J Educ Community Health. 10(4):242-249.
doi: 10.34172/jech.2505
Review Article
Challenges and Opportunities for Diabetes Care in Indigenous People: A Scoping Review
Yusran Haskas 1, *  , Suarnianti Suarnianti 1
, Suarnianti Suarnianti 1  , Indah Restika 1
, Indah Restika 1 
Author information:
1Nursing Science Department, Nani Hasanuddin Health Institute, Makassar, Indonesia
Abstract
Background: Diabetes mellitus in indigenous people has increased globally. This disease develops very quickly and has a higher prevalence among indigenous people. When caring for diabetes, indigenous people face many obstacles that worsen their condition. However, only a few studies have comprehensively reviewed such a condition and investigated various tribal backgrounds of indigenous people. This study aimed to identify diverse challenges and opportunities in caring for diabetes in indigenous people.
Methods: This scoping review was conducted from March to August 2022 by searching for manuscripts on PubMed, Science Direct, Cochrane Library, Wiley, Directory of Open Access Journals, ProQuest, GARUDA, and Grey Literature databases to identify challenges and opportunities in caring for diabetes mellitus in indigenous people. Three reviewers independently screened the results, and the extracted data were then mapped, categorized, and summarized.
Results: This study identified eight categories of challenges and three opportunities. Trust, language, health literacy, access to health services, and costs are challenges for indigenous people in caring for diabetes. In addition, three aspects were considered opportunities to care for diabetes in indigenous people: support from health workers who are from the indigenous communities to solve trust issues, intervention modification based on culture, language, and technology, and support from health authorities.
Conclusion: Challenges to the indigenous people’s religious and cultural factors should be addressed seriously to care for diabetes. However, this action requires different approaches and cannot be generalized to all indigenous communities.
Keywords: Diabetes care barriers, Diabetes care opportunities, Diabetes care, Indigenous people, Diabetes mellitus
Copyright and License Information
© 2023 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Haskas Y, Suarnianti S, Restika I. Challenges and opportunities for diabetes care in indigenous people: a scoping review. J Educ Community Health. 2023; 10(4):242-249. doi:10.34172/jech.2505
Introduction
Diabetes has reached epidemic proportions in indigenous populations worldwide (1). The disease develops very quickly, and a higher prevalence is found in the indigenous population than in the general population (2). In addition, indigenous people who have diabetes will more frequently experience complications than other groups (3), and this complication rate will increase dramatically over the next decade (4). Indigenous people with diabetes mellitus frequently experience complications such as diabetic macular edema, proliferative diabetic retinopathy, cardiovascular diseases, kidney disease, and death (5). Such conditions occur because they encounter many barriers in receiving health care, and these barriers worsen their diabetes management (6). Moreover, this condition certainly and substantially reduces their disability-free life expectancy (7).
Diabetes in indigenous people is caused by several factors: the historical context of colonial policies, the people’s adverse experiences in their remote places, the long-term metabolic effects of hunger and stress (8), the experience of food restrictions that may encourage subsequently inadequate nutritional behavior (9), food insecurity in remote areas where indigenous communities live (10), and environmental degradation of traditional food sources such as fish and seafood (11). In recent years, cultural safety has been proposed as a transformative approach to health care that possibly increases the need for considerations, expectations, rights, and identities of indigenous patients (12). However, the current knowledge about cultural safety in caring for diabetes does not allow the development of a local understanding of diabetes issues or support the information on clinical practices (13).
In addition, no reviews focused on diabetes care, opportunities, and challenges for indigenous people. The previous review generally discussed diabetes in indigenous people, including their burden of diabetes, complications, and diabetes management (14). This study is the first review that considers the complexity of diabetes problems, the challenges of diabetes care, and the low commitment to handling national health problems for indigenous people. This study is interesting and can handle diabetes care problems in indigenous people. Therefore, this study aimed to identify scientific evidence on the challenges and opportunities of diabetes care in indigenous people with diabetes mellitus.
Materials and Methods
Research Design
This scoping review scrutinized the challenges and opportunities to care for diabetes mellitus in indigenous people. Moreover, this review referred to the Joanna Briggs Institute (15) and scoping review methodology(16).
Study Protocol
The reporting of this scoping review was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Extension for Scoping Reviews (PRISMA-ScR) (http://www.prisma-statement.org/documents/PRISMA-ScR-Fillable-Checklist_11Sept2019.pdf) (17).
Search Strategies
This study used several keywords for the literature search such as diabetes mellitus, indigenous people, diabetes care, and barriers in diabetes care. The extensive search was conducted on PubMed, Science Direct, Cochrane Library, Wiley, Directory of Open Access Journals, ProQuest, GARUDA, and Google Scholar. A recent search of the confirmed database (ISI database) resulted in no additional studies for consideration. After identifying diabetes care, more specific search terms were performed to find barriers to diabetes mellitus care. This review limited studies published in peer-reviewed journals from 2012 to 2022 and written in English. The keywords were adopted from Medical Subject Heading (MeSH) terms, and Boolean operators used in the search were as follows: “diabetes mellitus” OR “diabetes mellitus, type 2” OR “diabetes mellitus, type 1” AND “indigenous peoples” OR “diabetes care” OR “diabetes management” OR “diabetes treatment” OR “challenge” OR “opportunity”. Full search strategies are presented in Supplementary file 1.
