J Educ Community Health. 11(2):118-125.
doi: 10.34172/jech.2986
Review Article
Medication Adherence Among Older People With Hypertension in Southeast Asia: A Scoping Review
Andi Fitrah Ramadhanty 1, 2  , Andi Masyitha Irwan 3, *
, Andi Masyitha Irwan 3, *  , Andina Setyawati 2
, Andina Setyawati 2
Author information:
1Nursing Program, Faculty of Nursing, Hasanuddin University, Makassar, Indonesia
2Medical Surgical Nursing Department, Faculty of Nursing, Hasanuddin University, Makassar, Indonesia
3Gerontological Nursing Department, Faculty of Nursing, Hasanuddin University, Makassar, Indonesia
Abstract
Background: Medication adherence (MA) is a crucial factor in effectively managing hypertension (HTN). Southeast Asia (SEA) is one of the regions with a significant burden of HTN. Understanding MA among patients with HTN is vital to identifying gaps and potential strategies to enhance its use and effectiveness for this region. However, little is known about MA among this population. This review study aimed to identify MA strategies implemented in previous studies on older people with HTN in SEA.
Methods: This scoping review was conducted from 2013 to 2023 by searching the Global Medicus Index, PubMed, ScienceDirect, EBSCO, CINAHL, Wiley, Garuda, and Google Scholar and grey literature to identify the aims of this paper using keyword variations such as "elderly" OR "older people" AND "hypertension" OR "Hypertensive" OR high blood pressure" AND "medication adherence" OR "medication compliance" AND "southeast Asia". Three reviewers independently examined the results, and the extracted data were then organized, categorized, and summarized.
Results: Out of 742 studies reviewed, 16 met the criteria and were included in this review. The evidence indicated that MA rates among older people with HTN in several countries in SEA were considered poor, with various reasons for non-adherence. Family support and level of knowledge were found to be the most common supportive factors for MA. Some studies demonstrated negative perceptions toward medication, with previous reviews reporting the use of herbal medicine as self-treatment due to fear of side effects of prescribed medications.
Conclusion: The level of adherence to prescribed medication among older people is considered low in the reviewed studies. The main reasons for non-adherence are negative perceptions toward prescribed medication, which were also expressed in some studies. Moreover, various efforts were made by individuals to improve their adherence to medication use.
Keywords: Medication adherence, Hypertension, Older people, Southeast Asia
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Ramadhanty AF, Irwan AM, Setyawati A. Medication adherence among older people with hypertension in Southeast Asia: a scoping review. J Educ Community Health. 2024; 11(2):118-125. doi:10.34172/jech.2986
Introduction
Hypertension (HTN) is a leading risk factor for non-communicable diseases such as heart disease, stroke, and other cardiovascular conditions, which are significant causes of mortality globally. Anti-hypertensive medications can effectively reduce blood pressure and the risk of these associated diseases (1). However, despite the efficacy, affordability, and availability of anti-hypertensive drugs, overall HTN control in the general population is still less than 60% (2).
The American Heart Association defines HTN as systolic blood pressure > 130 mm Hg and/or diastolic blood pressure > 80 mm Hg (3). The World Health Organization reports that HTN prevalence varies by region and income group. The African region has the highest prevalence (27%), while the Americas have the lowest prevalence (18%). Based on specific regions, the World Health Organization data shows the prevalence of HTN in Africa, Southeast Asia (SEA), and the Americas to be 40%, 36%, and 35%, respectively, and about 60–80% are 65 years old (4). In Southeast Asian countries, the prevalence of HTN has significantly increased over the last two decades (5). Its prevalence remains quite high globally, and the incidence rate increases with age (6). A recent study has reported that there is a one-third increase in the population of HTN in SEA every year (7). The rising prevalence of HTN in Asian countries, driven by Western lifestyles, modernization, and urbanization, has made HTN control a significant public health challenge (8).
One way to control HTN is by taking medication regularly and at the recommended dosage prescribed by a doctor. Medication adherence (MA) can be defined as the process in which patients take their medication as prescribed (9). Low adherence leads to resistance to HTN treatment (10). In older people, the use of antihypertensive drugs has led to a decrease in overall cardiovascular disease, morbidity rates, and mortality rates in individuals with HTN (11). The main cause of uncontrolled blood pressure in older people is non-adherence to treatment, either intentional or unintentional (12). Older people with chronic diseases tend to exhibit poor MA compared to young adults (13). This results in more serious complications and impacts the quality of life of older people, such as increased morbidity, mortality, and additional costs for the healthcare system (14–16).
Several reviews have reported that the use and effectiveness of herbal remedies for HTN, fear of side effects from prescribed medications, and easier access are reasons for choosing herbal remedies (17). However, they only focus on self-care management without emphasizing the overview of MA for HTN at present (17). Furthermore, Pinho et al (18) reported MA in patients with HTN, focusing only on the interventions applied rather than the older people with HTN. Then, a review conducted by Nawi et al (7) demonstrated the prevalence and risk factors of HTN in the SEA region but only focused on urban areas.
