J Educ Community Health. 11(2):91-97.
doi: 10.34172/jech.2982
Original Article
The Impact of an Educational Program on the Stages of Change for Mammography Screening Among Rural Women with Low Health Literacy
Elhan Salehi 1  , Nasrin Ghiasi 1
, Nasrin Ghiasi 1  , Reza Pakzad 2
, Reza Pakzad 2  , Mohsen Jalilian 1, *
, Mohsen Jalilian 1, * 
Author information:
1Department of Public Health, Faculty of Health, Ilam University of Medical Sciences, Ilam, Iran
2Department of Epidemiology, Faculty of Health, Ilam University of Medical Sciences, Ilam, Iran
Abstract
Background: The aim of the study was to investigate the effect of an educational program on the mammography screening stage of change among rural women with low health literacy.
Methods: In general, 52 rural women participated in this experimental study. The samples were selected using a multi-stage cluster sampling method and divided into two intervention (n=26) and control (n=26) groups. An educational program was implemented for the intervention group for one month. The data collection tool was a valid questionnaire based on constructs of the transtheoretical model (TTM) related to mammography screening, which was completed in the pre-test phase and after three and six months. The data were analyzed using SPSS 16 at the significant level of 0.05.
Results: There was no significant difference between the control and intervention groups at the pre-test phase (P>0.05). The intervention group demonstrated considerable progress in the stage of change for mammography screening after three- and six-month follow-ups (P<0.001, odds ratio [OR]=2.54). The odds ratio of progress in the stages of change in the intervention group compared to the control group significantly increased after three (P<0.001, OR=4.29) and six (P<0.001, OR=5.45) months of follow-up. In addition, the findings indicated a significant increase in the mean scores of decisional balance, processes of change, and self-efficacy in the intervention group compared to the control group three and six months after the educational intervention (P<0.005).
Conclusion: The educational program significantly advanced mammography screening stages among rural women with low health literacy. These results highlight the program’s effectiveness in enhancing screening behaviors in this underserved population.
Keywords: Health education, Mammography, Transtheoretical model, Women
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Salehi E, Ghiasi N, Pakzad R, Jalilian M. The impact of an educational program on the stages of change for mammography screening among rural women with low health literacy. J Educ Community Health. 2024; 11(2):91-97. doi:10.34172/jech.2982
Introduction
The early detection of breast cancer (BC) almost leads to complete recovery and plays a crucial role in reducing mortality and associated complications (1). BC is one of the major leading causes of mortality among women. According to Global Cancer Statistics, in 2020, the age-standardized incidence and mortality rates for this cancer were reported as 13.3 and 7.3, respectively (2). In Iran, the incidence of BC has been rising over the past two decades. According to data from the National Cancer Registry of Iran, the number of cases is projected to increase by 63% by 2025. Furthermore, it is estimated that the number of diagnosed cases will reach 25 013 by the mentioned year (3). Considering that there is no definite way to prevent this cancer, screening for early detection is essential (4,5). Screening aims to reduce mortality rates associated with the disease (6,7). BC screening includes breast self-examination, clinical breast examination, and mammography (8). Mammography leads to a greater reduction in mortality rates compared to other screening methods (9). When the disease is confined to the breast, the chance of survival in the next five years is 75%–90%. In the second stage of the disease, the patient’s survival probability decreases by 16% (10). It is estimated that 30–35 cases of BC are detected through mammography screening (11). Current guidelines recommend mammography screening starting at the age of 40, yet many women still avoid periodic screenings (8). Although mammography rates have increased significantly in recent decades, they are still below recommended levels in many communities (12,13). Generally, the awareness of Iranian women regarding mammography and BC is not high, and they tend to consult a physician only when the disease has progressed to advanced stages (12).
Due to inadequate education and low health literacy levels, especially among rural women, there is little inclination toward undergoing mammography screening (12). Health literacy is one of the factors that influences women’s health outcomes and has been identified as a determinant of participation in screening programs in numerous studies (1,14-16). Additionally, it has been reported that other factors such as age, family history, and family support, physician recommendations, perceived sensitivity and severity, self-efficacy, and perceived benefits significantly influence the decision to undergo mammography screening (4).
Increasing knowledge, especially during the early stages of behavior change (e.g., pre-contemplation and contemplation), can be utilized as a strategy or a change process to promote mammography screening (17). Highlighting the risk of BC and understanding the perceived risks of the disease can affect decision-making balance (18).
