J Educ Community Health. 9(4):235-240.
doi: 10.34172/jech.2022.1829
Original Article
COVID-19 Preventive Behaviors and Related Beliefs Among Diabetics: The Use of Protection Motivation Theory
Mohadese Sadri 1  , Majid Barati 2, 3
, Majid Barati 2, 3  , Shiva Borzouei 4, *
, Shiva Borzouei 4, *  , Saeed Bashirian 5, Salman Khazaei 6, Ensiyeh Jenabi 2
, Saeed Bashirian 5, Salman Khazaei 6, Ensiyeh Jenabi 2  , Sepideh Zareian 7
, Sepideh Zareian 7
Author information:
1Department of Public Health, School of Health, Hamadan University of Medical Sciences, Hamadan, Iran
2Autism Spectrum Disorders Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
3Department of Public Health, Asadabad School of Medical Sciences, Asadabad, Iran
4Clinical Research Development Unit of Shahid Beheshti Hospital, Hamadan University of Medical Science, Hamadan, Iran
5Social Determinants of Health Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
6Research Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran
7Head of Statistics and Information Technology Management Infrastructure Department, Hamadan University of Medical Sciences, Hamadan, Iran
Abstract
Background: Recent data from coronavirus disease 2019 (COVID-19) confirm that diabetes, along with advanced age, is an important risk factor for adverse prognosis. Therefore, the present study aimed to determine the status of COVID-19 prevention behaviors and related beliefs among diabetic patients in Hamadan province using protection motivation theory (PMT).
Methods: This cross-sectional descriptive study was conducted from April to September 2020. The research population included all diabetics, of whom 355 patients, who referred to an adult endocrinologist in Hamadan, were selected using the convenience sampling method. The data collection tool was a researcher-made questionnaire with demographic variables and PMT constructs. Data were analyzed by SPSS 22 using descriptive statistics, correlation, and logistic regression.
Results: According to the result, the PMT construct explained 15% of the variance in the frequency of the intention to perform preventive behaviors. Perceived sensitivity (β=-0.128), perceived response efficiency (β=0.140), and perceived response cost (β=0.386) were the best significant predictors of behavior (P<0.05). There was a significant relationship between gender (P<0.001), marital status (P<0.001), and level of education (P=0.040) in observing preventive behaviors.
Conclusion: It is necessary to enhance the levels of awareness and self-efficacy of diabetic patients to reduce fear in this at-risk group. Further, it is appropriate to use PMT to promote preventive behaviors.
Keywords: Diabetes, Preventive behaviors, Beliefs, Cognitive-social theories, Coronavirus
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Sadri M, Barati M, Borzouei S, Bashirian S, Khazaei S, Jenabi E, et al. Covid-19 preventive behaviors and related beliefs among diabetics: the use of protection motivation theory. J Educ Community Health. 2022; 9(4):235-240. doi:10.34172/ jech.2022.1829
Introduction
In the new millennium, people are exposed to serious health challenges such as the growing trend of non-communicable diseases, including cardiovascular diseases, cancers, and diabetes (1). The World Health Organization (WHO) states that there is a clear epidemic of diabetes strongly related to changes in the patient’s lifestyle and economic status (2). According to WHO reports, the number of people with diabetes will increase from 200 million in 2000 to 592 million in 2035, with the highest prevalence in developing countries such as the Middle East nations. Among the Middle East countries, Iran has the third rank with 4.5 million diabetic people (3). The WHO indicates that diabetes kills 3.2 million people annually and predicts that this number will be doubled by 2030 (4). Over the past two decades, the prevalence of acute respiratory infections has turned into one of the most serious global health risks and challenges (5). The recent coronavirus, which was detected in China in late 2019, is a new coronavirus called coronavirus disease 2019 (COVID-2019) from the coronavirus family and the beta-coronavirus genus (6). The disease is currently prevalent in most countries of the world such that it has affected more than 60 million people and killed more than one million people worldwide. The disease spread so fast in Iran similar to other countries. According to the Ministry of Health and Medical Education of Iran, on November 30 of 2020, 948 749 definite cases of COVID-19 infection and 47 874 deaths were registered in the country (7). As diabetes is a chronic disease adversely affecting all body systems, people with diabetes are at greater risk for complications when infected with the virus (8). In one of the most recent studies on 50 466 patients with coronavirus, the death rate from the virus was reported to be 4.3. Nonetheless, most of those who died had previous underlying diseases such as hypertension, diabetes, and cardiovascular diseases (9). Recent data from COVID-19 confirm that diabetes, along with advanced age, is an essential risk factor for adverse prognosis. According to a preliminary analysis by a