J Educ Community Health. 11(3):163-169.
doi: 10.34172/jech.2951
Original Article
Celiac Disease: From Adherence to Gluten-Free Diet to Health-Related Quality of Life
Ehsan Vesali-Monfared 1  , Abolfazl Mohammadbeigi 2
, Abolfazl Mohammadbeigi 2  , Sarallah Shojaei 3
, Sarallah Shojaei 3  , Rahim Aali 4
, Rahim Aali 4  , Aazam Farahanie 5
, Aazam Farahanie 5  , Mohammad Reza Ghadir 5, *
, Mohammad Reza Ghadir 5, * 
Author information:
1Department of Gastroenterology and Hematology Diseases Research Center, Shahid Beheshti Hospital, Qom University of Medical Sciences, Qom, Iran
2Department of Biostatistics and Epidemiology, School of Health, Research Center for Environmental Pollutants, Qom University of Medical Sciences, Qom, Iran
3Department of Nursing and Midwifery, School of Nursing, Qom University of Medical Sciences, Qom, Iran
4Department of Environmental Health, School of Health, Research Center for Environmental Pollutants, Qom University of Medical Sciences, Qom, Iran
5Department of Internal Medicine, School of Medicine, Gastroenterology and Hepatology Diseases Research Center, Shahid Beheshti Hospital, Qom University of Medical Sciences, Qom, Iran
Abstract
Background: Celiac disease (CD) is a genetic and immune-mediated disorder in which eating gluten reduces intestinal absorption and damages the mucosa and villi of the small intestine. This study was designed to investigate adherence to a gluten-free diet (GFD) and health-related quality of life (QOL).
Methods: This cross-sectional study was conducted on 122 patients with CD in Qom in 2023. Sampling was performed in an easy and accessible way from celiac patients. The research tool was a researcher-made questionnaire. The obtained data were analyzed by descriptive and inferential statistical tests using SPSS 23.
Results: The average age of the patients was 37.57±9.59 years, and 93% had a GFD. Gastrointestinal symptoms demonstrated a positive and significant correlation with GFD, age, marital status, and QOL (P<0.001). The percentage of patients’ QOL scores (39.57%) was lower than the average. Adherence to a GFD could predict favorable changes in patients’ QOL (β=0.71, P<0.001), and CD predicted gastrointestinal symptoms (β=0.64, P<0.001). The study model showed a good fit based on two important indicators of good model fit (χ2 /pdf=2.14 and RMSEA=0.069).
Conclusion: The results revealed that better adherence to the GFD leads to a better clinical response and a decrease in gastrointestinal symptoms, thereby improving the QOL of celiac patients.
Keywords: Celiac disease, Adherence, Gluten-free diet, Quality of life
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Vesali-Monfared E, Mohammadbeigi A, Shojaei S, Aali R, Farahanie A, Ghadir MR. Celiac disease: from adherence to gluten-free diet to health-related quality of life. J Educ Community Health. 2024; 11(3):163-169. doi:10.34172/jech.2951
Introduction
Celiac disease (CD) is a common genetic and immune-mediated disability that destroys the mucosa and villi of the small intestine and reduces the absorption capacity of the intestine by eating gluten, which is present in many grains similar to wheat (1). People with CD may have gastrointestinal signs, extra-intestinal signs, or no signs at all. Generally, the CD is associated with symptoms of malabsorption, such as diarrhea, steatorrhea, and weight loss (2,3).
These gastrointestinal specifications and pathological processes emerge as an outcome of gluten-mediated intestinal damage (4). According to the results of studies, the prevalence of CD is about 0.7%–1% worldwide (5). In recent years, CD has been introduced as a public health issue. Numerous studies have estimated that the disease affects approximately 1% of the European population. Population-based data on CD prevalence have also been reported from the Middle East, India, and the like (5). The prevalence of the disease in Central Asia and Iran is similar and equals 1%–2%, which is twice as much in women as in men (6). The clinical manifestations of CD change according to the age of the patient, the duration of the malady, and its severity, and it varies from asymptomatic patients to patients with severe malnutrition (7). Various demographic factors related to the disease and treatment can also affect the severity of the disease (8). The only effective and safe treatment for this sickness is to eliminate foods and products containing gluten (2,9). Although it is possible to control the disease and its complications with a strict gluten-free diet (GFD) and stop the autoimmune response, following this diet has serious consequences for patients’ social activities and mental and physical stress caused by this challenge. It may affect the quality of life (QOL) of these patients (4,10). In addition, various studies have shown that following a GFD has a physical and psychological effect on the health-related QOL (HRQOL) in patients with CD. Due to the feature of this disease and given that the duration of adherence to a GFD is costly and requires more energy, the HRQOL of these patients can be severely pretentious by this issue (11). It is expected that the gastrointestinal symptoms associated with CD can explain the quality and extent of dietary compliance in patients with CD (9,12). It is also predicted that adherence to GFD can have a significant impact on the HRQOL of patients with CD through changes in the severity of gastrointestinal symptoms (13-15). Therefore, the current study was implemented to investigate adherence to a GFD and related health QOL.