Understanding the overview of MA among older people with HTN is crucial for identifying gaps and potential strategies to strengthen its effectiveness and use in the SEA region. However, little is known about the MA overview in this population. Therefore, this review was conducted to present an overview of MA among older people with HTN in SEA by exploring factors influencing adherence, differences in HTN management approaches, and initiatives implemented to improve adherence. The findings can contribute to a better understanding of this health challenge in the region and support efforts to improve HTN management in the older population.
Objectives
The aim of this paper is to identify MA strategies that have been implemented in several previous studies on older people suffering from HTN in SEA.
Materials and Methods
This scoping review systematically synthesizes research evidence on MA strategies for older people with HTN in SEA, even though it has different objectives and methods (19). The method or framework used in this scoping review is the Arksey and O’Malley framework (20), which consists of five steps to explain and facilitate each stage of the framework.
Stage 1: Identifying the Research Question
The research question of this scoping review is as follows:
What is the overview of MA among older people with HTN in SEA? The countries in SEA include Brunei, Malaysia, Indonesia, Thailand, Singapore, the Philippines, Vietnam, Laos, Cambodia, Myanmar, and East Timor.
Stage 2: Identifying Relevant Studies and Search Terms
After identifying the scoping review question, this review followed a search strategy guided by Joanna Briggs Institute (21) to describe MA among older people with HTN in SEA. The next step was to identify relevant articles by determining keywords and phrases used in the search. Overall, 8 databases were utilized for this scoping review, including Global Medicus Index, PubMed, ScienceDirect, EBSCO, CINAHL, Wiley, Garuda, and Google Scholar. An initial search was conducted by extracting titles, abstracts, and content to identify keyword terms. Keywords used for each database are presented in Table 1.
Table 1.
The Keywords Used in This Search
|
No.
|
Database
|
Keywords
|
Article Obtained
|
Date of Access
|
| 1 |
Global Medicus Index |
Elderly OR older people AND high blood pressure OR hypertension OR hypertensive AND medication adherence |
9 |
October 17, 2023 |
| 2 |
PubMed |
((((Elderly[MeSH Terms]) OR (older people[Title/Abstract])) AND (((high blood pressure[MeSH Terms]) OR (hypertension[Title/Abstract])) OR (hypertensive[Title/Abstract]))) AND ((medication adherence[MeSH Terms]) OR (medication compliance[MeSH Terms]))) AND ((southeast Asia[MeSH Terms])) |
11 |
October 17, 2023 |
| 3 |
ScienceDirect |
((((Elderly[MeSH Terms]) OR (older people[Title/Abstract])) AND (((high blood pressure[MeSH Terms]) OR (hypertension[Title/Abstract])) OR (hypertensive[Title/Abstract]))) AND ((medication adherence[MeSH Terms]) OR (medication compliance[MeSH Terms]))) AND ((southeast Asia[MeSH Terms])) |
69 |
October 17, 2023 |
| 4 |
EBSCO |
TX (elderly or older people) AND TX (hypertension or high blood pressure or hypertensive) AND TX (medication adherence or medication compliance) AND TX southeast Asia |
60 |
October 18, 2023 |
| 5 |
CINAHL |
(Elderly):ti,ab,kw OR (older people):ti,ab,kw AND (“hypertension”):ti,ab,kw OR (“hypertensive”):ti,ab,kw OR (“high blood pressure”):ti,ab,kw AND (“medication therapy management”):ti,ab,kw OR (medication adherence):ti,ab,kw OR (“compliance”):ti,ab,kw AND (“Southeast Asian”):ti,ab,kw |
389 |
October 18, 2023 |
| 6 |
Wiley |
“Elderly OR older people” and “hypertension OR hypertensive OR high blood pressure” and “medication adherence OR medication compliance” and “southeast Asia, anywhere” |
92 |
October 18, 2023 |
| 7 |
Garuda |
Lansia AND hipertensi OR tekanan darah tinggi OR tekanan darah AND Kepatuhan OR Kepatuhan minum obat, by abstract |
7 |
October 19, 2023 |
| 8 |
Google Scholar |
“Lansia” DAN “Hipertensi” ATAU “tekanan darah tinggi” DAN “kepatuhan minum obat” ATAU “kepatuhan” DAN “Asia tenggara” |
163 |
October 19, 2023 |
Additionally, we searched for other references that, in the authors’ assessment, were related to this review on Google Scholar, as these references may have been missed in the search process in previous databases. The initial search was conducted by extracting titles, abstracts, and content to identify other terms and keywords, including alternative options that were relevant to other contexts and cultures.
The inclusion and exclusion criteria for this paper were based on the Population Concept Context (21). The population in this review included older people diagnosed with HTN according to the age limit specified in the country where the study was conducted. This review has focused on qualitative and quantitative primary data studies, including those collecting original data via interviews, surveys, or experiments. Review articles, study protocols, intervention studies, and populations with pregnancy-induced HTN were excluded from the investigation. The search was limited to full-text articles published in English and Indonesian from 2013 to 2023, as the incidence of HTN has increased in the last ten years. Ten years was determined as the time limit of the search, as that marks the recent increase in the prevalence of HTN in SEA countries (22). English is the principal language in global scientific communication. The majority of international scientific publications are written in English. Furthermore, articles in both English and Indonesian are more accessible to researchers through international and national databases.