small group in Wuhan, approximately 20% of those admitted to intensive care units were diabetic. In addition, new Italian data show that more than two-thirds of people with acute respiratory syndrome died of diabetes (10,11). Thus, it is necessary to pay attention to preventive measures by diabetic patients during the epidemic caused by this virus. Determinants and factors affecting preventive behaviors must be identified for this purpose (12). The patterns and theories of behavior change are used in this respect. Fear appeal theories are among the best known of these theories used to examine barriers to proper health behaviors and behavior descriptions (13,14). Protection motivation theory (PMT) is one of the cognitive-social theories used to study factors affecting motivation, and ultimately, the protective behavior of the individual. This theory, which was developed by Rogers, has been employed as a general framework for predicting health behaviors and health-related interventions (15). Based on the assumptions of this theory, threat and confrontation evaluations are two parallel cognitive processes that lead to protection motivation. According to this theory, individuals must first feel threatened about the disease (perceived sensitivity). Then, they should perceive the depth of the risk and the severity of its various complications (perceived severity) and understand the consequence of not performing protective behaviors at the least possible level (reward for an inconsistent response). Moreover, they must believe in the usefulness and applicability of the prevention program (response effectiveness) and find the factors preventing action less costly than its benefits (response costs). In this way, they can understand the ability to perform protective behaviors (perceived self-efficacy) to take preventive actions (15,16). Diabetes is recognized as one of the most important risk factors for increasing COVID-19 mortality (17), and PMT plays a role in the analysis of beliefs associated with performing protective behaviors in diabetic patients. Therefore, the present study sought to determine the status of the preventive behaviors of diabetic patients in Hamadan Province using PMT during the COVID-19 outbreak.
Materials and Methods
This cross-sectional study was performed from April to September 2020 in Omid Clinic in Hamadan. The research population consisted of all diabetics, of whom 355 cases referring to an adult endocrinologist were selected as the sample using the convenient sampling method among the patients with the inclusion criteria. The inclusion criteria were being a patient with at least a 6-month history of diabetes, having the least literacy level, being over 20 years of age, and showing a willingness to participate in the study. The exclusion criterion, on the other hand, was the dissatisfaction of patients with participation in the study. First, patients were given the necessary information about the objectives of the study and the confidentiality of the information, then they filled out the questionnaire.
A researcher-made questionnaire was used to collect the data. The first part had 9 questions about demographic characteristics, including age, gender, level of education, and marital status, as well as information about the person’s illness such as duration of diabetes, height and weight of the patient, fasting blood sugar level, and quarterly blood sugar level. Questions related to PMT were designed using a sample of a questionnaire used in a similar study (18). This section included the construct of perceived sensitivity with 2 questions (e.g., I am unlikely to develop COVID-19), perceived severity with 3 questions (e.g., COVID-19 can lead to death), perceived response effectiveness with 5 questions (e.g., frequently washing hands with soap and water prevents COVID-19). In addition, the other constructs were perceived self-efficacy with 5 questions (e.g., I can stop shaking hands with others) and the cost of the perceived answer with 2 questions (e.g., I feel it is difficult to protect myself against COVID-19). Protection motivation with 1 question (“I intend to adhere to the recommended precaution until the end of the COVID-19 pandemic”) was measured based on a 5-point Likert-type scale from strongly agree (5) to strongly disagree (1). Preventive behavior against COVID-19 was evaluated with 5 questions (e.g., using a mask) on a three-point scale of never (0), sometimes (1), and always (2). In this study, the threat evaluation score was estimated by summing the perceived sensitivity and severity scores. Further, the coping evaluation score was determined by summing the perceived response self-efficacy and efficiency scores minus the perceived response cost. Then, the total scores of the threat evaluation and response were divided by the number of questions in each section to weigh and standardize. Eventually, the coping score was subtracted from the threat score. If the obtained value was a positive number (zero or higher), it showed the person’s involvement in the risk perception process. Furthermore, if the number was negative (less than zero), it was the person’s involvement in the fear perception process (19).