Education is considered one of the important factors in increasing knowledge and the tendency to adapt screening behaviors for BC (19). Earlier studies have emphasized the implementation of interventions to increase knowledge and encourage women in screening programs (7,18,20). The transtheoretical model (TTM) is one of the models of behavior change that is widely used to encourage women to participate in screening programs (18,21). In this model, behavior change is considered to occur in several stages. Individuals progress through these stages by utilizing cognitive and behavioral change processes and balancing the benefits and costs of the change. Typically, these changes are accompanied by the development of self-efficacy in individuals to adopt new behaviors. Given that women’s participation in mammography screening requires balanced decision-making and overcoming related barriers and fears, the TTM can be an appropriate choice to assist them in engaging in screening programs (18,22,23). Hence, this study sought to investigate the effect of an educational program on the mammography screening stage of change among rural women with low health literacy.
Materials and Methods
Setting and Sampling
Overall, 52 rural women aged 40 years and above residing in rural areas in Dalahoo county, located in Kermanshah Province, western Iran, participated in this experimental study. The study was conducted from March to October 2023. The sample size was determined based on a similar study (24) and was calculated using the following formula:
In this study, S2p = 0.2605, μ1 = 4.56, and μ2 = 4.24 were taken into consideration. Given a confidence level of 0.95 and an error margin of 0.05, the sample size was estimated to be 19.94 participants. Considering a potential 30% dropout rate, the final sample size for each group was determined to be 26 participants.
In addition, a multi-stage cluster sampling framework was used in the sampling process. Initially, two out of six comprehensive rural health centers in Dalahoo county (Kamran and Gahvareh) were randomly selected. Using the lottery method, Gahvareh and Kamran villages were designated as the intervention and control groups, respectively.
Inclusion and Exclusion Criteria
The inclusion criteria for the study were residing in a village, being in the age range of 40–69 years, having at least an elementary level of education and low health literacy level (score of 66 or less from the health literacy for Iranian adults questionnaire) (25), being in the pre-contemplation and contemplation stages of change in the TTM, and completing an informed consent form. On the other hand, the exclusion criteria included undergoing mammography screening in the past two years, having a breast examination by a physician in the past year, performing breast self-examination at least four times (in general) in the past year, and having first-degree relatives with BC. The other exclusion criteria were suffering from or having a history of breast mass, suffering from or having a history of mental illnesses, experiencing pregnancy and lactation, and having a history of participating in BC screening education classes.
Intervention
After establishing telephone contact with eligible women for study participation, they were invited to the rural health center, where further information about the study objectives was provided to them. After completing a written informed consent form, they were enrolled in the study, and in the next step, pre-test data were collected through interviews.
A one-month educational program based on the TTM structures was designed and implemented for the intervention group. Considering that women entered the study at the precontemplation and contemplation stages, the change strategies were initially determined based on these two stages. Subsequently, to help women progress through the remaining stages, change strategies were applied based on the principles of the TTM. Educational sessions were held at the comprehensive rural health center. Educational content was prepared and tailored to the model structures using the principles of health communication. For the intervention group, 12 group education sessions plus one face-to-face midwifery counseling session were held for each individual. The face-to-face counseling was conducted by a midwife employed at the comprehensive rural health centers. The time of each session was 45 minutes. Educational posters were installed at the comprehensive rural health center hall, and educational pamphlets were distributed during group sessions. Additionally, to maintain continuous access to learning resources, a channel was created on the ITA messaging application (an Iranian messaging application), and intervention group participants were invited to join. Educational podcasts, videos, and animations related to mammography were shared on this channel. It is worth mentioning that to enhance communication with participants and the attractiveness of educational resources, the native language (Kurdish) was used in podcasts, videos, and animations. It is important to note that the educational content and media were approved by the research team prior to their use. During the implementation of the educational program, the control group received no education from the research team. In this study, the control group received the routine care and education provided by the comprehensive health service centers, and the research team imposed no restrictions on the control group’s access to these standard services. To assess the impact of the educational program, post-test data were collected three months later, and follow-up data were collected six months later through interviews. The study flow diagram is depicted in Figure 1.