Study Selection and Eligibility Criteria
This review involved three reviewers to minimize bias. The selected studies were reviewed in two stages. First, the authors reviewed the title and abstract, and second, the full-text articles were reviewed. The selection process was conducted through gradual inclusion and exclusion criteria, as presented in scheme 1 using the PRISMA. Afterward, 544 potential articles were identified. This review excluded manuscripts not written in English, not following the research questions, duplicated, not provided in full text, not discussing diabetes care, and not following the research results. Thus, this study only involved 19 articles that met the inclusion criteria (Figure 1). The inclusion criteria encompassed the PCC: the population (indigenous people with diabetes mellitus), concept(diabetes care), and context (challenges and opportunities in diabetes care).
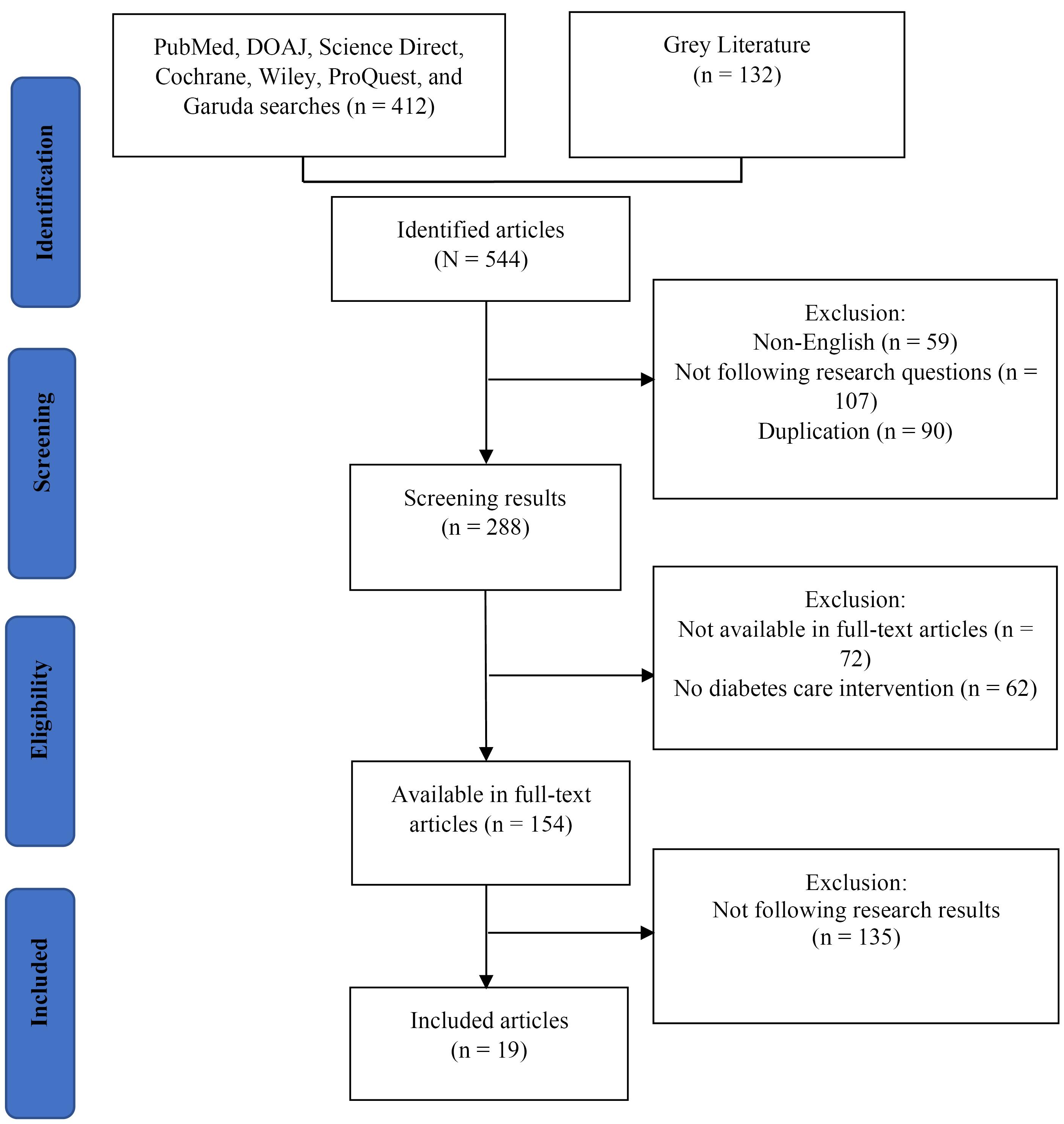
Figure 1.
Flowchart for Inclusion and Exclusion Studies
.
Flowchart for Inclusion and Exclusion Studies
Data Extraction
The data were extracted from full-text journal articles that met the inclusion criteria. The current review employed the data extraction form developed by the Joanna Briggs Institute (18). The analytical framework was developed to document the selected studies and research characteristics in an Excel spreadsheet. These characteristics included researchers, years, research sites, titles, designs, research objectives, samples, and results. The review results were reported in a narrative form to identify themes of barriers and opportunities in caring for indigenous people with diabetes.
Data Analysis and Synthesis
We compiled descriptive statistics (frequencies and percentages) in methodological tables and narrative synthesis of all the included studies (19 articles). Data relevant to the objectives and questions of this scoping review were evaluated. Each reviewer synthesized a comprehensive description of identified themes that answered the objectives and questions of this scope. They included “What are the challenges of diabetes care in indigenous people?” and “What are the opportunities of diabetes care in indigenous people?” A narrative synthesis is a systematic and transparent analysis approach that a review employs to analyze and summarize text and explain the findings (19).