Materials and Methods
This cross-sectional survey was performed on celiac patients in the Gastroenterology and Liver Diseases Research Center, CD Group in Qom from June to December 2023. Sampling was conducted in an easy and accessible way and among patients who met the inclusion criteria. Suffering from this disease based on special gastrointestinal diagnostic tests (serology, endoscopy, biopsy, and tissue transglutaminase antibody test) and having a GFD diet for at least 6 months were the indications and criteria for entering the study. In case of not completing the informed consent form and the questionnaire, it was possible to exclude from the research. The sample size for the current research was based on the studies performed by Mohammadibakhsh et al (6) and Deepak et al (16), considering the prevalence of CD of 1%, the mean QOL score of 37.20 ± 11.09, the confidence interval of 95%, and d = 2 (accuracy between one-tenth and three-tenths of a standard deviation). Given a 10% attrition rate, the minimum sample size required for this study was estimated at 122 individuals.
A standard questionnaire was used for data collection, which was employed and evaluated in terms of validity and reliability in previous studies. The first part included demographic information, and the second section contained seven questions regarding awareness of CD. The questions were recorded on a dichotomous (yes/no) scale. For each correct or wrong answer, a score of 1 or 0 was considered, respectively, and the total score ranged from 0 to 7. Internal consistency of the questionnaire was assessed using Cronbach’s alpha value considered acceptable at 0.60 (17).
The third part of the questionnaire encompassed questions on the Gastrointestinal Symptom Rating Scale (GSRS). This questionnaire has 14 questions. Each question is scored on a 5-point Likert-type scale from no discomfort (1) to severe discomfort (5), and the total score ranges from 14 to 70. Moreover, it has 4 dimensions, namely, abdominal pain (heart pain, hunger, and nausea), diarrhea (diarrhea, loose stools, and urgent need to defecate), constipation (constipation, hard stools, and feeling of incomplete defecation), and indigestion (abdominal cramping, flatulence, belching, and increased abdominal gas). The total score is obtained from the sum of the average scores in each subscale, and the increase in the score in this scale indicates the severity of the symptoms, according to Cronbach’s alpha, 0.62, 0.83, and 0.80, respectively (18). A Cronbach’s alpha of 0.70 was estimated in this study. The fourth part included items related to adherence to GFD. Compatibility with the diet was assessed using the CD adherence test (CDAT) questionnaire, which evaluates adherence to a GFD using seven items on a 5-point Likert-type scale, and the total score ranges from 7 to 35. (19). Finally, the fifth part was related to questions about patients’ HRQOL. HRQOL in people with CD was evaluated using the HRQOL-SF36 standard questionnaire. This is a 36-question questionnaire that assesses physical and mental health. Scores in this questionnaire range from 0 to 100. The reliability and validity of the Persian version of this questionnaire (r = 1.9-1.7) have been confirmed in Iran (20). After data collection, all analyses were performed using SPSS software, version 23. The normality of the data distribution was assessed using the Kolmogorov-Smirnov test, and the frequency and descriptive variables were evaluated using analytical tests. In addition, the Pearson correlation test was utilized to determine the correlation between variables. Further, a regression test was employed to measure the effect of variables and predict what the QOL as a dependent variable would be with each change in the independent variables. Structural equation modeling was performed using Amos 26 software to determine the goodness-of-fit indices of the model. The value of the significance level was considered 0.05. This study has been registered at Qom University of Medical Sciences (ethical code IR.MUQ.REC.1402.107).
Results
Overall, 122 participants with CD with a mean age of 37.57 ± 9.59 years were examined in this research. Of these, 80 (66%) were women, 55 (46%) were married, and 115 patients (93%) had and followed a GFD. The mean duration of the disease was 2.1 ± 04.05 years (Table 1). Pearson correlation coefficients between the study constructs (Table 2) revealed a positive and significant correlation between a GFD and the duration of the diet with CD. A significant correlation was also found between GFD and the duration of adherence to the diet. Statistically, a positive and significant statistical relationship was reported between QOL and adherence to the GFD (P < 0.001).
Table 1.
Frequency Distribution of Demographic Characteristics (N = 122)
|
Variables
|
Category
|
Frequency
|
Percent
|
| Age |
1-20 |
54 |
44.5 |
| 21-40 |
36 |
29.5 |
| 40-60 |
32 |
26 |
| Gender |
Male |
42 |
34 |
| Female |
80 |
66 |
| Marital status |
Single |
67 |
54 |
| Marriage |
55 |
46 |
| Level of education |
Diploma |
85 |
69 |
| BSc |
28 |
23 |
| MSc/PhD |
9 |
8 |
| Job-status |
Self-employed |
19 |
15.5 |
| Employee |
18 |
14.5 |
| Retired |
4 |
3 |
| Scholar |
41 |
33.5 |
| Unemployed |
40 |
33 |
| Duration disease |
1-3 |
52 |
43 |
| 4-6 |
26 |
21 |
| 7-10 |
31 |
25 |
| > 11 |
13 |
11 |
| GFD regime |
Yes |
115 |
93 |
| No |
7 |
7 |
| GFD duration |
0-5 |
80 |
65 |
| 6-10 |
32 |
26.5 |
| > 11 |
10 |
8.5 |
| GFD adherence |
Yes |
112 |
92 |
| No |
10 |
8 |
Note. GFD: Gluten-free diet.
