainland China: a systematic review. Clin Epidemiol Glob Health 2024; 26:101514. doi: 10.1016/j.cegh.2024.101514 [Crossref] [ Google Scholar]
- Tung WC, Chen Y, Yang X, Lam C. Human papillomavirus vaccination: a quantitative cross-sectional study of perceived barriers, influential advisors, and acculturation among Chinese college students aged 18-26 in the USA. Psychol Health Med 2024; 29(4):856-67. doi: 10.1080/13548506.2023.2277152 [Crossref] [ Google Scholar]
- Daniel CL, McLendon L, Green CL, Anderson KJ, Pierce JY, Perkins A. HPV and HPV vaccination knowledge and attitudes among medical students in Alabama. J Cancer Educ 2021; 36(1):168-77. doi: 10.1007/s13187-019-01613-3 [Crossref] [ Google Scholar]
- Dybsand LL, Hall KJ, Carson PJ. Immunization attitudes, opinions, and knowledge of healthcare professional students at two Midwestern universities in the United States. BMC Med Educ 2019; 19(1):242. doi: 10.1186/s12909-019-1678-8 [Crossref] [ Google Scholar]
- Zhou L, Wang J, Cheng P, Li Y, Liu G, Zhang X. HPV vaccine hesitancy among medical students in China: a multicenter survey. Front Public Health 2022; 10:774767. doi: 10.3389/fpubh.2022.774767 [Crossref] [ Google Scholar]
- Liu Y, Jiang X, Xu L, Di N, Jiang L, Tao X. Difference between medical and nonmedical students on knowledge, practice, and attitude towards the human papillomavirus vaccine in China: a cross-sectional study. J Cancer Educ 2021; 36(5):1014-21. doi: 10.1007/s13187-019-01682-4 [Crossref] [ Google Scholar]
- Xiang F, Guan Q, Liu X, Xiao H, Xia Q, Liu X. Distribution characteristics of different human papillomavirus genotypes in women in Wuhan, China. J Clin Lab Anal 2018; 32(8):e22581. doi: 10.1002/jcla.22581 [Crossref] [ Google Scholar]
- Xu Y, Bi W, Liu T, Jiang Y, Wang Q, Fan R. Factors associated with intention of human papillomavirus vaccination among Chinese college students: implications for health promotion. Hum Vaccin Immunother 2021; 17(12):5426-32. doi: 10.1080/21645515.2021.2007014 [Crossref] [ Google Scholar]
- Daniel WW, Cross CL. Biostatistics: A Foundation for Analysis in the Health Sciences. 11th ed. Wiley; 2018.
- Huang PC, Hung CH, Kuo YJ, Chen YP, Ahorsu DK, Yen CF. Expanding protection motivation theory to explain willingness of COVID-19 vaccination uptake among Taiwanese university students. Vaccines (Basel) 2021; 9(9):1046. doi: 10.3390/vaccines9091046 [Crossref] [ Google Scholar]
- Sukmadewi Sukmadewi, Chunuan S, Wiwattanawongsa K, Widayati A. A predictive model of human papillomavirus vaccination intention among young women in southern Thailand. Pac Rim Int J Nurs Res 2021; 25(2):298-311. [ Google Scholar]
- Thomas T, Dalmida S, Higgins M. The student human papillomavirus survey: nurse-led instrument development and psychometric testing to increase human papillomavirus vaccine series completion in young adults. J Nurs Meas 2016; 24(2):226-44. doi: 10.1891/1061-3749.24.2.226 [Crossref] [ Google Scholar]
- Cocchio S, Bertoncello C, Baldovin T, Fonzo M, Bennici SE, Buja A. Awareness of HPV and drivers of HPV vaccine uptake among university students: a quantitative, cross-sectional study. Health Soc Care Community 2020; 28(5):1514-24. doi: 10.1111/hsc.12974 [Crossref] [ Google Scholar]
- Li TT. A Study on Adult Female HPV Vaccination Behavior and Willingness to Vaccinate Based on Protection Motivation Theory [dissertation]. China: Wuhan University of Light Industry; 2019.
- Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ 2011; 2:53-5. doi: 10.5116/ijme.4dfb.8dfd [Crossref] [ Google Scholar]
- Fouzul Kareema MI, Bt Zubairi AM. Item objective congruence analysis for multidimensional items content validation of a reading test in Sri Lankan university. Engl Lang Teach 2022; 15(1):106-17. [ Google Scholar]
- Chowdhury MZ, Turin TC. Variable selection strategies and its importance in clinical prediction modelling. Fam Med Community Health 2020; 8(1):e000262. doi: 10.1136/fmch-2019-000262 [Crossref] [ Google Scholar]
- Liu Y, Di N, Tao X. Knowledge, practice and attitude towards HPV vaccination among college students in Beijing, China. Hum Vaccin Immunother 2020; 16(1):116-23. doi: 10.1080/21645515.2019.1638727 [Crossref] [ Google Scholar]
- Ma Y, Wang C, Liu F, Lian G, Li S, He Q. Human papillomavirus vaccination coverage and knowledge, perceptions and influencing factors among university students in Guangzhou, China. Hum Vaccin Immunother 2021; 17(10):3603-12. doi: 10.1080/21645515.2021.1927411 [Crossref] [ Google Scholar]
- Pingali C, Yankey D, Elam-Evans LD, Markowitz LE, Williams CL, Fredua B. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years - United States, 2020. MMWR Morb Mortal Wkly Rep 2021; 70(35):1183-90. doi: 10.15585/mmwr.mm7035a1 [Crossref] [ Google Scholar]
- Hailu G, Wirtu D, Tesfaye T, Getachew M. Human papillomavirus vaccine uptake and associated factors among adolescent girls in high schools of Nekemte city, Western Ethiopia, 2020. BMC Womens Health 2023; 23(1):560. doi: 10.1186/s12905-023-02702-8 [Crossref] [ Google Scholar]
- Al-Naggar RA, Bobryshev YV, Al-Jashamy K, Al-Musli M. Practice of HPV vaccine and associated factors among school girls in Melaka, Malaysia. Asian Pac J Cancer Prev 2012; 13(8):3835-40. doi: 10.7314/apjcp.2012.13.8.3835 [Crossref] [ Google Scholar]
- World Health Organization (WHO). Human Papillomavirus (HPV) Vaccination Coverage. Available from: https://immunizationdata.who.int/pages/coverage/hpv.html. Accessed August 22, 2023.
- Drolet M, Bénard É, Pérez N, Brisson M. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis. Lancet 2019; 394(10197):497-509. doi: 10.1016/s0140-6736(19)30298-3 [Crossref] [ Google Scholar]
- Mihretie GN, Liyeh TM, Ayele AD, Belay HG, Yimer TS, Miskr AD. Female adolescents’ knowledge and acceptability of human papillomavirus vaccine in Debre Tabor town, Ethiopia: a cross-sectional study. BMJ Open 2023; 13(3):e061813. doi: 10.1136/bmjopen-2022-061813 [Crossref] [ Google Scholar]
- Wu H, Tong X, Wang L, Huang Y, Zhang L. HPV vaccine information, knowledge, attitude, and recommendation intention among male college students in China. Hum Vaccin Immunother 2023; 19(2):2228163. doi: 10.1080/21645515.2023.2228163 [Crossref] [ Google Scholar]
- Varer Akpinar C, Alanya Tosun S. Knowledge and perceptions regarding human papillomavirus (HPV) and willingness to receive HPV vaccination among university students in a north-eastern city in Turkey. BMC Womens Health 2023; 23(1):299. doi: 10.1186/s12905-023-02455-4 [Crossref] [ Google Scholar]
- Ghosh S, Bhattacharya S, Mukherjee S, Chakravarty S. Promote to protect: data-driven computational model of peer influence for vaccine perception. Sci Rep 2024; 14(1):306. doi: 10.1038/s41598-023-50756-3 [Crossref] [ Google Scholar]
- Mohammad Nabizadeh S, Taymoori P, Hazhir MS, Shirazi M, Roshani D, Shahmoradi B. Predicting vitamin E and C consumption intentions and behaviors among factory workers based on protection motivation theory. Environ Health Prev Med 2018; 23(1):51. doi: 10.1186/s12199-018-0742-z [Crossref] [ Google Scholar]
- Kose D, Erkorkmaz U, Cinar N, Altinkaynak S. Mothers’ knowledge and attitudes about HPV vaccination to prevent cervical cancers. Asian Pac J Cancer Prev 2014; 15(17):7263-6. doi: 10.7314/apjcp.2014.15.17.7263 [Crossref] [ Google Scholar]
- Biederman E, Donahue K, Sturm L, Champion V, Zimet G. The association between maternal human Biederman E, Donahue K, Sturm L, Champion V, Zimet G The association between maternal human papillomavirus (HPV) experiences and HPV vaccination of their children. Hum Vaccin Immunother 2021; 17(4):1000-5. doi: 10.1080/21645515.2020.1817714 [Crossref] [ Google Scholar]
- Park Y, Ki M, Lee H, Lee JK, Oh JK. Parental factors affecting decision to vaccinate their daughters against human papillomavirus. Cancer Prev Res (Phila) 2023; 16(3):133-8. doi: 10.1158/1940-6207.capr-22-0412 [Crossref] [ Google Scholar]
- Dickinson C, Bumatay S, Valenzuela S, Hatch BA, Carney PA. An exploratory study of rural parents’ knowledge and attitudes about HPV vaccination following a healthcare visit with their child’s primary care provider. J Prim Care Community Health 2023; 14:21501319231201227. doi: 10.1177/21501319231201227 [Crossref] [ Google Scholar]