Results
General Characteristics
This study imported 544 articles for screening, and only 19 articles fit the inclusion criteria. The reviewed articles are summarized in Schematic 1. Most of the studies were conducted in the Australian outback with five aboriginal tribes (12,20-23), one Victorian native (24), and one Torres Strait Islander native (23); in Canada with four Ontario natives (25-28), three Alberta natives (28,29), one Vancouver native (28), and one Atikamekw native (30); in Guatemala with one Solol native (31) and one Mayan Kaqchikel native (32); in Queensland with one Cunnamulla native (33); and one in the United States with Alaska and Indians natives (34). The majority of research sites were the community (73.68%, n = 14), clinics (15.78%, n = 3), and primary health centers (10.52%, n = 2), as presented in Table 1.
Table 1.
Methodological Characteristics of the Included Articles (N = 19)
|
Characteristics
|
Categories
|
No.
|
%
|
| Research designs |
Qualitative |
9 |
42.1 |
| Cross-sectional |
2 |
10.52 |
| Cohort study |
1 |
5.26 |
| Randomized controlled trial |
3 |
15.78 |
| Mix method |
1 |
5.26 |
| Before/after study without a control group |
1 |
5.26 |
| Controlled intervention study |
2 |
10.52 |
| Targets of study |
Aborigine |
5 |
26.31 |
| Torres Strait Islander |
1 |
5.26 |
| Victoria |
1 |
5.26 |
| Alberta |
3 |
15,78 |
| Ontario |
5 |
26,31 |
| Vancouver |
1 |
5.26 |
| Atikamekw |
1 |
5.26 |
| Solol |
1 |
5.26 |
| Maya Kaqchikel |
1 |
5.26 |
| Indian |
1 |
5.26 |
| Alaska |
1 |
5.26 |
| Cunnamulla |
1 |
5.26 |
| Settings |
Clinic |
3 |
15.78 |
| Community |
14 |
73.68 |
| Primary health centers |
2 |
10.52 |
| Sampling techniques |
Purposive sampling |
4 |
21.05 |
| Snowball sampling |
3 |
15.78 |
| Cluster sampling |
1 |
5.26 |
| Convenience sampling |
1 |
5.26 |
| Non-probability sampling |
1 |
5.26 |
| Unavailable information |
10 |
52.63 |
Diabetes Care Challenges in Indigenous People
Trust
Trust from indigenous people seriously hinders their diabetes mellitus care. Indigenous people with diabetes mellitus have low confidence in various aspects to access health programs from the government and health workers (31). This condition is a result of social determinants of health and negative experiences in health services (35). Moreover, they face difficulties due to racism and discrimination (36). Discrimination exposure is associated with distress, low psychological coping mechanisms, and risky health behaviors (37); thus, this problem reflects racial pressure that can affect diabetes pressure in indigenous people with diabetes (38). Health workers must certainly respond to this condition by providing empathy-based health services and culture-based care for indigenous people. Such strategies can build a trusting relationship.
Language
Language frequently hampers indigenous people with diabetes to obtain health services because health services are not provided as expected. Language barriers can decrease access to health care, adherence to treatment, and follow-up treatment (39). The use of certain words or phrases can intentionally or unintentionally reveal personal characteristics such as race, religion, health, gender, and encouraging or discouraging motivations (40). Encouraging language binds messages and motivation to improve health outcomes; in contrast, discouraging language creates stressful life experiences for people with diabetes. Indigenous people’s non-fluency in using a common language is another factor that fails health workers to provide accurate health services (41).
Access to Healthcare and Treatment
Limited access to health services and treatment is very likely to aggravate diabetes mellitus in indigenous people. Health system disparities, limited access to medicines, and poor integration of diabetes services are complex and inseparable issues (42). Such conditions result in poor punctuality of care, retention, and poor coordination of patients. These problems can contribute to mortality, morbidity, cost wastage, and health-related suffering (43). Based on the patients’ perspectives, the most commonly reported challenge in accessing care is the lack of medical facilities. As a result, they are forced to purchase necessary medicines from private stores with unaffordable prices. Another frequently reported challenge is the high cost of services for glucose checks and medicines due to out-of-stock at public facilities (44). Other challenges include the lack of transportation due to long distances to facilities, long waiting times, sharing medical service points with other patients, delays in opening clinics, the lack of laboratory equipment/supplies, and an insufficient number of health personnel who provide diabetes services in health facilities (44). Doctors’ discrimination against indigenous patients is another obstacle to access to services and treatment (45).
Health Literacy
This study has found that indigenous people have low health literacy. Low health literacy is generally found in people with low levels of education but can be improved by providing necessary educational programs (46). Health literacy has a pivotal role in managing diabetes care. This statement is supported by (47) who asserted that adequate health literacy is significantly associated with better outcomes of diabetes disease (glycemic control, knowledge, and self-care). Thus, achieving better health literacy is an important goal to prevent and manage chronic conditions such as diabetes (48). In contrast, people with inadequate health literacy frequently have difficulties reading prescriptions, analyzing the risks of their medical procedures, and understanding or following instructions provided by health staff (49). Such a condition will ultimately worsen the care coordination and dissatisfaction between the two parties, leading to treatment dropouts (50). Indigenous people tend to have low health literacy because they do not understand the conveyed health information such as a condition that interferes with their disease self-management. Health literacy improves health care outcomes and service efficiency, promotes health equality (50), and measures the efficiency of awareness/education initiatives implemented by health authorities (51).
Cost
In addition to morbidity and mortality, diabetes causes a substantial economic burden on individuals, households, and health systems (52). These aspects are also the main reasons why patients with diabetes mellitus do not visit health facilities to treat the disease. There are also three other complete reasons. First, the distance from the house to the health facility center is quite far, so indigenous people require transportation costs (33). Second, indigenous people cannot afford health insurance, and the third reason is that drugs in private pharmacies require higher costs (53). Therefore, it is important to identify approaches, treatment cost-reduction strategies, and further investments to reduce the cost burden and prevent severe complications (54). Although a healthcare strategy can cut medical costs, health technology such as telehealth, is unavailable in outbacks (55).