Table 2.
Pearson Correlation Coefficients Between the Study’s Constructs (N = 122)
|
Variables
|
1
|
2
|
3
|
4
|
5
|
6
|
7
|
| Duration disease |
1 |
|
|
|
|
|
|
| GFD regime |
-0.211* |
1 |
|
|
|
|
|
| GFD duration |
0.776** |
-0.304** |
1 |
|
|
|
|
| Knowledge |
-0.030 |
-0.172 |
-0.081 |
1 |
|
|
|
| GSRS |
0.082 |
0.167 |
-0.049 |
-0.229* |
1 |
|
|
| CDAT |
-0.048 |
-0.001 |
-0.050 |
-0.039 |
0.254** |
1 |
|
| Quality of life |
-0.058 |
0.072 |
-0.096 |
-0.141 |
0.463** |
0.111 |
1 |
Note. GFD: Gluten-free diet; GSRS: Gastrointestinal Symptom Rating Scale; CDAT: Celiac disease adherence test. **Correlation is significant at the 0.01 level. *Correlation is significant at the 0.05 level.
Among the constructs of the model, the highest mean percentage of points was related to awareness, followed by adherence to a GFD. The percentage of patients’ HRQOL scores (39.57%) was reported as below average (Table 3).
Table 3.
Mean, Standard Deviation, and Score Range of the Study’s Constructs (N = 122)
|
Variables
|
M (SD)
|
Score Range
|
Mean Percentage of Achievable Score*
|
| Knowledge |
3.51 (.946) |
0-6 |
58.5 |
| CDAT |
22.01 (3.59) |
7-35 |
53.6 |
| GSRS |
28.27 (11.43) |
14-70 |
25.3 |
| Physical quality of life |
36.24 (5.86) |
28-54 |
31.6 |
| Mental quality of life |
40.18 (4.06) |
31-51 |
45.9 |
| Total quality of life |
40.18 (6.36) |
1-100 |
39.57 |
Note.CDAT: Celiac disease adherence test; GSRS: Gastrointestinal Symptom Rating Scale; M: Mean; SD: Standard deviation. * Calculation: (Mean − Minimum) ÷ (Maximum − Minimum) × 100
The results of regression analysis for predicting HRQOL are presented in Table 4. The findings demonstrated that in stage 1, demographic characteristics could explain 1.9% of the variance in HRQOL (P = 0.206). By adding the disease duration variable and having a GFD, the duration of the GFD in stage 2 increased the variance of the HRQOL by 3.6% (P = 0.13). Eventually, dimensions of consciousness structure, GSRS, and CDAT were added to the model, which could generally explain 17% of the variance of HRQOL (P< 0.001).
Table 4.
Hierarchical Regression Analysis to Determine and Predict Health-Related Quality of Life
|
Variables
|
B
|
SE
|
Beta
|
P
value
|
95.0% Confidence Interval for B
|
|
Lower Bound
|
Upper Bound
|
| Age |
-0.235 |
1.005 |
-0.031 |
0.815 |
-2.226 |
1.756 |
| Gender |
0.934 |
1.280 |
0.070 |
0.467 |
-1.603 |
3.471 |
| Marital status |
0.684 |
1.478 |
0.054 |
0.644 |
-2.244 |
3.613 |
| Job |
-0.566 |
0.453 |
-0.130 |
0.215 |
-1.464 |
0.333 |
| Education |
-1.530 |
1.009 |
-0.149 |
0.133 |
-3.530 |
0.471 |
| Duration disease |
-0.545 |
0.849 |
-0.090 |
0.522 |
-2.227 |
1.137 |
| GFD regime |
-2.996 |
2.973 |
-0.110 |
0.316 |
-8.887 |
2.896 |
| GFD regime duration |
0.012 |
1.317 |
0.001 |
0.992 |
-2.598 |
2.623 |
| GFD adherence |
2.871 |
2.479 |
0.124 |
0.249 |
-2.042 |
7.784 |
| Knowledge |
-0.411 |
0.606 |
-0.061 |
0.499 |
-1.611 |
0.789 |
| GSRS |
0.242 |
0.056 |
0.435 |
0.000 |
0.131 |
0.353 |
| CDAT |
-0.054 |
0.160 |
-0.030 |
0.737 |
-.371 |
0.263 |
| Adjusted R2 = 0.17, R = 0.50, P < 0.001 |
Note. GFD: Gluten-free diet; GSRS: Gastrointestinal Symptom Rating Scale; CDAT: Celiac disease adherence test; SE: Standard error.