Table 1 provides keywords and phrases used in the search. In addition, references were searched in Google Scholar for additional articles that may have been missed in previous database searches by using BOOLEAN phrases and medical subject heading (MeSH) terms with keyword variations such as “elderly” OR “older people” AND “hypertension” OR “Hypertensive” OR “high blood pressure” AND “medication adherence” OR “medication compliance” AND “Southeast Asia”.
Stage 3: Study Selection and Extraction
Figure 1 shows the process and results of screening articles using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart and manuscript extraction criteria after the initial search based on the inclusion and exclusion criteria of the study. In summary, 807 relevant articles were collected from 8 databases. After removing duplicates, 742 articles remained. The next step was to screen articles based on titles/abstracts, resulting in 84 articles for full-text screening. After full-text screening, 37 articles were eligible, and based on the inclusion criteria, 16 articles were relevant to the research question and included for analysis. Three reviewers (AFR, AMI, and AS) independently examined the results, and the extracted data were then organized, classified, and summarized.
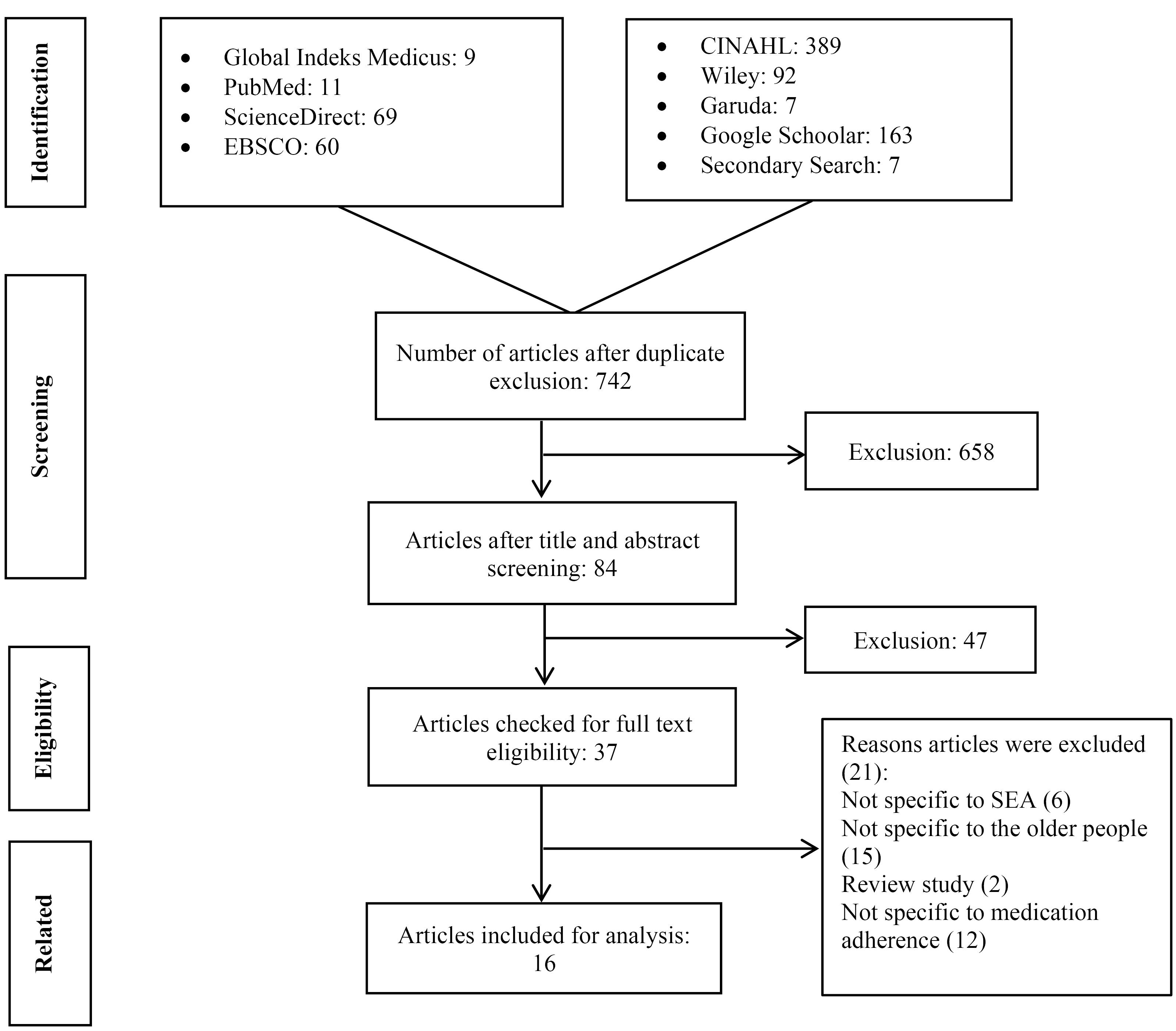
Figure 1.
Flow Diagram of the Study Selection Process
.
Flow Diagram of the Study Selection Process
Evaluation of Quality of Articles
All articles identified from the article search were imported into the Mendeley reference manager software and exported after de-duplication to the Rayyan Software Program (23). To ensure reliability among reviewers, two reviewers (AMI and AFR) were assigned to screen 25 English-language articles for titles, abstracts, and full texts using the Joanna Briggs Institute Manual method. There was disagreement in 8% of the articles, which was resolved through reviewer discussion to achieve 100% agreement at each screening stage.