Religion and Culture
Religion and culture are two separate barrier categories and supporting factors but overlap in many ways. For example, religious festivals frequently involve traditional food. A religious belief can become a barrier and opportunity factor. A study has proven this statement (56). Religion and culture have different options on how to interpret God’s will and how to inculcate diabetes mellitus in a religious context. The diagnosis of diabetes mellitus can be considered “God-given”, and this belief leads believers to surrender to the will of God (57). Another belief states that “not taking care of one’s body is against self-responsibility” (58). Several studies showed the importance of rice in many cultures in South Asian, African, and Latin communities. Preventive diets are frequently called Western diets, so it is less significantly accepted by indigenous people who consume traditional rice-based diets (59).
Opportunities To Care For Indigenous People with Diabetes
Opportunities for Indigenous Health Workers
This is a unique phenomenon of diabetes care for indigenous people. Involving health workers who come from the indigenous area is an important part to succeed the diabetes care (1). This is in line with the concept of patient trust, which states that patients will trust people from their group more than from strangers (60). Diabetes care for indigenous people is complicated to implement if it does not involve indigenous health workers who understand the local language and culture; moreover, indigenous health workers can accommodate the implementation of diabetes care (23). In addition, involving indigenous health workers can increase indigenous people’s confidence to encounter diabetes (61).
Intervention Modification Based on Culture, Language, and Technology
Some modified interventions that consider the needs and backgrounds (culture, beliefs, and language) of indigenous people provide significant results and effective care for their diabetes (62,63). In addition, to solve the problems of high costs and difficult service access gaps in diabetes care, indigenous people can employ technology-based modified interventions (32,33).
Support From Health Authority
The health authority is the main party that conducts diabetes care and makes health policies concerning the availability of medical/health personnel, health care facilities, and health technology development for indigenous people. The support from the health authority positively impacts the quality of health care (57) and improves health facilities because doctors and other health workers who continuously follow up patients’ health conditions are available (64).
Discussion
Aborigines and indigenous people in Ontario are the largest populations in this review. Although Aborigines are indigenous tribes of Australia, many of them not only occupy the Australian mainland but also Ontario, a province in Canada. Therefore, aborigine tribes and natives have always existed and become the population of many studies (65). Meanwhile, Ontario is home to 23% of all indigenous people in Canada. There are 133 First Nation communities located in Ontario, representing at least seven major cultural and linguistic groups (66).
Eight barrier categories and two opportunity factors are identified in each indigenous group. The most common opportunity factors are health authority support and support from native health workers which are similar in each indigenous group. Meanwhile, the most common barriers are limited knowledge due to low health literacy, lack of medical and health personnel support, and high cost. The differences between tribal groups, indigenous groups, and the most common barriers are minimal. Only one category of barriers can be attributed to one tribal and indigenous group, namely, language barriers. Other factors such as sufficient support from health authorities, the adequate assignment of medical personnel in the outback, and the availability of health access and health technology facilities can improve diabetes mellitus treatments designed for indigenous people (67). However, cultural factors seem to be exclusive and vital for indigenous people (Figure 2).
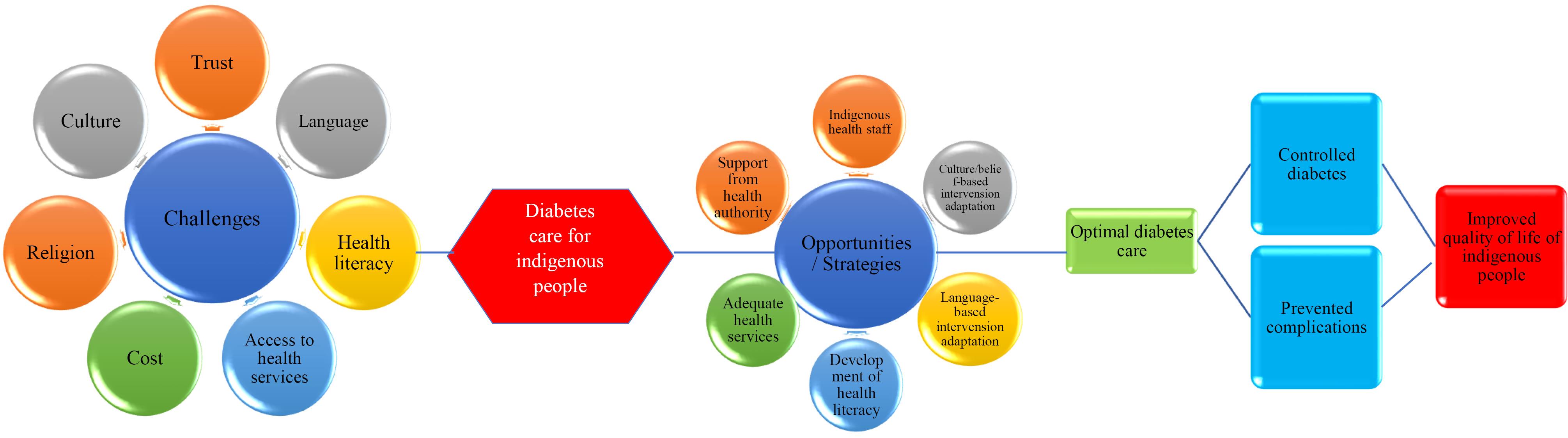
Figure 2.