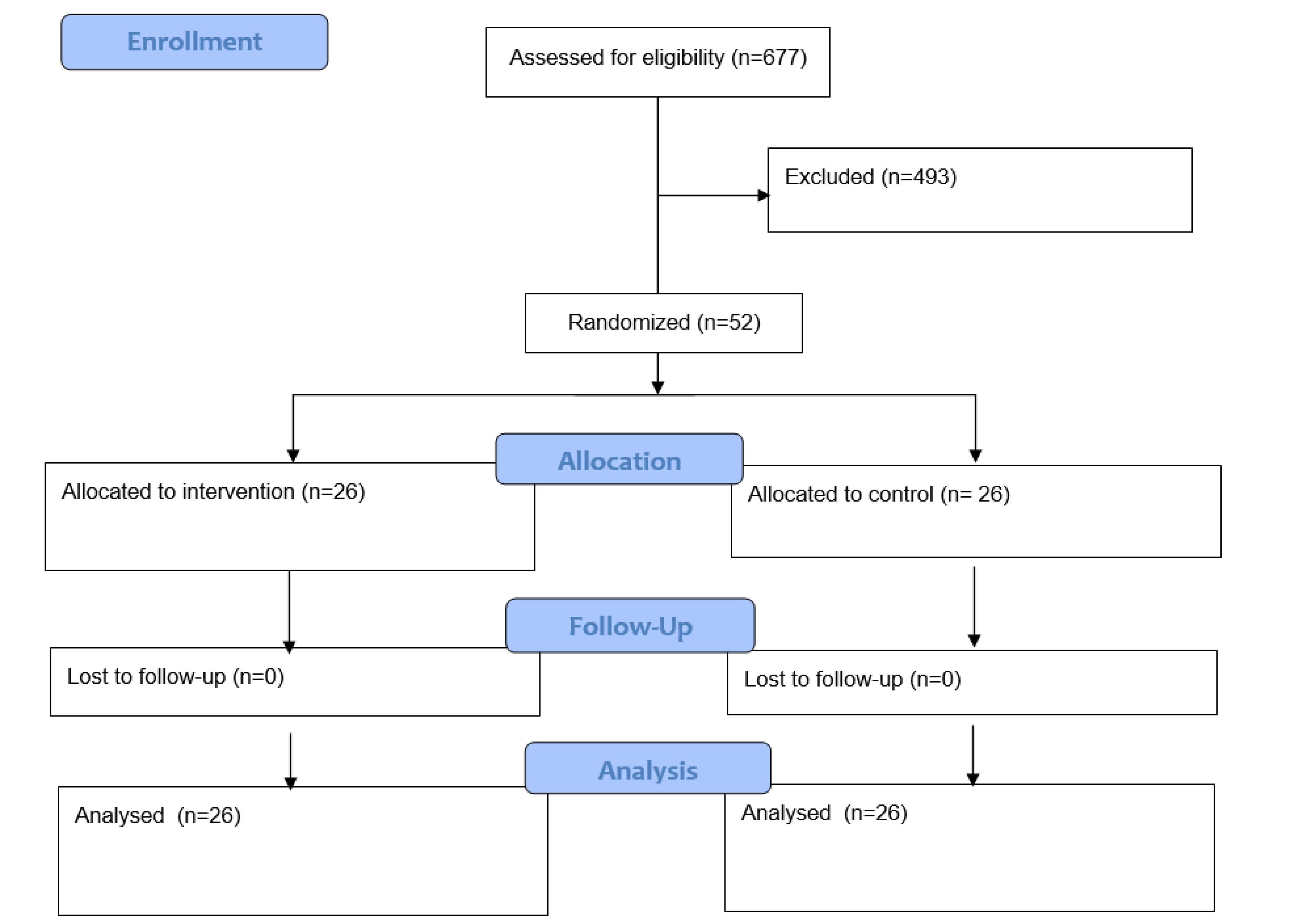
Figure 1.
Study Flow Diagram
.
Study Flow Diagram
Instruments
The data collection method in this study was the use of a questionnaire completed through interviews with participants. This questionnaire, developed by Khodayarian et al, measures the constructs of the TTM in relation to mammography screening. Its validity and reliability have been confirmed previously. This questionnaire includes an algorithm for assessing mammography screening stages of change (6 items), a decisional balance questionnaire (18 items) using a 4-point Likert-type scale (from not sure to completely sure), a 16-item cognitive and behavioral scale using a 4-point Likert-type scale (from completely agree to completely disagree), and a self-efficacy questionnaire (8 items) using a 4-point Likert-type scale (from not sure to completely sure). Higher scores indicate a better status in the respective construct (22).
Data Analysis
The data were analyzed using SPSS software, version 27. Descriptive statistics such as means, standard deviations, and analytical tests, including independent sample t-test, Fisher’s exact test, repeated measures ANOVA, and generalized estimation equation (GEE) (by considering exchangeable for the correlation structure), were used at a significance level of 5% and a confidence interval of 95%. The GEE was utilized to analyze the trend of progression in mammography screening stages of change (ordinal scale) over time in the intervention and control groups.
Results
The mean age of participants in the study was 57.86 ± 78.8 years. The mean age of the control and intervention groups was 56.5 ± 9.10 and 58.23 ± 7.92, respectively. The majority of them had education below the diploma level. More details are provided in Table 1. The homogeneity of the groups was examined using independent sample t-tests and Fisher’s exact tests. The groups did not differ significantly in the distribution of demographic variables (P > .05).
Table 1.