The correlation between compliance to a GFD and gastrointestinal signs on HRQOL was analyzed through the path analysis model (Table 5). According to the results, adherence to a GFD was able to explain the changes in HRQOL in patients (β = 0.71, P < 0.001). The effect of gastrointestinal signs on the HRQOL was significant (β = 0.27, P< 0.05). Further, this model assessed the predictive power of CDAT related to changes in GSRS (P < 0.001, β = 0.64). The results of structural equation modeling showed that two very important indicators of the goodness of fit of the model (χ2/df = 2.14 and RMSEA = 0.069) were at the desirable and acceptable threshold. Furthermore, the goodness of fit index of the model (GFI = 0.902), adjusted fit (AGFI = 0.878), and relative fit (CFI = 0.905) were reported as acceptable. Other indications of the goodness of fit of the structural model are displayed in Figures 1 and 2 (CFI = 0.905, NFI = 0.714, TLI = 0.862, AGFI = 0.878, CMIN = 4034.698, df = 1884, χ2/df = 2.14, and RMSEA = 0.069).
Table 5.
Regression Weights Between Structural Parameters Using Structural Equation Modeling (N = 122)
|
Variables
|
Relationship
|
Variables
|
Estimate
|
SE*
|
Test Statistics
|
P
value
|
| Knowledge |
→ |
CDAT |
-0.518 |
0.722 |
-3.809 |
P< 0.001 |
| Knowledge |
→ |
GSR |
-0.114 |
0.447 |
-0.945 |
P= 0.345 |
| Knowledge |
→ |
QOL |
0.059 |
0.404 |
0.628 |
P= 530 |
| CDAT* |
→ |
GSR |
0.649 |
0.117 |
3.823 |
P< 0.001 |
| GFD adherence |
→ |
QOL* |
0.713 |
0.152 |
3.798 |
P< 0.001 |
| GSRS* |
→ |
QOL |
0.274 |
0.150 |
2.127 |
P< 0.05 |
Note. *CDAT: Celiac disease adherence test; GSRS: Gastrointestinal Syndrome Rating Scale; QOL: Quality of life; SE: Standard error.
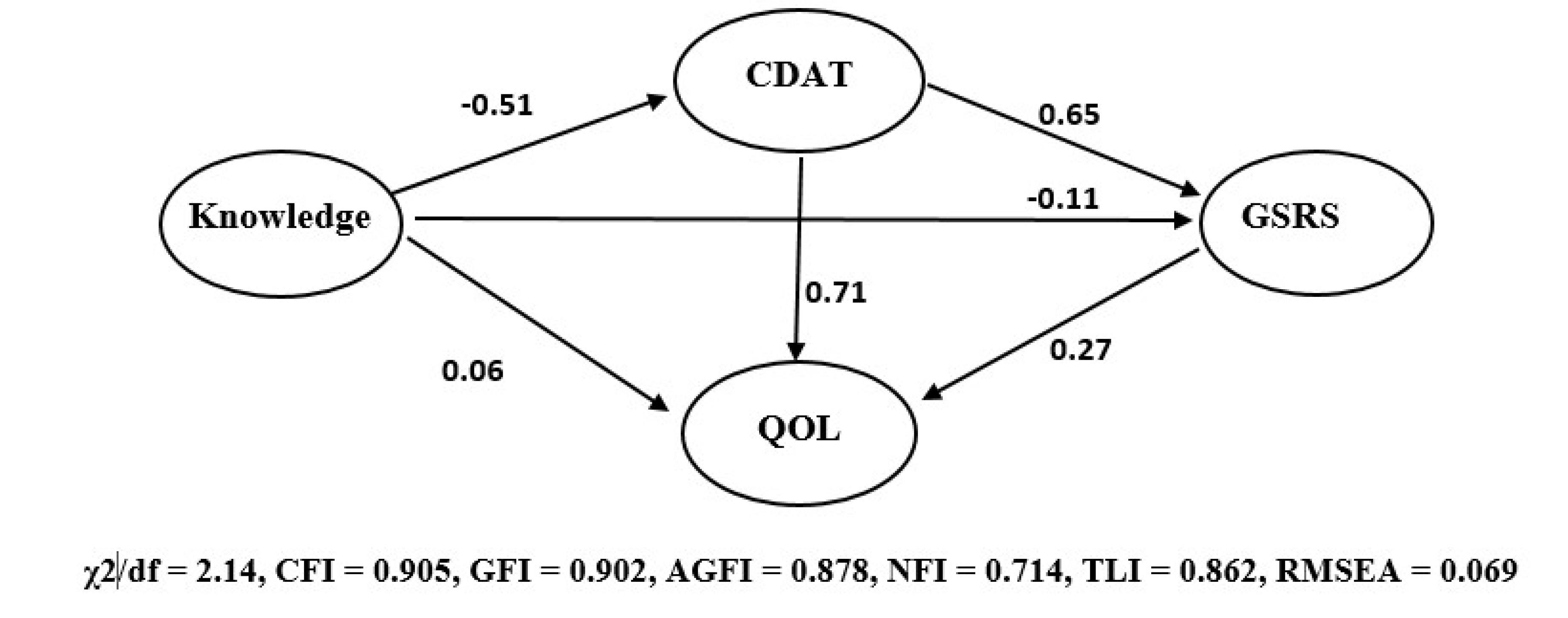
Figure 1.