Scheme of Diabetes Care for Indigenous People
.
Scheme of Diabetes Care for Indigenous People
Crucial considerations are needed to care for diabetes in indigenous people. Challenges and opportunity factors for indigenous people should be considered when developing diabetes care interventions for indigenous people. However, the religious and cultural backgrounds of the indigenous people should be considered separately; hence, it is necessary to find different approaches to care for diabetes in indigenous people.
All barrier and opportunity factors are relevantly identified to rural people and should be considered by adapting existing programs or developing new interventions specific to indigenous people. An example of intervention is diabetes self-management-based telehealth. This program is adapted to conduct diabetes care, specifically for indigenous people (62). The data-based diabetes self-management education and support (DSMES) intervention is culturally adapted to rural cities of the Mayan Tribe in Guatemala (63). Diabetes mellitus in indigenous people can be solved by directly modifying the existing interventions or adopting the culture of alternative food such as a rice-based diet. In addition, indigenous people’s trust in health authorities should be increased because it is a principle aspect to consider. More complex aspects such as the support of medical/health personnel or gender differences should be addressed by developing new preventive interventions for the target population.
In general, there are some similar challenges in managing diabetes in indigenous people and in the general society, including inadequate health literacy, a lack of support (68), health system and policy factors, availability and accessibility of resources (69), and high costs (53). However, the most significant challenges in managing diabetes in indigenous people are trust, cultural concerns, and language concerns.
Limitations
This study has some limitations. Ten studies do not provide enough information about sampling techniques. Meanwhile, others do not apply a scientific approach to sampling but rely on convenience sampling, and due to a lack of expert employees, this analysis excluded publications written in languages other than English. Moreover, since this study is a scoping review, it does not include levels of evidence and quality of evaluation.
Conclusion
To develop diabetes care in indigenous people, the existing challenges and opportunity factors must be considered, and adapted interventions can apply to indigenous people. Trust, language, health literacy, access to health services, and costs are common barriers for indigenous people. In addition, religious and cultural factors, in particular, require different approaches to deal with diabetes mellitus in indigenous people.
Authors’ Contribution
Conceptualization: Yusran Haskas.
Data curation: Suarnianti Suarnianti.
Formal analysis: Yusran Haskas.
Funding acquisition: Yusran Haskas.
Investigation: Suarnianti Suarnianti.
Methodology: Yusran Haskas.
Project administration: Suarnianti Suarnianti.
Resources: Indah Restika.
Software: Indah Restika.
Supervision: Yusran Haskas.
Validation: Suarnianti Suarnianti.
Visualization: Indah Restika.
Writing–original draft: Yusran Haskas.
Writing–review & editing: Suarnianti Suarnianti.
Competing Interests
The authors declare no conflict of interests.
Ethical Approval
Not applicable.
Funding
None.
Supplementary Files
Supplementary file 1. Search strategies used in this study
(pdf)
References
- Harris SB, Tompkins JW, TeHiwi B. Call to action: a new path for improving diabetes care for Indigenous peoples, a global review. Diabetes Res Clin Pract 2017; 123:120-33. doi: 10.1016/j.diabres.2016.11.022 [Crossref] [ Google Scholar]
- Schroth RJ, Halchuk S, Star L. Prevalence and risk factors of caregiver reported severe early childhood caries in Manitoba First Nations children: results from the RHS Phase 2 (2008-2010). Int J Circumpolar Health 2013;72. 10.3402/ijch.v72i0.21167.
- Macaulay AC, Montour LT, Adelson N. Prevalence of diabetic and atherosclerotic complications among Mohawk Indians of Kahnawake, PQ. CMAJ 1988; 139(3):221-4. [ Google Scholar]
- Crowshoe L, Dannenbaum D, Green M, Henderson R, Hayward MN, Toth E. Type 2 diabetes and Indigenous peoples. Can J Diabetes 2018; 42 Suppl 1:S296-306. doi: 10.1016/j.jcjd.2017.10.022 [Crossref] [ Google Scholar]
- Xie J, Ikram MK, Cotch MF, Klein B, Varma R, Shaw JE. Association of diabetic macular edema and proliferative diabetic retinopathy with cardiovascular disease: a systematic review and meta-analysis. JAMA Ophthalmol 2017; 135(6):586-93. doi: 10.1001/jamaophthalmol.2017.0988 [Crossref] [ Google Scholar]
- Ishtiaq I. Health disparities: diabetes prevalence in Indigenous populations. SFU Health Sciences Undergraduate Journal. 2022(1):1-11.
- Gregg EW, Lin J, Bardenheier B, Chen H, Rejeski WJ, Zhuo X. Impact of intensive lifestyle intervention on disability-free life expectancy: the look AHEAD study. Diabetes Care 2018; 41(5):1040-8. doi: 10.2337/dc17-2110 [Crossref] [ Google Scholar]
- Reading CL, Wien F. [Health Inequalities and Social Determinants of Health in Indigenous Peoples]. Prince George: Centre de Collaboration Nationale de la Santé Autochtone; 2009.