Stage 4: Data Mapping
The data were independently extracted using the Rayyan Software Program and Mendeley and then compiled into tables based on the included items. Next, the studies were filtered to report the overview of MA among people with HTN in SEA. The characteristics of each study and the research methods were described and presented in table form. Factors influencing MA were presented as reported by the authors. The measured variables are listed in Table S1 (Supplementary file 1).
Stage 5: Organizing, Summarizing, and Reporting Results
The results of this review are reported through descriptive analysis and a narrative summary of the findings using text and tabulation, based on the stages of the method or framework of the Arksey and O’Malley scoping review method (20).
Results
Characteristics of Studies
Out of 37 articles checked for full-text eligibility, 21 were excluded for different reasons. Six articles were not specific to SEA, 15 did not focus on older people, 2 were review studies, and 12 were not specific to MA. Therefore, 16 articles were included for analysis; more than half (10) were conducted in Indonesia (24-33), 3 in Thailand (34-36), 2 in Myanmar (37,38), and 1 in Malaysia (39). However, for other SEA countries such as Vietnam, Singapore, the Philippines, Laos, Brunei, Cambodia, and East Timor, the authors found no articles that matched the keywords. Tables S1 and S2 present quantitative and qualitative studies of MA, respectively. The largest sample from the included studies was found in a study conducted in Thailand, with a total of 600 participants (34). In other studies, the sample sizes ranged from 5 to 410. Regarding the study settings, among quantitative studies, six were conducted in rural areas (24,25,27,30,37,38) and six were performed in urban areas (26,28,31,34,35,40). For qualitative studies, two were conducted in rural areas (32,36), and two were performed in urban areas (33,39). Overall, the ages of the participants in these studies ranged from 45 to 90 years old.
Medication Adherence Among Older People With Hypertension
In the included studies, both quantitative (24-28,30,31,34,35,37-40) and qualitative (32,33,36,39) studies indicated that older people with HTN still have poor adherence levels, with the most common reasons cited in quantitative studies being a lack of family support (24-26,30), knowledge levels (24-27,30,31,40), and age (24,37,38).
As for qualitative studies, the majority of the participants explored reasons for non-adherence to medication and factors that support and motivate them to improve their MA. Overall, two studies reported the use of herbal remedies as substitutes for antihypertensive drugs (32,39), and several studies showed negative perceptions toward the antihypertensive drugs consumed (31,35,36,38,39).
Factors Supporting and Inhibition
In the reviewed studies, several factors were identified as supporting or hindering MA among older people with HTN. These factors are described in the article text as examples of statements from participants found in the studies (Table S2). These factors were further categorized into individual, environmental, and social groups (Figure 2). Individual factors are those under the control or influence of the individual, while environmental and social factors are those influenced by the individuals’ household environment or the community where they reside.
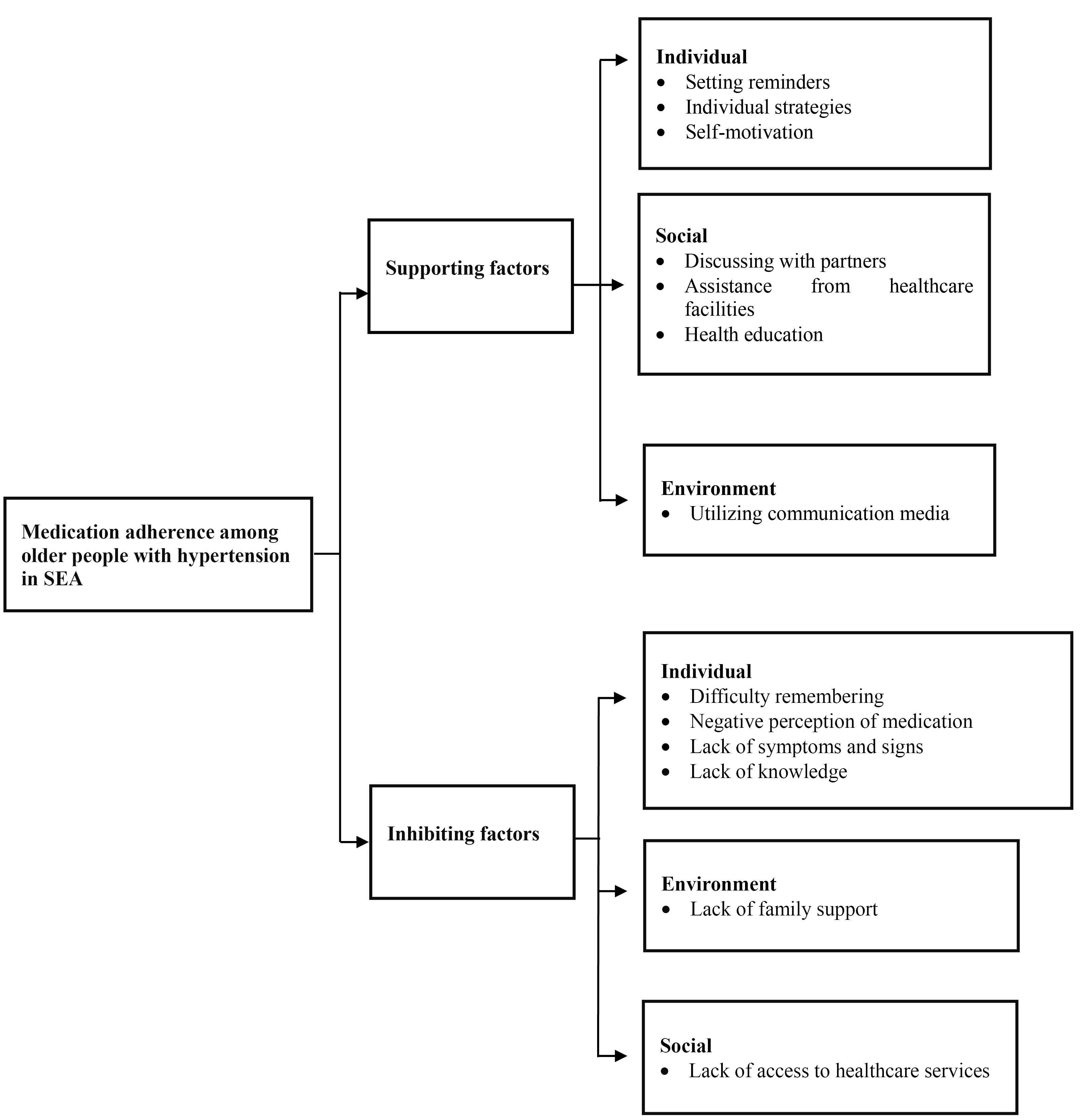
Figure 2.