The content validity of the questionnaire was evaluated by a panel of experts using the opinions of 10 health education and health promotion experts, internal medicine, and endocrinologists. The final form of the questions of each section was determined by applying the desired changes. The reliability of the questionnaire was investigated in a pilot study on 30 diabetic patients. The internal correlation coefficient (Cronbach’s alpha) of the constructs was estimated at 0.704.
The collected data were entered into SPSS software (version 22) and analyzed using descriptive statistics, Pearson’s correlation test, and logistic regression.
Results
The mean age of the study participants was 57.94 ± 10.03 with a range of 33-89 years, and most people were in the age group of 50-60 years. Most subjects were females (57.5%) and had a diploma (34.1%). Moreover, 36.1% of patients reported their duration of illness between 5 and 10 years. More than half of the participants were overweight. In terms of fasting blood sugar, 60.8% of patients had blood sugar higher than 130 mg/dL. In the quarterly blood sugar test, the results showed that 60.8% of patients had A1C > 7.5 (Table 1). As regards COVID-19 information sources, over 80% of the participants used radio and television to obtain information. Additionally, more than 60% of people considered radio and television as the most reliable source of information in this case. Studies on the frequency of access to personal protective equipment demonstrated that more than 95% of people had access to masks as the most important means of personal protection.
Table 1.
Distribution of Absolute and Relative Frequency of Demographic Information of the Subjects (N = 355)
|
Variables
|
Frequency
|
Percent
|
| Gender |
Female |
204 |
57.5 |
| Male |
151 |
42.5 |
| Age groups |
Less than 50 years |
86 |
24.2 |
| 51-60 years |
131 |
36.9 |
| 61-70 years |
100 |
28.2 |
| 71 years and older |
38 |
10.7 |
| Educational level |
Illiterate |
121 |
34.1 |
| High school |
68 |
19.2 |
| Diploma |
121 |
34.1 |
| University |
45 |
12.7 |
| Marital status |
Married |
351 |
98.9 |
| Single |
4 |
1.1 |
| Duration of infection |
1-5 years |
119 |
33.5 |
| 5-10 years |
128 |
36.1 |
| Over 11 years |
108 |
30.4 |
| Body mass index |
Less than 24.9 |
84 |
23.7 |
| 25-29.9 |
197 |
55.5 |
| More than 30 |
74 |
20.8 |
| Blood sugar of the current month |
Less than 130 |
181 |
39.2 |
| More than 130 |
216 |
60.8 |
| Quarterly blood sugar (A1c) |
Less than 7.5 |
181 |
39.2 |
| More than 7.5 |
216 |
60.8 |
Concerning the studied preventive behaviors, the results revealed that most participants always washed their hands frequently with soap and water and observed social distance, and used gloves less than others (Figure 1).