Demographic Characteristics of Study Participants
|
|
No. (%)
|
P
Value
|
|
Control (n=26)
|
Intervention (n=26)
|
| Number of children* |
3.57 ± 1.83 |
4.30 ± 2.22 |
0.20 |
| Education level |
Elementary |
4 (15.3) |
6 (23.06) |
0.07 |
| Secondary |
13 (50) |
13 (50) |
| Diploma |
9 (34.7) |
7 (26.94) |
| Insurance coverage |
Yes |
23 (88.5) |
25 (96.2) |
0.61 |
| No |
3 (11.5) |
1 (3.8) |
| Job |
Housewife |
24 (92.3) |
26 (100) |
0.35 |
| Employee |
2 (7.7) |
0 (0) |
Note. * Data presented as means± standard deviation.
Table 2 compares the mean scores of the constructs of the TTM in the intervention and control groups at the pre-test stage. The results of the independent sample t-test indicated that the groups did not significantly differ at the pre-test phase (P > 0.05).
Table 2.
Mean Scores of TTM Constructs in the Control and Intervention Groups at the Pre-test
|
|
Group
|
Number
|
Mean±SD
|
P
Value
|
| Decisional balance |
Control |
26 |
37.46 ± 9.5 |
0.84 |
| Intervention |
26 |
38.04 ± 12.12 |
| Cognitive process of change |
Control |
26 |
17.96 ± 5.4 |
0.84 |
| Intervention |
26 |
18.27 ± 6.1 |
| Behavioral process of change |
Control |
26 |
23.54 ± 5.91 |
0.71 |
| Intervention |
26 |
22.96 ± 5.41 |
| Self-efficacy |
Control |
26 |
14.85 ± 7.57 |
0.96 |
| Intervention |
26 |
14.77 ± 5.48 |
Note. TTM: Transtheoretical model; SD: Standard deviation.
Examination of the pre-test data revealed that all participants were in the pre-contemplation and contemplation stages of change, and no significant difference was observed between them (P = 0.48). The GEE test was utilized to consider the progress trend in the mammography screening stages of change in the two groups over time (Table 3). By considering stages of change as the dependent variable and visit time and group as predictor variables, the results of GEE demonstrated significant progress in the intervention group compared to the control group (OR = 2.54, P = 0.04). In other words, the odds ratio (OR) of transition (from the pre-contemplation phase to the preparation phase) in the intervention group was 2.54 times that in the control group. Furthermore, compared to the pre-test phase, the OR for change over the 3-month (OR = 4.29, P < 0.001) and 6-month follow-up phases (OR = 5.45, P < 0.001) significantly increased in the intervention group. In other words, the odds of transition in the 3- and 6-month follow-up phases were 4.29 and 5.45 times higher than that in the pre-test phase. This result can also be approved by marginal effects, so that the results confirmed a significant increase in the transition phase from pre-test until 6 months after the intervention (the marginal effect of visit = 1.24, P < 0.001). However, this transition further happened in the intervention group in comparison to the control group (the marginal effect of group = 1.51, P = 0.04).
Table 3.
The Trend of Mammography Screening Stages of Change in Intervention and Control Groups
|
Stage of Change
|
Control Group (n = 26)
|
Intervention Group (n = 26)
|
Time Effect (Baseline=Pre-test)
|
Group Effect
(Baseline = Control)
|
Marginal Effect
|
|
3 Months
|
6 Months
|
|
Pre-test
|
3 Months
|
6 Months
|
Pre-test
|
3 Months
|
6 Months
|
OR (95% CI)
|
P-value
|
OR (95% CI)
|
P-value
|
OR (95% CI)
|
P-value
|
Group
|
Visit
|
|
PC
|
20
(76.9) |
17
(65.4) |
17
(65.4) |
22
(84.6) |
12
(46.2) |
6
(23.1) |
4.29
(2.09 to 8.78) |
<0.001 |
5.45
(2.33 to 12.74) |
<0.001 |
2.54
(1.02 to 6.31) |
0.044 |
1.51
(p:0.042) |
1.24 (p<0.001) |
|
C
|
6
23.1) |
7
(26.9) |
8
(30.8) |
4
(15.4) |
7
(26.9) |
15
(57.7) |
|
P
|
0
(0) |
2
(7.7) |
1
(3.8) |
0
(0) |
7
(26.9) |
5
(19.2) |
PC: Pre-contemplation; C: Contemplation; P: Preparation
The repeated measures test indicated a significant increase in the mean scores of the TTM constructs over time in the intervention group compared to the control group (P< 0.05, Table 4).
Table 4.