Framework of Medication Adherence Among Older People With Hypertension: Supporting and Inhibiting Factors in Southeast Asia
.
Framework of Medication Adherence Among Older People With Hypertension: Supporting and Inhibiting Factors in Southeast Asia
Among statements described in the studies, “setting reminders” (33,39), “personal strategies” (39), and “self-motivation” (33) are considered individual supporting factors. In addition, “discussing with a partner” (39), “healthcare facility assistance” (39), and “health education” (36,39) are regarded as social supporting factors, and “utilizing communication media” (33,39) is considered an environmental supporting factor. On the other hand, “difficulty remembering” (33,36,39), “negative perceptions of medication” (36,39), “lack of symptoms and signs” (32,36), and “lack of knowledge” (32,39) are grouped as individual hindering factors. Further, “lack of family support” (33) and “lack of access to healthcare services” (32,39) are considered environmental hindering and social hindering factors, respectively.
Discussion
This review mainly aimed to present an overview of MA among older people with HTN in the SEA region by exploring factors influencing adherence, differences in HTN management approaches, and initiatives implemented to improve adherence. The presented evidence revealed that MA among older people with HTN in several SEA countries is considered quite poor, with various reasons for non-adherence. Other parts of Asia showed similar trends, with South Asia (48%) followed by East Asia (45%) and the Middle East (41%) (41). Family support and knowledge levels were the most common supporting factors for MA identified in this review. In Latvia, 61.4% of respondents felt confident about their medications, while others were unsure about the necessity, safety, and effectiveness of the medications or the severity of their illness (42). In China, 31.1% of patients adhered to their antihypertensive medication, and MA among people with HTN improved with an increase in social support (43). Various initiatives and approaches have been implemented to improve MA among older people, including the use of application devices that help older people prevent missed doses and treatment support (44). Multi-dimensional support is essential for people with HTN, with the strongest support coming from partners or children, followed by support from healthcare professionals, friends, and the community (43). Non-adherence to medication has been a major reason behind uncontrolled HTN. The global increase in HTN remains poorly addressed in several populations, including in SEA. Therefore, the emphasis on reducing the risk of HTN is a clear implication of our findings.
Another finding from our review is the negative perception toward medication. Similarly, previous reviews in the SEA region reported the use of herbal medicine as self-treatment due to fear of side effects from prescribed medications (17). Thus, it is important to assess the knowledge of patients and healthcare providers in conveying the side effects of the treatment to be taken.
Various individual, social, and environmental factors influencing MA were identified in all the reviewed studies. As these findings are secondary outcomes of our research, further studies are needed to explore the scope and complexity of factors affecting MA.
Participants in studies on HTN described various unique challenges across all the included studies. Nevertheless, some patterns can be identified; it was found that setting reminders, making individual strategy efforts, increasing self-motivation, discussing with partners, providing healthcare facility support, and utilizing communication media are supportive strategies for improving MA. One study reported improved MA with reminders through phone calls from healthcare providers (45). Awareness of the disease and treatment is likely to make patients more adherent (46).
Another consideration for MA among older people with HTN in the SEA region is difficulty in remembering the medication schedule and lack of family support. Living with family triggers adherence to medication due to support (33), which is in line with our findings. A study reported that strong perceived family support would increase self-esteem and motivation, and motivated patients with HTN would adhere to therapy plans (47). Therefore, the development and evaluation of interventions designed specifically to enhance family support for patient adherence, including training for family members on the importance of medication and how they can assist patients in adhering to treatment, are important.
Another inhibiting factor was the lack of access to healthcare services. People with unemployment face challenges in accessing medication due to the cost of public transportation, as 60% of them cannot afford transportation costs to hospitals (48,49).