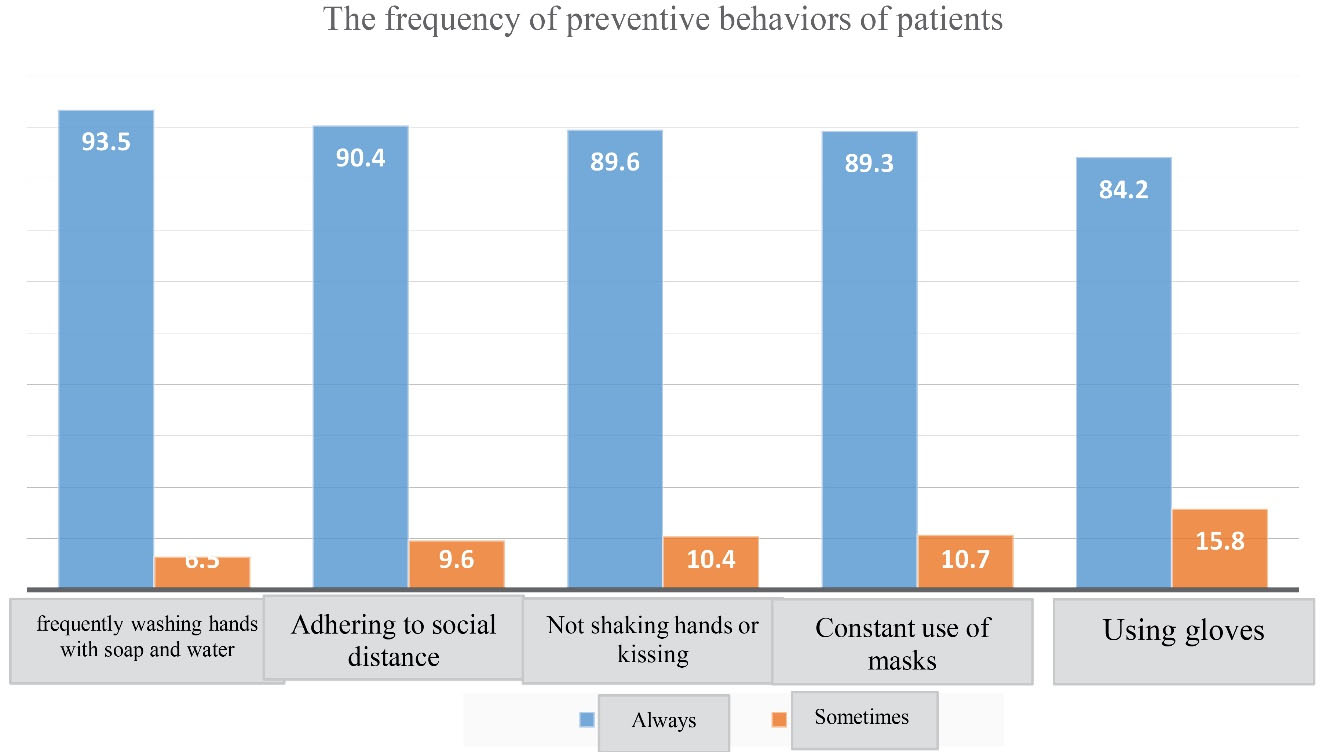
Figure 1.
Distribution of relative frequency of preventive behaviors of the subjects
.
Distribution of relative frequency of preventive behaviors of the subjects
The results of examining the relationship between demographic variables and preventive behavior of study participants indicated a significant difference in the mean score of preventive behavior with gender (0.001), marital status (0.001), and education (0.040). In other words, women, married people, and people with diplomas had stronger preventive behavior (Table 2).
Table 2.