Estimated Standardized Direct Effects for the Proposed Model. Note. df: Degree of freedom; CFI: Comparative fit index; GFI: Goodness-of-fit index; AGFI: Adjusted goodness-of-fit index; NFI: Normed fit index; TLI: Tucker-Lewis index; RMSEA: Root mean square error of approximation.
.
Estimated Standardized Direct Effects for the Proposed Model. Note. df: Degree of freedom; CFI: Comparative fit index; GFI: Goodness-of-fit index; AGFI: Adjusted goodness-of-fit index; NFI: Normed fit index; TLI: Tucker-Lewis index; RMSEA: Root mean square error of approximation.
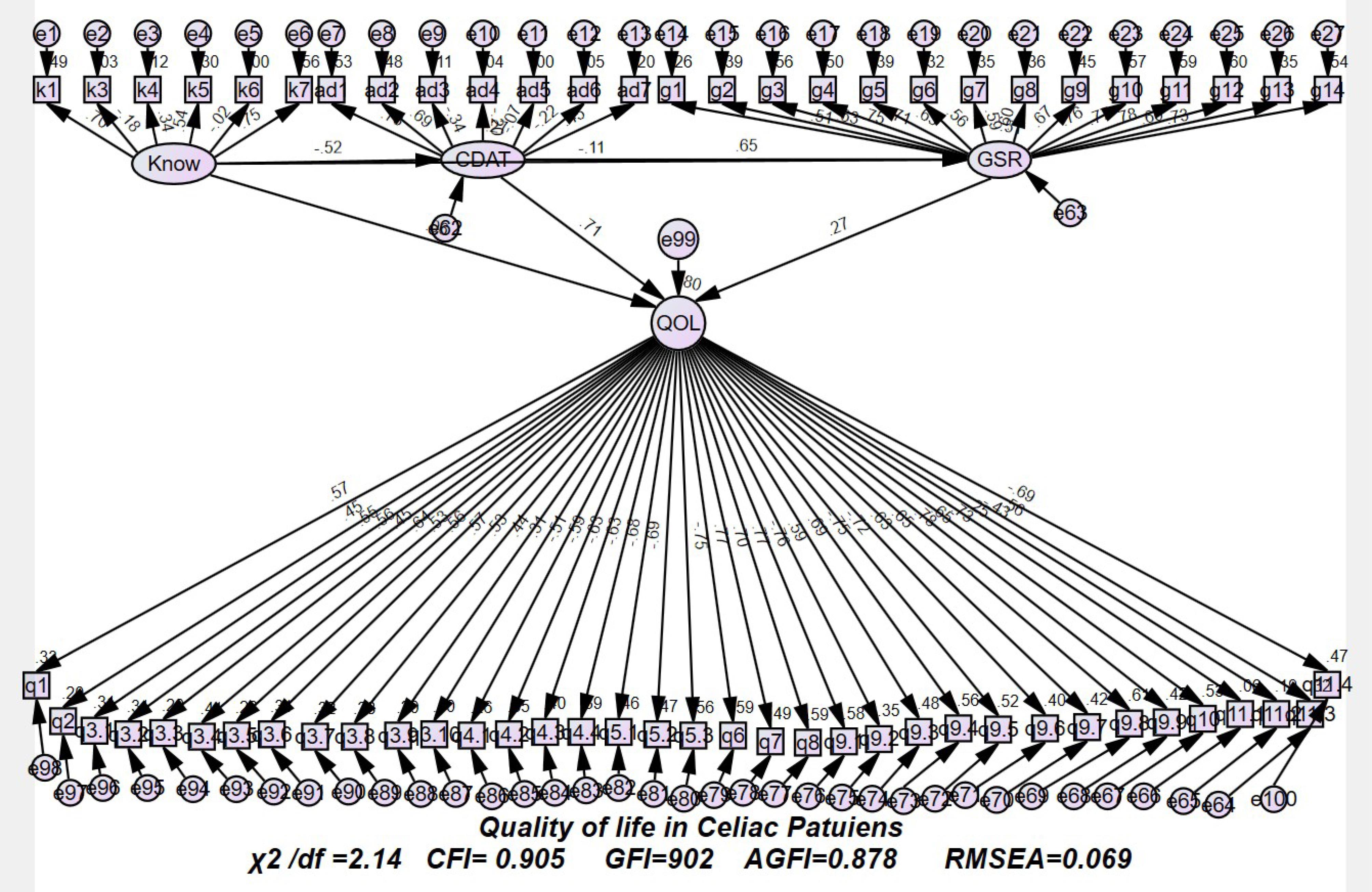
Figure 2.