- Mosby I, Galloway T. “Hunger was never absent”: how residential school diets shaped current patterns of diabetes among Indigenous peoples in Canada. CMAJ 2017; 189(32):E1043-5. doi: 10.1503/cmaj.170448 [Crossref] [ Google Scholar]
- Tait CA, L’Abbé MR, Smith PM, Rosella LC. The association between food insecurity and incident type 2 diabetes in Canada: a population-based cohort study. PLoS One 2018; 13(5):e0195962. doi: 10.1371/journal.pone.0195962 [Crossref] [ Google Scholar]
- Sharp D. Environmental toxins, a potential risk factor for diabetes among Canadian Aboriginals. Int J Circumpolar Health 2009; 68(4):316-26. doi: 10.3402/ijch.v68i4.17372 [Crossref] [ Google Scholar]
- Brazionis L, Keech A, Ryan C, Brown A, O’Neal D, Boffa J. Associations with sight-threatening diabetic macular oedema among Indigenous adults with type 2 diabetes attending an Indigenous primary care clinic in remote Australia: a Centre of Research Excellence in Diabetic Retinopathy and Telehealth Eye and Associated Medical Services Network study. BMJ Open Ophthalmol 2021; 6(1):e000559. doi: 10.1136/bmjophth-2020-000559 [Crossref] [ Google Scholar]
- Tremblay MC, Graham J, Porgo TV, Dogba MJ, Paquette JS, Careau E. Improving cultural safety of diabetes care in Indigenous populations of Canada, Australia, New Zealand and the United States: a systematic rapid review. Can J Diabetes 2020; 44(7):670-8. doi: 10.1016/j.jcjd.2019.11.006 [Crossref] [ Google Scholar]
- Burrow S, Ride K. Review of Diabetes Among Aboriginal and Torres Strait Islander People. Australian Indigenous HealthInfoNet; 2016.
- Lockwood C, Dos Santos KB, Pap R. Practical guidance for knowledge synthesis: scoping review methods. Asian Nurs Res (Korean Soc Nurs Sci) 2019; 13(5):287-94. doi: 10.1016/j.anr.2019.11.002 [Crossref] [ Google Scholar]
- Peterson J, Pearce PF, Ferguson LA, Langford CA. Understanding scoping reviews: definition, purpose, and process. J Am Assoc Nurse Pract 2017; 29(1):12-6. doi: 10.1002/2327-6924.12380 [Crossref] [ Google Scholar]
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018; 169(7):467-73. doi: 10.7326/m18-0850 [Crossref] [ Google Scholar]
- Joanna Briggs Institute (JBI). The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI Scoping Reviews. JBI; 2015.
- Thomson H, Campbell M. “Narrative Synthesis” of Quantitative Effect Data in Cochrane Reviews: Current Issues and Ways Forward. University of Glasgow, Cochrane Training; 2020.
- Burgess A, Hawkins J, Kostovski C, Duncanson K. Assessing cultural appropriateness of patient-reported outcome measures for Aboriginal people with diabetes: study protocol. Public Health Res Pract 2022; 32(1):31122105. doi: 10.17061/phrp31122105 [Crossref] [ Google Scholar]
- McDermott RA, Schmidt B, Preece C, Owens V, Taylor S, Li M. Community health workers improve diabetes care in remote Australian Indigenous communities: results of a pragmatic cluster randomized controlled trial. BMC Health Serv Res 2015; 15:68. doi: 10.1186/s12913-015-0695-5 [Crossref] [ Google Scholar]
- Ekinci EI, Pyrlis F, Hachem M, Maple-Brown LJ, Brown A, Maguire G. Feasibility of once weekly exenatide-LAR and enhanced diabetes care in Indigenous Australians with type 2 diabetes (Long-acting-Once-Weekly-Exenatide laR-SUGAR, ‘Lower SUGAR’ study). Intern Med J 2021; 51(9):1463-72. doi: 10.1111/imj.15428 [Crossref] [ Google Scholar]
- Yashadhana A, Fields T, Blitner G, Stanley R, Zwi AB. Trust, culture and communication: determinants of eye health and care among Indigenous people with diabetes in Australia. BMJ Glob Health 2020; 5(1):e001999. doi: 10.1136/bmjgh-2019-001999 [Crossref] [ Google Scholar]
- Atkinson-Briggs S, Jenkins A, Keech A, Ryan C, Brazionis L. A model of culturally-informed integrated diabetes education and eye screening in Indigenous primary care services and specialist diabetes clinics: Study protocol. J Adv Nurs 2021; 77(3):1578-90. doi: 10.1111/jan.14734 [Crossref] [ Google Scholar]
- Slater M, Green ME, Shah B, Khan S, Jones CR, Sutherland R. First Nations people with diabetes in Ontario: methods for a longitudinal population-based cohort study. CMAJ Open 2019; 7(4):E680-8. doi: 10.9778/cmajo.20190096 [Crossref] [ Google Scholar]
- Jacklin K, Ly A, Calam B, Green M, Walker L, Crowshoe L. An innovative sequential focus group method for investigating diabetes care experiences with Indigenous peoples in Canada. Int J Qual Methods 2016; 15(1):1609406916674965. doi: 10.1177/1609406916674965 [Crossref] [ Google Scholar]
- Naqshbandi Hayward M, Pace R, Zaran H, Dyck R, Hanley AJ, Green ME. Closing the Indigenous health gap in Canada: results from the TransFORmation of IndiGEnous PrimAry HEAlthcare delivery (FORGE AHEAD) program. Diabetes Res Clin Pract 2020; 162:108066. doi: 10.1016/j.diabres.2020.108066 [Crossref] [ Google Scholar]
- Jacklin KM, Henderson RI, Green ME, Walker LM, Calam B, Crowshoe LJ. Health care experiences of Indigenous people living with type 2 diabetes in Canada. CMAJ 2017; 189(3):E106-12. doi: 10.1503/cmaj.161098 [Crossref] [ Google Scholar]