Studying the Relationship Between Demographic Variables and Preventive Behavior of the Subjects
|
Variables
|
Mean
|
SD
|
P
Value
|
| Gender |
Female |
9.69 |
1.00 |
< 0.001 |
| Male |
9.09 |
1.75 |
| Age |
< 50 years |
9.35 |
1.58 |
0.753 |
| 51-60 years |
9.53 |
1.16 |
| 61-70 years |
9.40 |
1.42 |
| 71 years and older |
9.34 |
1.66 |
| Marital status |
University |
9.46 |
1.37 |
< 0.001 |
| Married |
7.00 |
2.00 |
| Duration of illness |
Single |
9.55 |
1.27 |
0.119 |
| 1-5 years |
9.23 |
1.68 |
| 5-10 years |
9.54 |
1.13 |
| Education |
Illiterate |
9.46 |
1.50 |
0.040 |
| High school |
9.40 |
1.40 |
| Diploma |
9.61 |
1.23 |
| University |
9.91 |
1.45 |
| BMI |
< 18.5 |
9.50 |
0.70 |
0.058 |
| 18.6-24.9 |
9.06 |
1.78 |
| 25-29.9 |
9.55 |
1.28 |
| More than 30 |
9.51 |
1.17 |
Note. SD: Standard deviation; BMI: Body mass index.
Based on the results, the constructs of the PMT in Table 3, perceived response efficiency, perceived self-efficacy, perceived intensity, and perceived sensitivity were in relatively good conditions. Moreover, there was a positive and significant correlation between protection motivation and perceived response efficiency, perceived self-efficacy, and perceived response cost. In addition, a direct and significant relationship was found between preventive behavior and perceived sensitivity, perceived severity, perceived response efficiency, and perceived self-efficacy. Of the 355 diabetic patients, 335 (94.4%) cases were in the process of understanding fear.
Table 3.
The Statistical Mean of Scores, Achievable Score Range, and Matrix of Pearson Correlation Coefficients Between the Studied Variables Among the Subjects
|
Variables
|
Mean±SD
|
The Average Percentage of the Maximum Achievable Score
|
1
|
2
|
3
|
4
|
5
|
6
|
| 1. Perceived sensitivity |
7.65 ± 1.41 |
70.62 |
1 |
|
|
|
|
|
| 2. Perceived intensity |
12.14 ± 1.57 |
76.16 |
0.261** |
1 |
|
|
|
|
| 3. Perceived response efficiency |
21.13 ± 2.53 |
80.65 |
0.081 |
0.006 |
1 |
|
|
|
| 4. Perceived self-efficacy |
20.02 ± 2.81 |
75.01 |
0.021 |
0.062 |
-0.281** |
1 |
|
|
| 5. Perceived response cost |
7.21 ± 2.36 |
65 |
-0.189** |
-0.172* |
-0.064 |
-0.281** |
1 |
|
| 6. Protective motivation |
4.25 ± 1.04 |
81.25 |
-0.044 |
0.056 |
0.105 |
0.159** |
0.353** |
1 |
Note. SD: Standard deviation. *Correlation is significant at 0.05, **Correlation is significant at 0.01.
The results of linear regression (Table 4) represented that various constructs of PMT explain 15% of the variance of intention to perform preventive behavior in the studied patients. Based on the findings, perceived sensitivity (P < 0.011), perceived response efficiency (P < 0.005), and perceived response cost (P < 0.0001) had a significant contribution to explaining the variance of intention to perform preventive behavior by the examined individuals.
Table 4.
The Results of the Linear Regression of PMT Constructs in Predicting the Intention of the Preventive Behavior of Subjects
|
Variable
|
Regression Coefficient
|
Standard Error
|
Line Slope (β)
|
P
Value
|
CI
|
Coefficient of Explanation* (R2)
|
|
High Bound
|
Low Bound
|
| Perceived sensitivity |
-0.094 |
0.037 |
-0.128 |
0.011 |
-0.166 |
-0.021 |
0.156 |
| Perceived response efficiency |
0.057 |
0.020 |
0.140 |
0.005 |
0.097 |
0.018 |
| Perceived response cost |
0.170 |
0.022 |
0.386 |
0.0001 |
0.217 |
0.126 |
Note. The results are related to the third stage of linear regression by the stepwise method.
Discussion
The present study was conducted to examine the status of preventive behaviors of COVID-19 using PMT among 355 diabetic patients in Hamadan from April to September 2020.