Estimated Standardized Direct Effects for the Proposed Model Using Structural Equation Modeling. Note. df: Degree of freedom; CFI: Comparative fit index; GFI: Goodness-of-fit index; AGFI: Adjusted goodness-of-fit index; RMSEA: Root mean square error of approximation.
.
Estimated Standardized Direct Effects for the Proposed Model Using Structural Equation Modeling. Note. df: Degree of freedom; CFI: Comparative fit index; GFI: Goodness-of-fit index; AGFI: Adjusted goodness-of-fit index; RMSEA: Root mean square error of approximation.
Discussion
CD is a principal public health problem globally caused by gluten in hereditary predisposed people. This disease is of great importance due to its high prevalence, occurrence of the disease at any age, wide range of clinical pretense, and late diagnosis (3). Variables that determine the HRQOL in these patients remain largely unknown (8). Therefore, this survey investigated CD, focusing on adherence to a GFD and health-related QOL in patients suffering from this disease.
In the current research, a significant relationship was observed between GSRS and QOL. The average HRQOL score was below average, and the path coefficient represented that CDAT with the maximum grade predicted changes in HRQOL. In general, 92% of the studied population adhered to the GFD based on the GFD adherence questions, which is in line with the results of the study of Casellas et al, indicating an adherence rate of 71.5% (21).
Based on the findings, adherence to a GFD had a remarkable correlation with HRQOL. Moreover, a significant correlation was found between GSRS and QOL, which conforms to the results of Nikniaz et al (8). In line with the present findings, those of the study by Deepak et al (16) demonstrated a positive statistical relationship between compliance with GFD and HRQOL. Likewise, Rajpoot et al (22) and Sainsbury et al (23) concluded that adherence to GFD will reduce gastrointestinal symptoms in patients with CD and improve HRQOL. Analysis based on HRQOL revealed that better HRQOL was associated with fewer gastrointestinal symptoms and better adherence. In other words, the gradual decrease in the HRQOL and the possible increase in the symptoms of the disease will be related to the increase in the degree of difficulty in adhering to the treatment. Therefore, adaptation has been suggested as an autonomous variable intricate in the HRQOL of participants (23).
In this research, there was no statistical connection between the duration of adaptation to a GFD and HRQOL. The current findings contradict those of the study performed by Enaud et al, indicating that there was a statistical relationship between the duration of following a GFD and the HRQOL of celiac patients (14).
Our results confirmed that the gastrointestinal symptoms related to CD have a statistically significant and positive correlation with adaptation to a GFD, which corroborates the results of previous research (14). It appears to be an association between reduced gastrointestinal signs and greater compliance with the GFD. However, because of the feasible interplay between CD and irritable bowel syndrome or inflammatory bowel disease, it is difficult to interpret the level of gastrointestinal signs in people with CD and its association with compliance with a GFD (12).
The demographic findings of this survey demonstrated that there was no significant correlation between age and marital status with GFD and even CDAT. The outcome of this survey is consistent with that of the study conducted by Barratt et al (24). The average score of the HRQOL of the participants of the present research was lower than the average, while in the study by Wolf et al (25), the average HRQOL was reported as favorable and moderate to high. This inconsistency may be partly due to differences in QOL instruments (general vs. CD specific), differences in dietary adherence instruments (self-reporting of dietary data), or geographic location. In this study, valid measures of QOL (HRQOL) were used, and the researchers relied on the participants’ opinions and awareness in answering the questionnaire. Additionally, in the current research, the average score of awareness and adaptation to the gluten diet was reported as close to the average. According to Casellas et al (21) and Nachman et al (26), the HRQOL is affected by the state of awareness and compliance with a GFD in people. In other words, being aware and having extensive information about the disease cause more adherence to GFD. The results of the present survey match those of a former study that suggested the existence of a relationship between HRQOL and GFD adherence (21).
Gastrointestinal symptoms and adherence to a GFD could predict 17% of the variance in HRQOL. In line with the present results, the findings of the study by Dimidi et al confirmed that there was a statistically significant correlation among the symptoms of CD following a GFD, so that the probability of symptoms increases with decreasing compliance to a GFD. In addition, adaptation to a GFD is consistently and significantly predicted for a better HRQOL in patients (15). The findings are in conformity with those of the study performed by Usai et al (27). The outcome of the regression analysis in the second stage showed that after improving adherence to the GFD, the HRQOL increased, and following a GFD predicted the patients’ HRQOL more strongly. In line with these findings, the results of the study by Lamba et al revealed that HRQOL and health-related physical and mental quality subscales increased after following the GFD (28). The present findings corroborate the results of former surveys (14,29), demonstrating that after one year of following a GFD, the HRQOL of celiac patients improved significantly, and gastrointestinal symptoms alleviated in these patients.