Mean Scores of the TTM Constructs in the Control and Intervention Groups at Pre-test, 3 Months, and 6 Months
|
|
Group
|
Number
|
Pre-test
|
3 Months
|
6 Months
|
Within-subject
|
Between-subject
|
Interaction
|
| Decisional balance |
Control |
26 |
37.46 ± 9.5 |
40.85 ± 8.35 |
41.65 ± 7.76 |
F = 122.75;
df = 1.35/67.67;
P < 0.001 |
F = 10.45;
df = 1/50;
P = 0.002 |
F = 43.512;
df = 1.35/67.67;
P < 0.001 |
| Intervention |
26 |
38.04 ± 12.12 |
49 ± 7.97 |
55.04 ± 4.95 |
| Cognitive process of change |
Control |
26 |
17.96 ± 5.4 |
19.08 ± 3.7 |
19.88 ± 3.75 |
F = 77.27;
df = 1.31/65.68;
P < 0.001 |
F = 19.12
df = 1/50
P < 0.001 |
F = 34.48;
df = 1.31/65.68;
P < 0.001 |
| Intervention |
26 |
18.27 ± 6.1 |
25.12 ± 3.18 |
27.42 ± 2.28 |
| Behavioral process of change |
Control |
26 |
23.54 ± 5.91 |
23.62 ± 4.92 |
23.85 ± 4.57 |
F = 18.62;
df = 1.21/60.67;
P < 0.001 |
F = 0.62
df = 1/50
P = 0.43 |
F = 12.96;
df = 1.21/60.67;
P < 0.001 |
| Intervention |
26 |
22.96 ± 5.41 |
24.92 ± 4.27 |
26.19 ± 3.58 |
| Self-efficacy |
Control |
26 |
14.85 ± 7.57 |
16.54 ± 6.78 |
15.96 ± 5.65 |
F = 63.89;
df = 1.49/74.41;
P < 0.001 |
F = 5.65;
df = 1/50;
P = 0.02 |
F = 35.73;
df = 1.49/74.41;
P < 0.001 |
| Intervention |
26 |
14.77 ± 5.48 |
19.81 ± 3.39 |
23.23 ± 3.27 |
Discussion
This study examined the impact of an educational intervention based on the TTM on the stages of change for mammography screening in rural women with low health literacy. Significant progress was observed in the stages of mammography screening behavior change in the intervention group over time. This progress was evident in a significantly increased odds ratio of change over time after 3 and 6 months in this group and was positively correlated with an increase in the number of individuals in the preparation stage for mammography screening. Considering the significant difference between the control and intervention groups in the progress of change stages, it appears that the educational program succeeded in targeting enabling and reinforcing factors of change and guiding individuals to the preparation stage. Overall, our findings align with those of previous research in this area. For instance, Khodayarian et al reported that a TTM-based intervention could effectively promote Pap smear testing among women aged 18–65 years, facilitating their progression from the pre-contemplation and contemplation stages to the preparation stage (22). Additionally, Pirzadeh et al documented a 97% progress rate in the stages of Pap smear screening in married women (26). Furthermore, Lee-in et al concluded that an educational intervention significantly improved the stage of change in mammography screening 3 and 6 months post-intervention in mammography non-adherent Chinese women (27).
Our findings demonstrated a significant increase in decisional balance regarding mammography screening in the intervention group compared to the control group. It seems that adopting educational strategies to introduce the benefits of mammography and its future advantages could shift individuals’ mental balance toward the decision to undergo mammography. Additionally, providing strategies to overcome barriers was effective in facilitating this change. Correcting misconceptions, as one of the major barriers to participation in mammography screening programs, also contributed to the success of the intervention group. This finding is consistent with the results of previous studies. For example, Duarte found that encouragement and motivational messages significantly reduced barriers to free mammography screening among women (28). Conversely, Hajian et al reported that a health belief model-based intervention did not successfully address barriers related to mammography screening behavior (29). The difference in findings may stem from attention to individuals’ stages of change and the use of stage-specific processes of change in the current study.
The adaptation of cognitive and behavioral processes of change increased over time among women in the intervention group. This progression was consistent with advances in the stages of change. Cognitive and behavioral processes of change facilitated the transition through stages of change and enhanced women’s movement toward the decision to undergo mammography screening, which aligns with those of some earlier studies (30-32). In the educational session, details of each change process were provided to the intervention group, aiming to familiarize women with change strategies and empower them to make decisions regarding mammography screening. Overall, it is presumed that, in this study, special attention to providing educational content tailored to the details of processes of change improved these constructs in women in the intervention group compared to the control group.