More than 80% of the participants had a favorable status in performing preventive behaviors in the study, which is in line with the results of Andarge et al (20). These researchers measured the intention and personal preventive measures against the prevalence of COVID-19 in adults with chronic illness in southern Ethiopia with the Theory of Planned Behavior. It is of note that, in this study, more than half of the participants followed preventive behaviors. In another study, Zhong et al (21) investigated knowledge, attitudes, and practices toward COVID-19-preventive behaviors among Chinese residents, whose behaviors were reported to be undesirable. Among these behaviors, frequent hand-washing with soap and water was the most common, while using gloves was the least frequent behavior. Further, other studies showed the positive effect of using protective equipment such as masks and gloves in preventing infection (22,23). In the study of the relationship between demographic variables and preventive behaviors among the participants, a significant relationship was identified between gender, marital status, and level of education with preventive behaviors, which conforms to the result reported by Zhong et al (21).
Based on the results, protection motivation, perceived response efficiency, perceived self-efficacy, perceived intensity, and perceived sensitivity were in relatively good conditions. Khazaei et al (24) studied the preventive behaviors of COVID-19 and related beliefs among health workers using a parallel process model developed as one of the theories of fear induction. They concluded that the status of perceived sensitivity, perceived intensity, perceived self-efficacy, and perceived response efficiencies was somehow desirable. In the present study, more than 90% of patients were in the process of fear appeal. This result is in conformity with those of Khazaei et al (24), Amirfakhraei et al (25), and external studies by Roy et al (26) and Rajkumar (27), examining COVID-19 anxiety among various populations.
The results of the linear regression between theoretical constructs and intent to perform preventive behaviors in the present study revealed that these constructs explain 15% of the variance of intent to perform among diabetic patients. Among these constructs, perceived sensitivity, perceived response effectiveness, and perceived response costs had a significant role in explaining the variance of preventive behavior by the subjects. However, in the study of Ezati Rad et al (28), examining COVID-19 preventive behaviors in Hormozgan, 39% of the intention to perform the behavior was predicted. This difference could be due to the influence of the data collection tool. Based on this research, the constructs of reward, perceived response effectiveness, self-efficacy, and fear had a significant contribution to the prediction, which are different from the constructs of the present study. This difference can be because of the effect of various contextual variables in the study. Furthermore, in the study of Grano et al (29) about the predictors of protective behaviors during the Italian COVID-19 pandemic, self-efficacy constructs and perceived severity were the strongest predictors of intention to engage in protective behaviors, followed by intentions and fear arousal predicted protective behaviors.
Among the limitations of the study were the use of a convenient sampling method and the cross-sectional nature of the study. Therefore, it is recommended that longitudinal studies should be designed and implemented in this regard. However, as a strong point of this study, the information used in this study has been collected in a self-report mode.
Conclusion
Adherence to preventive behaviors by diabetic patients was evaluated as desirable, whereas the level of fear of COVID-19 was extremely high in this group. Hence, it is recommended that effective educational theories should be used to formulate educational programs to lower the level of fear in this group. In this respect, educational interventions based on fear-motivating theories can be applied in high-risk groups. Additionally, the same pattern can be employed in future studies on other at-risk groups.
Acknowledgments
The study was approved by the Research Council of Hamadan University of Medical Sciences (Project number: 9904242481) and conducted with the support of the Vice-chancellor for Research and Technology of Hamadan University of Medical Sciences. Hereby, the authors are pleased to appreciate all those participating in the study.
Author Contributions
Conceptualization: Majid Barati, Shiva Borzouei.
Data curation: Sepideh Zareian.
Formal Analysis: Salman Khazaei.
Funding acquisition: Saeed Bashirian, Shiva Borzouei.
Investigation: Majid Barati, Mohadeseh Sadri.
Methodology: Salman Khazaei, Ensiyeh Jenabi.