In the present study, the outcome of path analysis using structural equation modeling represented that the path coefficient between CDAT and QOL was significant, and CDAT with the maximum score predicted changes in HRQOL. The GSRS could also predict 27% of changes in HRQOL. The findings of Nikniaz et al (8) confirmed the effect of CDAT and GSRS on the HRQOL of celiac patients. In line with this study, the findings of Möller et al indicated that gastrointestinal symptoms, directly and indirectly, affect the HRQOL through negative perception of the disease, inconsistent coping, catastrophizing of pain, and mental distress. An increase of 50.6% could explain the percentage of changes in HRQOL. Moreover, based on the goodness of fit indices and the results of the present study, the study model showed a good fit (13).
This study had some weaknesses. The completion of the questionnaire was self-reported, and it was performed by sending the link of the questionnaire to the personal page in the social networks of each of the patients. On the other hand, the study had some strengths. During the implementation of this study, in cooperation with the Gastrointestinal and Liver Diseases Research Center of Qom University of Medical Sciences, to improve the QOL of this group of patients, all their medical and demographic information was saved online. Patients with CD were registered, and in this way, we managed to provide financial support packages for the preparation of a GFD.
Conclusion
According to the findings of previous studies, almost all surveys confirmed a positive trace of GFD on the HRQOL of CD patients (30). The results of the current research also emphasized the effect of GFD adherence and gastrointestinal signs on the variance of HRQOL in patients with CD. Following a GFD can play a role in explaining the variance in the HRQOL of celiac patients indirectly and through digestive symptoms. Based on the findings of this study, better adherence to the GFD can lead to a better clinical response and fewer gastrointestinal symptoms, thus enhancing the HRQOL of celiac patients.
Acknowledgments
The authors sincerely appreciate the cooperation of the participating patients in the research.
Authors’ Contribution
Conceptualization: Ehsan Vesali-Monfared, Sarallah Shojaei, Mohammad Reza Ghadir.
Data curation: Ehsan Vesali-Monfared, Abolfazl Mohammadbeigi, Aazam Farahanie.
Formal analysis: Ehsan Vesali-Monfared, Abolfazl Mohammadbeigi.
Funding acquisition: Ehsan Vesali-Monfared, Rahim Aali.
Investigation: Ehsan Vesali-Monfared, Sarallah Shojaei, Mohammad Reza Ghadir.
Methodology: Abolfazl Mohammadbeigi, Ehsan Vesali-Monfared.
Project administration: Ehsan Vesali-Monfared, Mohammad Reza Ghadir.
Resources: Ehsan Vesali-Monfared, Rahim Aali.
Software: Seyed Mohammad Riahi.
Supervision: Ehsan Vesali-Monfared, Aazam Farahanie.
Validation: Ehsan Vesali-Monfared, Rahim Aali, Mohammad Reza Ghadir.
Visualization: Ehsan Vesali-Monfared, Sarallah Shojaei.
Writing–original draft: Ehsan Vesali-Monfared, Abolfazl Mohammadbeigi, Aazam Farahanie, Mohammad Reza Ghadir.
Writing–review & editing: Ehsan Vesali-Monfared, Aazam Farahanie, Mohammad Reza Ghadir.
Competing Interests
The authors declare that there was no conflict of interests.
Ethical Approval
This study was registered at Qom University of Medical Sciences (ethical code IR.MUQ.REC.1402.107). Informed consent was obtained from the participants.
Funding
The current research received financial support from Qom University of Medical Sciences.
References
- Parzanese I, Qehajaj D, Patrinicola F, Aralica M, Chiriva-Internati M, Stifter S. Celiac disease: from pathophysiology to treatment. World J Gastrointest Pathophysiol 2017; 8(2):27-38. doi: 10.4291/wjgp.v8.i2.27 [Crossref] [ Google Scholar]
- Rubio-Tapia A, Hill ID, Kelly CP, Calderwood AH, Murray JA. ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol 2013; 108(5):656-76. doi: 10.1038/ajg.2013.79 [Crossref] [ Google Scholar]
- Gujral N, Freeman HJ, Thomson AB. Celiac disease: prevalence, diagnosis, pathogenesis and treatment. World J Gastroenterol 2012; 18(42):6036-59. doi: 10.3748/wjg.v18.i42.6036 [Crossref] [ Google Scholar]
- Choung RS, Lamba A, Marietta EV, See JA, Larson JJ, King KS. Effect of a gluten-free diet on quality of life in patients with nonclassical versus classical presentations of celiac disease. J Clin Gastroenterol 2020; 54(7):620-5. doi: 10.1097/mcg.0000000000001277 [Crossref] [ Google Scholar]
-
Singh P, Arora A, Strand TA, Leffler DA, Catassi C, Green PH, et al. Global prevalence of celiac disease: systematic review and meta-analysis. Clin Gastroenterol Hepatol 2018;16(6):823-36.e2. doi: 10.1016/j.cgh.2017.06.037.