Understanding the challenges and patterns that affect MA in older people with HTN allows for planning more effective strategies to improve adherence so patients can manage their condition better and minimize the risk of complications.
Limitations of the Study
One limitation of this review was the inclusion of only studies that were published in English and Indonesian languages. Additionally, there may have been differences in the terms used in each country, which could have led to overlooks by the researchers.
Conclusion
To the best of our knowledge, our review is the first to investigate adherence to medication among older people with HTN in the SEA region. Based on our findings, there was a low rate of adherence to prescribed medication among older people in the reviewed studies. The main reason for non-adherence was a negative perception of the prescribed medication, which was also expressed in several studies. Various strategies were used by individuals to improve their MA. To better understand the individual and situational factors that influence this adherence, further research is necessary. More careful research will support a more personalized approach to addressing these challenges.
Authors’ Contribution
Conceptualization: Andi Fitrah Ramadhanty, Andi Masyitha Irwan
Data curation: Andi Fitrah Ramadhanty, Andi Masyitha Irwan.
Formal analysis: Andi Fitrah Ramadhanty, Andi Masyitha Irwan, Andina Setyawati.
Investigation: Andi Fitrah Ramadhanty, Andi Masyitha Irwan, Andina Setyawati.
Methodology: Andi Fitrah Ramadhanty, Andi Masyitha Irwan.
Project administration: Andi Fitrah Ramadhanty, Andi Masyitha Irwan.
Resources: Andi Fitrah Ramadhanty.
Software: Andi Fitrah Ramadhanty, Andi Masyitha Irwan.
Supervision: Andi Masyitha Irwan, Andina Setyawati.
Validation: Andi Masyitha Irwan, Andina Setyawati.
Visualization: Andi Fitrah Ramadhanty.
Writing–original draft: Andi Fitrah Ramadhanty.
Writing–review & editing: Andi Fitrah Ramadhanty, Andi Masyitha Irwan, Andina Setyawati.
Competing Interests
No author of this paper has any conflict of interests, including specific financial interests, relationships, or affiliations related to the subject matter or materials included in this manuscript.
Ethical Approval
Not applicable.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Supplementary Files
Supplementary files contain Tables S1 and S2.
(pdf)
References
- Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016; 387(10022):957-67. doi: 10.1016/s0140-6736(15)01225-8 [Crossref] [ Google Scholar]
- Zhou B, Danaei G, Stevens GA, Bixby H, Taddei C, Carrillo-Larco RM. Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet 2019; 394(10199):639-51. doi: 10.1016/s0140-6736(19)31145-6 [Crossref] [ Google Scholar]
- Carey RM, Whelton PK. Prevention, detection, evaluation, and management of high blood pressure in adults: synopsis of the 2017 American College of Cardiology/American Heart Association Hypertension Guideline. Ann Intern Med 2018; 168(5):351-8. doi: 10.7326/m17-3203 [Crossref] [ Google Scholar]
- World Health Organization (WHO). Hypertension. 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/hypertension.
- Damasceno A. Noncommunicable disease. In: The Heart of Africa: Clinical Profile of an Evolving Burden of Heart Disease in Africa. John Wiley & Sons; 2016. p. 155-7.
- Aronow WS, Fleg JL, Pepine CJ, Artinian NT, Bakris G, Brown AS. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Coll Cardiol 2011; 57(20):2037-114. doi: 10.1016/j.jacc.2011.01.008 [Crossref] [ Google Scholar]
- Mohammed Nawi A, Mohammad Z, Jetly K, Abd Razak MA, Ramli NS, Wan Ibadullah WAH. The prevalence and risk factors of hypertension among the urban population in Southeast asian countries: a systematic review and meta-analysis. Int J Hypertens 2021; 2021:6657003. doi: 10.1155/2021/6657003 [Crossref] [ Google Scholar]
- Angeli F, Reboldi G, Verdecchia P. The 2014 hypertension guidelines: implications for patients and practitioners in Asia. Heart Asia 2015; 7(2):21-5. doi: 10.1136/heartasia-2015-010639 [Crossref] [ Google Scholar]
- Vrijens B, Urquhart J. Methods for measuring, enhancing, and accounting for medication adherence in clinical trials. Clin Pharmacol Ther 2014; 95(6):617-26. doi: 10.1038/clpt.2014.59 [Crossref] [ Google Scholar]
- Jung O, Gechter JL, Wunder C, Paulke A, Bartel C, Geiger H. Resistant hypertension? Assessment of adherence by toxicological urine analysis. J Hypertens 2013; 31(4):766-74. doi: 10.1097/HJH.0b013e32835e2286 [Crossref] [ Google Scholar]