In general, the effectiveness of the educational approach used in this study on the self-efficacy of women in the intervention group in deciding to undergo mammography screening was evident. Implemented strategies included breaking behavior into smaller steps, introducing individuals who had previously undergone mammography screening, and providing verbal encouragement for mammography screening. Secginli and Nahcivan reported increased confidence in breast self-examination six months after a health promotion program related to BC screening behaviors among Turkish women (33). Davis et al also demonstrated increased self-efficacy in mammography screening among women aged 40 and above after an educational intervention (34). Similarly, Tuzcu et al found increased self-efficacy among immigrant women in Turkey regarding BC screening in the intervention group compared to the control group 3 and 6 months post-intervention (35). On the other hand, these results are not consistent with the findings of some other studies.
A study on cancer screening behaviors in women revealed that a specific educational intervention did not significantly enhance self-efficacy in the participants, despite other positive outcomes related to knowledge and attitudes toward screening.
The consistency of our findings with previous studies confirms the effectiveness of the strategies used to increase self-efficacy in women in the intervention group.
Conclusion
The results of the present study revealed that interventions based on the TTM can have a positive impact on women’s stage of change to undergo mammography screening. Activating change processes appropriate to the stage of change has significantly encouraged rural women with low health literacy to effectively participate in mammography screening programs. Moreover, assisting these individuals in creating a suitable balance between the pros and cons of mammography screening and reinforcing their self-efficacy led to significant progress in the stages of change in the intervention group compared to the control group 3 and 6 months post-intervention.
Strengths and Limitations
The strength of this study was providing intervention to rural women with low health literacy and in inactive stages of change to mammography screening. Additionally, the processes of change strategies, especially cognitive processes, were utilized to assist women in the upward stage of change. Changes in the structures of the theoretical model 3 and 6 months after the educational program for the long-term evaluation of intervention effects were another strength. Conversely, the limitation was the lack of sufficient resources, such as financial support and time for continued study and assessment of long-term effects over at least one year.
Although the control group in this study exhibited no significant improvement in the variables under investigation, it is important to acknowledge that the nature of education-focused intervention studies inherently carries the risk of information transfer from the intervention group to the control group. As a result, the inability to fully control conditions to prevent the potential spillover of intervention effects to the control group represents a notable limitation of this study.
Acknowledgements
The authors appreciate the participation of rural women in this study.
Authors’ Contribution
Conceptualization: Mohsen Jalilian, Nasrin Ghiasi.
Data curation: Elham Salehi, Reza Pakzad, Mohsen Jalilian.
Formal analysis: Reza Pakzad, Mohsen Jalilian.
Funding acquisition: Elham Salehi, Nasrin Ghiasi, Reza Pakzad, Mohsen Jalilian.
Investigation: Elham Salehi, Mohsen Jalilian.
Methodology: Mohsen Jalilian, Nasrin Ghiasi.
Project administration: Mohsen Jalilian, Nasrin Ghiasi.
Resources: Mohsen Jalilian, Nasrin Ghiasi, Elham Salehi.
Software: Elham Salehi.
Supervision: Mohsen Jalilian, Nasrin Ghiasi.
Validation: Mohsen Jalilian, Nasrin Ghiasi, Elham Salehi.
Visualization: Mohsen Jalilian, Reza Pakzad.
Writing–original draft: Mohsen Jalilian, Nasrin Ghiasi, Reza Pakzad.
Writing–review & editing: Mohsen Jalilian, Reza Pakzad.
Competing Interests
There was no conflict of interests.
Ethical Approval
This study was approved by the Ethics Committee of Ilam University of Medical Sciences (IR.MEDILAM.REC.1401.102). Its code of ethics is available from: https://ethics.research.ac.ir/IR.MEDILAM.REC.1401.102.
Funding
This research project was financially supported by Ilam University of Medical Sciences.