Project administration: Saeed Bashirian.
Supervision: Majid Barati.
Validation: Mohadeseh Sadri.
Writing – original draft: Mohadeseh Sadri, Majid Barati.
Writing – review & editing: Shiva Borzouei, Saeed Bashirian, Salman Khazaei.
Conflict of Interests
The authors reported no conflict of interests in the study.
Ethical Permissions
The study was approved by the Ethics Committee for the Research Council and the Research of Hamadan University of Medical Sciences with the ethics code of ID IR.UMSHA.REC.1399.231.
Funding/Support
This study was funded by Hamadan University of Medical Sciences, Hamadan, Iran.
References
- Swe EE, Htet KKK, Thekkur P, Aung LL, Aye LL, Myint T. Increasing trends in admissions due to non-communicable diseases over 2012 to 2017: findings from three large cities in Myanmar. Trop Med Health 2020; 48:24. doi: 10.1186/s41182-020-00209-8 [Crossref] [ Google Scholar]
- Abi Khalil C, Al Suwaidi J, Refaat M, Mohammedi K. Cardiac complications of diabetes. Biomed Res Int 2018; 2018:8578394. doi: 10.1155/2018/8578394 [Crossref] [ Google Scholar]
- Marzban A. Relationship between spiritual health and quality of life in type II diabetic patients: a cross-sectional study in Yazd. J Diabetes Nurs 2018;6(4):641-52. [Persian].
- Mousavizadeh SN, Ashktorab T, Ahmadi F, Zandi M. Evaluation of barriers to adherence to therapy in patients with diabetes. J Diabetes Nurs 2016;4(3):94-108. [Persian].
- Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol 2019; 17(3):181-92. doi: 10.1038/s41579-018-0118-9 [Crossref] [ Google Scholar]
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382(8):727-33. doi: 10.1056/NEJMoa2001017 [Crossref] [ Google Scholar]
- Worldometer. COVID-19 Coronavirus Pandemic [Internet]. USA: Worldometer; 2020. Avaliable from: https://www.worldometers.info/coronavirus/. Accessed June 20, 2020.
- Hussain A, Bhowmik B, do Vale Moreira NC. COVID-19 and diabetes: Knowledge in progress. Diabetes Res Clin Pract 2020; 162:108142. doi: 10.1016/j.diabres.2020.108142 [Crossref] [ Google Scholar]
- Sun P, Qie S, Liu Z, Ren J, Xi J. Clinical characteristics of 50466 patients with 2019-nCoV infection. medRxiv [Preprint]. February 25, 2020. Available from: https://www.medrxiv.org/content/10.1101/2020.02.18.20024539v2.
- Song Z, Xu Y, Bao L, Zhang L, Yu P, Qu Y. From SARS to MERS, thrusting coronaviruses into the spotlight. Viruses 2019; 11(1):59. doi: 10.3390/v11010059 [Crossref] [ Google Scholar]
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395(10223):497-506. doi: 10.1016/s0140-6736(20)30183-5 [Crossref] [ Google Scholar]
- Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020; 7(3):228-9. doi: 10.1016/s2215-0366(20)30046-8 [Crossref] [ Google Scholar]
- Fathi Y, Barati M, Zandiyeh M, Bashirian S. Prediction of preventive behaviors of the needlestick injuries during surgery among operating room personnel: application of the health belief model. Int J Occup Environ Med 2017; 8(4):232-40. doi: 10.15171/ijoem.2017.1051 [Crossref] [ Google Scholar]
- Witte K, Allen M. A meta-analysis of fear appeals: implications for effective public health campaigns. Health Educ Behav 2000; 27(5):591-615. doi: 10.1177/109019810002700506 [Crossref] [ Google Scholar]
- Koelen MA, Van den Ban AW. Health Education and Health Promotion. 1thed. Netherlands: Wageningen Academic Publishers; 2004. p. 62-4.