- Oster RT, Virani S, Strong D, Shade S, Toth EL. Diabetes care and health status of First Nations individuals with type 2 diabetes in Alberta. Can Fam Physician 2009; 55(4):386-93. [ Google Scholar]
- Tremblay MC, Bradette-Laplante M, Witteman HO, Dogba MJ, Breault P, Paquette JS. Providing culturally safe care to Indigenous people living with diabetes: identifying barriers and enablers from different perspectives. Health Expect 2021; 24(2):296-306. doi: 10.1111/hex.13168 [Crossref] [ Google Scholar]
- Nieblas-Bedolla E, Bream KDW, Rollins A, Barg FK. Ongoing challenges in access to diabetes care among the Indigenous population: perspectives of individuals living in rural Guatemala. Int J Equity Health 2019; 18(1):180. doi: 10.1186/s12939-019-1086-z [Crossref] [ Google Scholar]
- Duffy S, Norton D, Kelly M, Chavez A, Tun R, de Guzmán Ramírez MN. Using community health workers and a smartphone application to improve diabetes control in rural Guatemala. Glob Health Sci Pract 2020; 8(4):699-720. doi: 10.9745/ghsp-d-20-00076 [Crossref] [ Google Scholar]
- Snoswell CL, Caffery LJ, Haydon HM, Wickramasinghe SI, Crumblin K, Smith AC. A cost-consequence analysis comparing patient travel, outreach, and telehealth clinic models for a specialist diabetes service to Indigenous people in Queensland. J Telemed Telecare 2019; 25(9):537-44. doi: 10.1177/1357633x19873239 [Crossref] [ Google Scholar]
- Jiang L, Johnson A, Pratte K, Beals J, Bullock A, Manson SM. Long-term outcomes of lifestyle intervention to prevent diabetes in American Indian and Alaska native communities: the special diabetes program for Indians diabetes prevention program. Diabetes Care 2018; 41(7):1462-70. doi: 10.2337/dc17-2685 [Crossref] [ Google Scholar]
- Conway J, Tsourtos G, Lawn S. The barriers and facilitators that Indigenous health workers experience in their workplace and communities in providing self-management support: a multiple case study. BMC Health Serv Res 2017; 17(1):319. doi: 10.1186/s12913-017-2265-5 [Crossref] [ Google Scholar]
- Wagner JA, Tennen H, Finan PH, Ghuman N, Burg MM. Self-reported racial discrimination and endothelial reactivity to acute stress in women. Stress Health 2013; 29(3):214-21. doi: 10.1002/smi.2449 [Crossref] [ Google Scholar]
- Pieterse AL, Todd NR, Neville HA, Carter RT. Perceived racism and mental health among Black American adults: a meta-analytic review. J Couns Psychol 2012; 59(1):1-9. doi: 10.1037/a0026208 [Crossref] [ Google Scholar]
- Fisher L, Mullan JT, Arean P, Glasgow RE, Hessler D, Masharani U. Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care 2010; 33(1):23-8. doi: 10.2337/dc09-1238 [Crossref] [ Google Scholar]
- Okrainec K, Booth GL, Hollands S, Bell CM. Impact of language barriers on complications and mortality among immigrants with diabetes: a population-based cohort study. Diabetes Care 2015; 38(2):189-96. doi: 10.2337/dc14-0801 [Crossref] [ Google Scholar]
- Dickinson JK, Guzman SJ, Maryniuk MD, O’Brian CA, Kadohiro JK, Jackson RA. The use of language in diabetes care and education. Diabetes Care 2017; 40(12):1790-9. doi: 10.2337/dci17-0041 [Crossref] [ Google Scholar]
- Beaton A, Manuel C, Tapsell J, Foote J, Oetzel JG, Hudson M. He Pikinga Waiora: supporting Māori health organisations to respond to pre-diabetes. Int J Equity Health 2019; 18(1):3. doi: 10.1186/s12939-018-0904-z [Crossref] [ Google Scholar]
- Nuche-Berenguer B, Kupfer LE. Readiness of sub-Saharan Africa healthcare systems for the new pandemic, diabetes: a systematic review. J Diabetes Res 2018; 2018:9262395. doi: 10.1155/2018/9262395 [Crossref] [ Google Scholar]
- Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob Health 2018; 6(11):e1196-252. doi: 10.1016/s2214-109x(18)30386-3 [Crossref] [ Google Scholar]
- Birabwa C, Bwambale MF, Waiswa P, Mayega RW. Quality and barriers of outpatient diabetes care in rural health facilities in Uganda - a mixed methods study. BMC Health Serv Res 2019; 19(1):706. doi: 10.1186/s12913-019-4535-x [Crossref] [ Google Scholar]
- McConkey S. Indigenous access barriers to health care services in London, Ontario: the “engaging for change improving health services for Indigenous peoples” qualitative study. Univ West Ont Med J 2017; 86(2):6-9. doi: 10.5206/uwomj.v86i2.1407 [Crossref] [ Google Scholar]
- Saleh A, Wirda W, Irwan AM, Latif AI. The relationships among self-efficacy, health literacy, self-care and glycemic control in older people with type 2 diabetes mellitus. Work Older People 2021; 25(2):164-9. doi: 10.1108/wwop-08-2020-0044 [Crossref] [ Google Scholar]
- Marciano L, Camerini AL, Schulz PJ. The role of health literacy in diabetes knowledge, self-care, and glycemic control: a meta-analysis. J Gen Intern Med 2019; 34(6):1007-17. doi: 10.1007/s11606-019-04832-y [Crossref] [ Google Scholar]
- Nutbeam D, Levin-Zamir D, Rowlands G. Health literacy and health promotion in context. Glob Health Promot 2018; 25(4):3-5. doi: 10.1177/1757975918814436 [Crossref] [ Google Scholar]
- Eberle ML, Clark D. NN/LM NER Healthy Community, Community of Interest Final Report (May 1, 2011-April 30, 2013). UMass Chan Medical School; 2013. p. 1-7. 10.13028/k4pk-ab70.