- Ikeda N, Sapienza D, Guerrero R, Aekplakorn W, Naghavi M, Mokdad AH. Control of hypertension with medication: a comparative analysis of national surveys in 20 countries. Bull World Health Organ 2014; 92(1):10-9C. doi: 10.2471/blt.13.121954 [Crossref] [ Google Scholar]
- Rahmani Pour E, Aliyari S, Farsi Z, Ghelich Y. Comparing the effects of interactive and noninteractive education using short message service on treatment adherence and blood pressure among patients with hypertension. Nurs Midwifery Stud 2020; 9(2):68-76. doi: 10.4103/nms.nms_82_19 [Crossref] [ Google Scholar]
- Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother 2011; 9(1):11-23. doi: 10.1016/j.amjopharm.2011.02.004 [Crossref] [ Google Scholar]
- Kubica A, Gruchała M, Jaguszewski M, Jankowski P, Świeczkowski D, Merks P. Adherence to treatment—a pivotal issue in long-term treatment of patients with cardiovascular diseases An expert standpoint. Med Res J 2018; 2(4):123-7. [ Google Scholar]
- Saleh A, Wirda W, Irwan AM, Latif AI. The relationships among self-efficacy, health literacy, self-care and glycemic control in older people with type 2 diabetes mellitus. Work Older People 2021; 25(2):164-9. doi: 10.1108/wwop-08-2020-0044 [Crossref] [ Google Scholar]
- Anwar N, Irwan AM, Saleh A, Usman S. Effect of foot massage on decreasing blood pressure and anxiety in older people with hypertension in Indonesia. J Health Manag 2022; 24(2):260-7. doi: 10.1177/09720634221087786 [Crossref] [ Google Scholar]
- Irwan AM, Potempa K, Abikusno N, Syahrul S. Self-care management for hypertension in Southeast Asia: a scoping review. J Multidiscip Healthc 2022; 15:2015-32. doi: 10.2147/jmdh.s367638 [Crossref] [ Google Scholar]
- Pinho S, Cruz M, Ferreira F, Ramalho A, Sampaio R. Improving medication adherence in hypertensive patients: a scoping review. Prev Med 2021; 146:106467. doi: 10.1016/j.ypmed.2021.106467 [Crossref] [ Google Scholar]
- Lockwood C, dos Santos KB, Pap R. Practical guidance for knowledge synthesis: scoping review methods. Asian Nurs Res 2019; 13(5):287-94. doi: 10.1016/j.anr.2019.11.002 [Crossref] [ Google Scholar]
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005; 8(1):19-32. doi: 10.1080/1364557032000119616 [Crossref] [ Google Scholar]
- Peters MD, Godfrey CM, McInerney P, Soares CB, Khalil H, Parker D. The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI Scoping Reviews. The Joanna Briggs Institute; 2015.
- World Health Organization (WHO). World Hypertension Day: “Measure Your Blood Pressure, Control it, Live Longer” [Internet]. Dr Poonam Khetrapal Singh, WHO Regional Director for South-East Asia; 2022. Available from: https://www.who.int/southeastasia/news/detail/17-05-2022-world-hypertension-day---measure-your-blood-pressure--control-it--live-longer.
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev 2016; 5(1):210. doi: 10.1186/s13643-016-0384-4 [Crossref] [ Google Scholar]
- Budiarti Y, Harokan A, Suryani L. Analisis Kepatuhan Minum Obat Pada Pasien Lansia Hipertensi Di Puskesmas Tanjung Sakti Pumi Tahun 2023. Jurnal Kesehatan Saelmakers PERDANA (JKSP) 2023; 6(2):399-408. doi: 10.32524/jksp.v6i2.1007 [Crossref] [ Google Scholar]
- Winarti W, Harokan A, Gustina E. Analisis Kepatuhan Pasien Hipertensi Dalam Pengobatan Di Puskesmas. Cendekia Medika: Jurnal Stikes Al-Maarif Baturaja 2023; 8(2):342-55. doi: 10.52235/cendekiamedika.v8i2.246 [Crossref] [ Google Scholar]
- Dolo LS, Yusuf A, Azis R. Analisis Faktor Memengaruhi Kepatuhan Berobat Lansia Penderita Hipertensi Pada Masa Pandemi COVID-19 Di Puskesmas Bulili Kota Palu. PREPOTIF: Jurnal Kesehatan Masyarakat 2021; 5(2):828-42. [ Google Scholar]
- Rahmawati R, Bajorek B. Factors affecting self-reported medication adherence and hypertension knowledge: A cross-sectional study in rural villages, Yogyakarta province, Indonesia. Chronic Illn 2018; 14(3):212-27. doi: 10.1177/1742395317739092 [Crossref] [ Google Scholar]
- Siregar HD, Marlindawani J, Harefa K, Ketaren O, Rohana T. Faktor-Faktor Yang Berhubungan Dengan Hipertensi Di Puskesmas Teladan Kota Medan Tahun 2021. J Healthc Technol Med. 20227(2):985-1001.
- Isbiyantoro I, Budiati E, Antoro B, Karyus A, Irianto SE. Faktor-faktor yang Berhubungan dengan Kepatuhan Minum Obat Pasien Hipertensi. Jurnal Ilmiah Permas: Jurnal Ilmiah STIKES Kendal 2023; 13(4):1565-76. [ Google Scholar]
- Hapsari DI, Kartiana U. Faktor-Faktor Yang Berhubungan Dengan Kepatuhan Pengobatan Penderita Hipertensi Pada Lansia di Wilayah Kerja Puskesmas Sepauk Tahun 2021. Jumantik 2023; 9(2):151-64. [ Google Scholar]
- Lestari P, Suastika L, Widyadharma I. Relationship between medication adherence and hypertension status in public health center. Int J Med Rev Case Rep 2019;1.