References
- Gunn CM, Maschke A, Paasche-Orlow MK, Kressin NR, Schonberg MA, Battaglia TA. Engaging women with limited health literacy in mammography decision-making: perspectives of patients and primary care providers. J Gen Intern Med 2021; 36(4):938-45. doi: 10.1007/s11606-020-06213-2 [Crossref] [ Google Scholar]
- Kavousi S, Maharlouei N, Rezvani A, Akbari Aliabad H, Molavi Vardanjani H. Worldwide association of the gender inequality with the incidence and mortality of cervical, ovarian, endometrial, and breast cancers. SSM Popul Health 2024; 25:101613. doi: 10.1016/j.ssmph.2024.101613 [Crossref] [ Google Scholar]
- Haghighat S, Omidi Z, Ghanbari-Motlagh A. Trend of breast cancer incidence in Iran during a fifteen-year interval according to national cancer registry reports. Iran J Breast Dis 2022; 15(2):4-17. doi: 10.30699/ijbd.15.2.4.[Persian] [Crossref] [ Google Scholar]
- Kalan Farmanfarma K, Mahdavifar N, Heidarpour Kiasara S, Hassanipour S, Salehiniya H. Determinants of mammography screening in Iranian women: a systematic review and meta-analysis. Breast Dis 2022; 41(1):279-94. doi: 10.3233/bd-210037 [Crossref] [ Google Scholar]
- Soltanahmadi Z, Abbaszadeh A, Tirgari B. A survey on the rate and causes of women’s participation or nonparticipation in breast and cervical cancers screening programs. Iran J Obstet Gynecol Infertil 2010; 13(3):37-46. doi: 10.22038/ijogi.2010.5855.[Persian] [Crossref] [ Google Scholar]
- Tilstra S, McNeil M. New developments in breast cancer screening and treatment. J Womens Health (Larchmt) 2017; 26(1):5-8. doi: 10.1089/jwh.2016.6197 [Crossref] [ Google Scholar]
- van der Waal D, Ripping TM, Verbeek AL, Broeders MJ. Breast cancer screening effect across breast density strata: a case-control study. Int J Cancer 2017; 140(1):41-9. doi: 10.1002/ijc.30430 [Crossref] [ Google Scholar]
- Ren W, Chen M, Qiao Y, Zhao F. Global guidelines for breast cancer screening: a systematic review. Breast 2022; 64:85-99. doi: 10.1016/j.breast.2022.04.003 [Crossref] [ Google Scholar]
- Busakhala NW, Chite FA, Wachira J, Naanyu V, Kisuya JW, Keter A. Screening by clinical breast examination in Western Kenya: who Comes?. J Glob Oncol 2016; 2(3):114-22. doi: 10.1200/jgo.2015.000687 [Crossref] [ Google Scholar]
- Rasoli Z, Farhadifar F, Taymoori P, Shahgheibi S, Seyedoshohadaei F, Shahsavari S. Effects of three educational intervention methods on repeated mammography among non-adherent women in Sanandaj. Sci J Kurdistan Univ Med Sci 2016; 20(6):116-25. doi: 10.22102/20.6.116.[Persian] [Crossref] [ Google Scholar]
- Kalan-Farmanfarma K, Zareban I, Jalili Z, Shahrakipour M. Effectiveness of education based on the health belief model on performing preventive measures for breast cancer among female teachers in Zahedan. J Educ Community Health 2014; 1(1):11-8. doi: 10.20286/jech-010111 [Crossref] [ Google Scholar]
- Fransen MP, Van Schaik TM, Twickler TB, Essink-Bot ML. Applicability of internationally available health literacy measures in the Netherlands. J Health Commun 2011; 16 Suppl 3:134-49. doi: 10.1080/10810730.2011.604383 [Crossref] [ Google Scholar]
- Sun Y, Sarma EA, Moyer A, Messina CR. Promoting mammography screening among Chinese American women using a message-framing intervention. Patient Educ Couns 2015; 98(7):878-83. doi: 10.1016/j.pec.2015.03.021 [Crossref] [ Google Scholar]
- Rakhshani T, Khiyali Z, Mirzaei M, Kamyab A, Khani Jeihooni A. Health literacy and breast and cervical cancer screening behaviors in women. J Educ Community Health 2023; 10(2):87-92. doi: 10.34172/jech.2023.A-10-110-16 [Crossref] [ Google Scholar]
- Ranjbaran S, Maleki Chollou K, Babazadeh T. Assessment of health literacy and health promoting behaviors among the urban adult population. Ethiop J Health Sci 2022; 32(5):985-92. doi: 10.4314/ejhs.v32i5.14 [Crossref] [ Google Scholar]
- Rezaee N, Seraji M. Relationship between health literacy and self-care in heart failure patients. J Health Lit 2019; 4(1):18-24. doi: 10.22038/jhl.2019.39135.1044 [Crossref] [ Google Scholar]
- Rademaker C. Evaluation of a Process Change on Mammography Screening Rates in a Family and Community Medicine Clinic. 2022. DNP Projects. 382. Available from: https://uknowledge.uky.edu/dnp_etds/382.