- Rezaeipandari H, Mirkhalili SM, Morowati Sharifabad MA, Ayatollahi J, Fallahzadeh H. Study of H1N1 influenza preventive behaviors predictors based on health belief model in Jiroft people. Qom Univ Med Sci J 2018; 12(3):76-86. doi: 10.29252/qums.12.3.76.[Persian] [Crossref] [ Google Scholar]
- Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020; 323(18):1775-6. doi: 10.1001/jama.2020.4683 [Crossref] [ Google Scholar]
- Bashirian S, Jenabi E, Khazaei S, Barati M, Karimi-Shahanjarini A, Zareian S. Factors associated with preventive behaviours of COVID-19 among hospital staff in Iran in 2020: an application of the Protection Motivation Theory. J Hosp Infect 2020; 105(3):430-3. doi: 10.1016/j.jhin.2020.04.035 [Crossref] [ Google Scholar]
- Milne S, Sheeran P, Orbell S. Prediction and intervention in health-related behavior: a meta-analytic review of protection motivation theory. J Appl Soc Psychol 2000; 30(1):106-43. doi: 10.1111/j.1559-1816.2000.tb02308.x [Crossref] [ Google Scholar]
- Andarge E, Fikadu T, Temesgen R, Shegaze M, Feleke T, Haile F. Intention and practice on personal preventive measures against the COVID-19 pandemic among adults with chronic conditions in Southern Ethiopia: a survey using the theory of planned behavior. J Multidiscip Healthc 2020; 13:1863-77. doi: 10.2147/jmdh.s284707 [Crossref] [ Google Scholar]
- Zhong BL, Luo W, Li HM, Zhang QQ, Liu XG, Li WT. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci 2020; 16(10):1745-52. doi: 10.7150/ijbs.45221 [Crossref] [ Google Scholar]
- Huh S. How to train health personnel to protect themselves from SARS-CoV-2 (novel coronavirus) infection when caring for a patient or suspected case. J Educ Eval Health Prof 2020; 17:10. doi: 10.3352/jeehp.2020.17.10 [Crossref] [ Google Scholar]
- Cheng VC, Wong SC, Chuang VW, So SY, Chen JH, Sridhar S. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J Infect 2020; 81(1):107-14. doi: 10.1016/j.jinf.2020.04.024 [Crossref] [ Google Scholar]
- Khazaei S, Bashirian S, Jenabi E, Barati M, Karimi-Shahanjarini A, Moeini B. COVID-19 preventive behaviors and its related beliefs among health workers: the role of threat and coping appraisals. J Educ Community Health 2020; 7(3):221-7. doi: 10.29252/jech.7.3.221.[Persian] [Crossref] [ Google Scholar]
- Amirfakhraei A, Masoumifard M, Esmaeilishad B, Dashtbozorgi Z, Darvish Baseri L. Prediction of corona virus anxiety based on health concern, psychological hardiness, and positive meta-emotion in diabetic patients. J Diabetes Nurs 2020; 8(2):1072-83. [ Google Scholar]
- Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr 2020; 51:102083. doi: 10.1016/j.ajp.2020.102083 [Crossref] [ Google Scholar]
- Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr 2020; 52:102066. doi: 10.1016/j.ajp.2020.102066 [Crossref] [ Google Scholar]
- Ezati Rad R, Mohseni S, Kamalzadeh Takhti H, Hassani Azad M, Shahabi N, Aghamolaei T. Application of the protection motivation theory for predicting COVID-19 preventive behaviors in Hormozgan, Iran: a cross-sectional study. BMC Public Health 2021; 21(1):466. doi: 10.1186/s12889-021-10500-w [Crossref] [ Google Scholar]
- Grano C, Singh Solorzano C, Di Pucchio A. Predictors of protective behaviours during the Italian COVID-19 pandemic: an application of protection motivation theory. Psychol Health. 2022:1-21. 10.1080/08870446.2022.2062355.