- Rahmawati R, Bajorek B. Understanding untreated hypertension from patients’ point of view: a qualitative study in rural Yogyakarta province, Indonesia. Chronic Illn 2018; 14(3):228-40. doi: 10.1177/1742395317718034 [Crossref] [ Google Scholar]
- Berek PA, Afiyanti Y. Compliance of hypertension patients in doing self-care: a grounded theory study. Jurnal Sahabat Keperawatan 2020; 2(1):21-35. [ Google Scholar]
- Wannasirikul P, Termsirikulchai L, Sujirarat D, Benjakul S, Tanasugarn C. Health literacy, medication adherence, and blood pressure level among hypertensive older adults treated at primary health care centers. Southeast Asian J Trop Med Public Health 2016; 47(1):109-20. [ Google Scholar]
- Charoensab N, Pinyopornpanish K, Thangsuk P, Jiraporncharoen W, Angkurawaranon C. Lowered blood pressure targets identify new, uncontrolled hypertensive cases: patient characteristics and implications for services in Thailand. BMC Health Serv Res 2020; 20(1):869. doi: 10.1186/s12913-020-05719-z [Crossref] [ Google Scholar]
- Woodham NS, Taneepanichskul S, Somrongthong R, Auamkul N. Self-care management among elderly patients with hypertension and poor adherence to treatment, living in rural Thailand: a qualitative study. Pak J Public Health 2018; 8(2):84-9. doi: 10.32413/pjph.v8i2.131 [Crossref] [ Google Scholar]
- Haung Z, Hong SA, Tejativaddhana P, Puckpinyo A, Myint M. Multiple self-care behaviors and associated factors in community-dwelling patients with hypertension in Myanmar. Nagoya J Med Sci 2020; 82(2):363-76. doi: 10.18999/nagjms.82.2.363 [Crossref] [ Google Scholar]
- Han WP, Hong SA, Tiraphat S. Factors related to medication adherence among essential hypertensive patients in tertiary hospitals in Yangon, Myanmar. J Public Health Dev 2015; 13(2):57-70. [ Google Scholar]
- Tan CS, Hassali MA, Neoh CF, Saleem F. A qualitative exploration of hypertensive patients’ perception towards quality use of medication and hypertension management at the community level. Pharm Pract (Granada) 2017; 15(4):1074. doi: 10.18549/PharmPract.2017.04.1074 [Crossref] [ Google Scholar]
- Ramli A, Ahmad NS, Paraidathathu T. Medication adherence among hypertensive patients of primary health clinics in Malaysia. Patient Prefer Adherence 2012; 6:613-22. doi: 10.2147/ppa.s34704 [Crossref] [ Google Scholar]
- Mahmood S, Jalal Z, Hadi MA, Khan TM, Haque MS, Shah KU. Prevalence of non-adherence to antihypertensive medication in Asia: a systematic review and meta-analysis. Int J Clin Pharm 2021; 43(3):486-501. doi: 10.1007/s11096-021-01236-z [Crossref] [ Google Scholar]
- Gavrilova A, Bandere D, Rutkovska I, Šmits D, Mauriņa B, Poplavska E. Knowledge about disease, medication therapy, and related medication adherence levels among patients with hypertension. Medicina (Kaunas) 2019; 55(11):715. doi: 10.3390/medicina55110715 [Crossref] [ Google Scholar]
- Pan J, Hu B, Wu L, Li Y. The effect of social support on treatment adherence in hypertension in China. Patient Prefer Adherence 2021; 15:1953-61. doi: 10.2147/ppa.s325793 [Crossref] [ Google Scholar]
- Suzuki R, Hasegawa T. Evaluation of a one-dose package medication support system for community-based elderly patients and eldercare facilities. Am J Health Syst Pharm 2018; 75(9):e202-12. doi: 10.2146/ajhp170176 [Crossref] [ Google Scholar]
- Holt EW, Rung AL, Leon KA, Firestein C, Krousel-Wood MA. Medication adherence in older adults: a qualitative study. Educ Gerontol 2014; 40(3):198-211. doi: 10.1080/03601277.2013.802186 [Crossref] [ Google Scholar]
- Mutneja E, Yadav R, Dey AB, Gupta P. Frequency and predictors of compliance among patients taking antihypertensive medicines. Indian Heart J 2020; 72(2):136-9. doi: 10.1016/j.ihj.2020.03.008 [Crossref] [ Google Scholar]
- Ojo OS, Malomo SO, Sogunle PT. Blood pressure (BP) control and perceived family support in patients with essential hypertension seen at a primary care clinic in Western Nigeria. J Family Med Prim Care 2016; 5(3):569-75. doi: 10.4103/2249-4863.197284 [Crossref] [ Google Scholar]
- Wariva E, January J, Maradzika J. Medication adherence among elderly patients with high blood pressure in Gweru, Zimbabwe. J Public Health Afr 2014; 5(1):304. doi: 10.4081/jphia.2014.304 [Crossref] [ Google Scholar]
- Irwan AM, Kato M, Kitaoka K, Kido T, Taniguchi Y, Shogenji M. Self-care practices and health-seeking behavior among older persons in a developing country: theories-based research. Int J Nurs Sci 2016; 3(1):11-23. doi: 10.1016/j.ijnss.2016.02.010 [Crossref] [ Google Scholar]