- Singh S, Acharya SD, Kamath A, Ullal SD, Urval RP. Health literacy status and understanding of the prescription instructions in diabetic patients. J Diabetes Res 2018; 2018:4517243. doi: 10.1155/2018/4517243 [Crossref] [ Google Scholar]
- Dahal PK, Hosseinzadeh H. Association of health literacy and diabetes self-management: a systematic review. Aust J Prim Health 2019; 25(6):526-33. doi: 10.1071/py19007 [Crossref] [ Google Scholar]
- World Health Organization (WHO). Global Report on Diabetes. WHO; 2016.
- Gao CC, Espinoza Suarez NR, Toloza FJK, Malaga Zuniga AS, McCarthy SR, Boehmer KR. Patients’ perspective about the cost of diabetes management: an analysis of online health communities. Mayo Clin Proc Innov Qual Outcomes 2021; 5(5):898-906. doi: 10.1016/j.mayocpiqo.2021.07.003 [Crossref] [ Google Scholar]
- Moucheraud C, Lenz C, Latkovic M, Wirtz VJ. The costs of diabetes treatment in low- and middle-income countries: a systematic review. BMJ Glob Health 2019; 4(1):e001258. doi: 10.1136/bmjgh-2018-001258 [Crossref] [ Google Scholar]
- Ciemins E, Coon P, Peck R, Holloway B, Min SJ. Using telehealth to provide diabetes care to patients in rural Montana: findings from the promoting realistic individual self-management program. Telemed J E Health 2011; 17(8):596-602. doi: 10.1089/tmj.2011.0028 [Crossref] [ Google Scholar]
- Bhattacharya G. Spirituality and type 2 diabetes self-management among African Americans in the Arkansas Delta. J Soc Serv Res 2013; 39(4):469-82. doi: 10.1080/01488376.2011.647989 [Crossref] [ Google Scholar]
- Isabekova G. Healthcare workers in the Southern Caucasus: availability, migration and patients’ access to healthcare. Caucasus Analytical Digest. 2018(103):6-17. 10.3929/ethz-b-000269801.
- Jesus TS, Bhattacharjya S, Papadimitriou C, Bogdanova Y, Bentley J, Arango-Lasprilla JC. Lockdown-related disparities experienced by people with disabilities during the first wave of the COVID-19 pandemic: scoping review with thematic analysis. Int J Environ Res Public Health 2021; 18(12):6178. doi: 10.3390/ijerph18126178 [Crossref] [ Google Scholar]
- Moise RK, Conserve DF, Elewonibi B, Francis LA, BeLue R. Diabetes knowledge, management, and prevention among Haitian immigrants in Philadelphia. Diabetes Educ 2017; 43(4):341-7. doi: 10.1177/0145721717715418 [Crossref] [ Google Scholar]
- Gucciardi E, Richardson A, Aresta S, Karam G, Sidani S, Beanlands H, et al. Storytelling to support disease self-management by adults with type 2 diabetes. Can J Diabetes 2019;43(4):271-7.e1. 10.1016/j.jcjd.2018.06.004.
- Babagoli MA, Nieto-Martínez R, González-Rivas JP, Sivaramakrishnan K, Mechanick JI. Roles for community health workers in diabetes prevention and management in low- and middle-income countries. Cad Saude Publica 2021; 37(10):e00287120. doi: 10.1590/0102-311x00287120 [Crossref] [ Google Scholar]
- Litchman ML, Kwan BM, Zittleman L, Simonetti J, Iacob E, Curcija K. A telehealth diabetes intervention for rural populations: protocol for a randomized controlled trial. JMIR Res Protoc 2022; 11(6):e34255. doi: 10.2196/34255 [Crossref] [ Google Scholar]
- Tschida S, Flood D, Guarchaj M, Milian J, Aguilar A, Fort MP. Implementation of a diabetes self-management education and support intervention in rural Guatemala: a mixed-methods evaluation using the RE-AIM framework. Prev Chronic Dis 2021; 18:E100. doi: 10.5888/pcd18.210259 [Crossref] [ Google Scholar]
- Lamarche PA, Pineault R, Gauthier J, Hamel M, Haggerty J. Availability of healthcare resources, positive ratings of the care experience and extent of service use: an unexpected relationship. Healthc Policy 2011; 6(3):46-56. doi: 10.12927/hcpol.2011.22178 [Crossref] [ Google Scholar]
- Kelly-Scott K, Smith K. Aboriginal Peoples: Fact Sheet for Canada. No 89. Ottawa: Statistics Canada; 2015. p. 1-9.
- Government of Canada. First Nation Profiles. Government of Canada; 2014.
- Butzner M, Cuffee Y. Telehealth interventions and outcomes across rural communities in the United States: narrative review. J Med Internet Res 2021; 23(8):e29575. doi: 10.2196/29575 [Crossref] [ Google Scholar]
- Shi C, Zhu H, Liu J, Zhou J, Tang W. Barriers to self-management of type 2 diabetes during COVID-19 medical isolation: a qualitative study. Diabetes Metab Syndr Obes 2020; 13:3713-25. doi: 10.2147/dmso.s268481 [Crossref] [ Google Scholar]
- Adhikari M, Devkota HR, Cesuroglu T. Barriers to and facilitators of diabetes self-management practices in Rupandehi, Nepal- multiple stakeholders’ perspective. BMC Public Health 2021; 21(1):1269. doi: 10.1186/s12889-021-11308-4 [Crossref] [ Google Scholar]