- Tung WC, Chen Y. Breast cancer knowledge and mammography use among Asian American women aged 40 and older: using the transtheoretical model approach. J Immigr Minor Health 2024; 26(1):140-7. doi: 10.1007/s10903-023-01529-7 [Crossref] [ Google Scholar]
- Early J, Armstrong SN, Burke S, Thompson DL. US female college students’ breast health knowledge, attitudes, and determinants of screening practices: new implications for health education. J Am Coll Health 2011; 59(7):640-7. doi: 10.1080/07448481.2010.528098 [Crossref] [ Google Scholar]
- Hazavehei SM, Ezzati-Rastegar K, Dogonchi M, Salimi N, Gheisvandi E. The impact of educational intervention programs to promoting mammography screening: a systematic review. J Educ Community Health 2016; 3(1):58-67. doi: 10.21859/jech-03018 [Crossref] [ Google Scholar]
- de Menezes MC, Mingoti SA, Cardoso CS, de Deus Mendonça R, Lopes AC. Intervention based on transtheoretical model promotes anthropometric and nutritional improvements - a randomized controlled trial. Eat Behav 2015; 17:37-44. doi: 10.1016/j.eatbeh.2014.12.007 [Crossref] [ Google Scholar]
- Khodayarian M, Farajkhoda T, Aryaeenezhad A, Sharifi M. Predicting factors of mammography adherence among Iranian women based on transtheoretical model. J Res Dev Nurs Midwifery 2020; 17(2):28-31. doi: 10.29252/jgbfnm.17.2.28 [Crossref] [ Google Scholar]
- Farajzadegan Z, Fathollahi-Dehkordi F, Hematti S, Sirous R, Tavakoli N, Rouzbahani R. The transtheoretical model, health belief model, and breast cancer screening among Iranian women with a family history of breast cancer. J Res Med Sci 2016; 21:122. doi: 10.4103/1735-1995.193513 [Crossref] [ Google Scholar]
- Fernández ME, Gonzales A, Tortolero-Luna G, Williams J, Saavedra-Embesi M, Chan W. Effectiveness of Cultivando la Salud: a breast and cervical cancer screening promotion program for low-income Hispanic women. Am J Public Health 2009; 99(5):936-43. doi: 10.2105/ajph.2008.136713 [Crossref] [ Google Scholar]
- Montazeri A, Tavousi M, Rakhshani F, Azin SA, Jahangiri K, Ebadi M, et al. Health Literacy for Iranian Adults (HELIA): development and psychometric properties. Payesh 2014;13(5):589-99. [Persian].
- Pirzadeh A, Amidi Mazaheri M. The effect of education on women’s practice based on the health belief model about Pap smear test. Int J Prev Med 2012; 3(8):585-90. [ Google Scholar]
- Lee-Lin F, Nguyen T, Pedhiwala N, Dieckmann NF, Menon U. A longitudinal examination of stages of change model applied to mammography screening. West J Nurs Res 2016; 38(4):441-58. doi: 10.1177/0193945915618398 [Crossref] [ Google Scholar]
- Duarte F. Encouraging mammograms using behavioral economics: a randomized controlled trial in Chile. Value Health 2021; 24(10):1463-9. doi: 10.1016/j.jval.2021.04.1275 [Crossref] [ Google Scholar]
- Hajian S, Vakilian K, Mirzaii Najabadi K, Hosseini J, Mirzaei HR. Effects of education based on the health belief model on screening behavior in high-risk women for breast cancer, Tehran, Iran. Asian Pac J Cancer Prev 2011; 12(1):49-54. [ Google Scholar]
- Li X, Yang S, Wang Y, Yang B, Zhang J. Effects of a transtheoretical model-based intervention and motivational interviewing on the management of depression in hospitalized patients with coronary heart disease: a randomized controlled trial. BMC Public Health 2020; 20(1):420. doi: 10.1186/s12889-020-08568-x [Crossref] [ Google Scholar]
- van Ravesteijn HJ, Suijkerbuijk YB, Langbroek JA, Muskens E, Lucassen PL, van Weel C. Mindfulness-based cognitive therapy (MBCT) for patients with medically unexplained symptoms: process of change. J Psychosom Res 2014; 77(1):27-33. doi: 10.1016/j.jpsychores.2014.04.010 [Crossref] [ Google Scholar]
- Wen SL, Li J, Wang AN, Lv MM, Li HY, Lu YF. Effects of transtheoretical model-based intervention on the self-management of patients with an ostomy: a randomised controlled trial. J Clin Nurs 2019; 28(9-10):1936-51. doi: 10.1111/jocn.14731 [Crossref] [ Google Scholar]
- Secginli S, Nahcivan NO. The effectiveness of a nurse-delivered breast health promotion program on breast cancer screening behaviours in non-adherent Turkish women: a randomized controlled trial. Int J Nurs Stud 2011; 48(1):24-36. doi: 10.1016/j.ijnurstu.2010.05.016 [Crossref] [ Google Scholar]
- Davis TC, Rademaker A, Bennett CL, Wolf MS, Carias E, Reynolds C. Improving mammography screening among the medically underserved. J Gen Intern Med 2014; 29(4):628-35. doi: 10.1007/s11606-013-2743-3 [Crossref] [ Google Scholar]
- Tuzcu A, Bahar Z, Gözüm S. Effects of interventions based on health behavior models on breast cancer screening behaviors of migrant women in Turkey. Cancer Nurs 2016; 39(2):E40-50. doi: 10.1097/ncc.0000000000000268 [Crossref] [ Google Scholar]