- Mohammadibakhsh R, Sohrabi R, Salemi M, Taheri Mirghaed M, Behzadifar M. Celiac disease in Iran: a systematic review and meta-analysis. Electron Physician 2017; 9(3):3883-95. doi: 10.19082/3883 [Crossref] [ Google Scholar]
- Barker JM, Liu E. Celiac disease: pathophysiology, clinical manifestations, and associated autoimmune conditions. Adv Pediatr 2008; 55:349-65. doi: 10.1016/j.yapd.2008.07.001 [Crossref] [ Google Scholar]
- Nikniaz Z, Asghari Jafarabadi M, Abbasalizad Farhangi M, Shirmohammadi M, Nikniaz L. Determinants of health-related quality of life in patients with celiac disease: a structural equation modeling. Health Qual Life Outcomes 2021; 19(1):204. doi: 10.1186/s12955-021-01842-5 [Crossref] [ Google Scholar]
- Caio G, Volta U, Sapone A, Leffler DA, De Giorgio R, Catassi C. Celiac disease: a comprehensive current review. BMC Med 2019; 17(1):142. doi: 10.1186/s12916-019-1380-z [Crossref] [ Google Scholar]
- Oza SS, Akbari M, Kelly CP, Hansen J, Theethira T, Tariq S. Socioeconomic risk factors for celiac disease burden and symptoms. J Clin Gastroenterol 2016; 50(4):307-12. doi: 10.1097/mcg.0000000000000366 [Crossref] [ Google Scholar]
- Burger JPW, de Brouwer B, IntHout J, Wahab PJ, Tummers M, Drenth JP. Systematic review with meta-analysis: Dietary adherence influences normalization of health-related quality of life in coeliac disease. Clin Nutr 2017; 36(2):399-406. doi: 10.1016/j.clnu.2016.04.021 [Crossref] [ Google Scholar]
- Oka P, Parr H, Barberio B, Black CJ, Savarino EV, Ford AC. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2020; 5(10):908-17. doi: 10.1016/s2468-1253(20)30217-x [Crossref] [ Google Scholar]
- Möller SP, Apputhurai P, Tye-Din JA, Knowles SR. Quality of life in coeliac disease: relationship between psychosocial processes and quality of life in a sample of 1697 adults living with coeliac disease. J Psychosom Res 2021; 151:110652. doi: 10.1016/j.jpsychores.2021.110652 [Crossref] [ Google Scholar]
- Enaud R, Tetard C, Dupuis R, Laharie D, Lamireau T, Zerbib F. Compliance with gluten free diet is associated with better quality of life in celiac disease. Nutrients 2022; 14(6):1210. doi: 10.3390/nu14061210 [Crossref] [ Google Scholar]
- Dimidi E, Kabir B, Singh J, Ageridou A, Foster C, Ciclitira P. Predictors of adherence to a gluten-free diet in celiac disease: do knowledge, attitudes, experiences, symptoms, and quality of life play a role?. Nutrition 2021; 90:111249. doi: 10.1016/j.nut.2021.111249 [Crossref] [ Google Scholar]
- Deepak C, Berry N, Vaiphei K, Dhaka N, Sinha SK, Kochhar R. Quality of life in celiac disease and the effect of gluten-free diet. JGH Open 2018; 2(4):124-8. doi: 10.1002/jgh3.12056 [Crossref] [ Google Scholar]
- Qasem WA, Roumi AA, Al Mojil K, Sakijha H, AlMughamis N. Awareness of celiac disease among the public in Kuwait: a cross-sectional survey. BMC Res Notes 2023; 16(1):133. doi: 10.1186/s13104-023-06415-x [Crossref] [ Google Scholar]
- Mazaheri M, Khoshouei MS. Comparison between psychometric characteristics of Persian version of the gastrointestinal symptoms rating scale in functional gastrointestinal disorders and normal groups. Govaresh 2012; 17(1):18-24. [ Google Scholar]
- Nikniaz Z, Asghari Jafarabadi M, Ghaffarifar S, Saeedi Z, Akbari Namvar Z, Shirmohammadi M. Psychometric properties of the Persian version of the celiac disease adherence test questionnaire. BMC Gastroenterol 2020; 20(1):247. doi: 10.1186/s12876-020-01396-8 [Crossref] [ Google Scholar]
- Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The Short Form Health Survey (SF-36): translation and validation study of the Iranian version. Qual Life Res 2005; 14(3):875-82. doi: 10.1007/s11136-004-1014-5 [Crossref] [ Google Scholar]
- Casellas F, Rodrigo L, Lucendo AJ, Fernández-Bañares F, Molina-Infante J, Vivas S. Benefit on health-related quality of life of adherence to gluten-free diet in adult patients with celiac disease. Rev Esp Enferm Dig 2015; 107(4):196-201. [ Google Scholar]
- Rajpoot P, Sharma A, Harikrishnan S, Baruah BJ, Ahuja V, Makharia GK. Adherence to gluten-free diet and barriers to adherence in patients with celiac disease. Indian J Gastroenterol 2015; 34(5):380-6. doi: 10.1007/s12664-015-0607-y [Crossref] [ Google Scholar]
- Sainsbury K, Mullan B, Sharpe L. Reduced quality of life in coeliac disease is more strongly associated with depression than gastrointestinal symptoms. J Psychosom Res 2013; 75(2):135-41. doi: 10.1016/j.jpsychores.2013.05.011 [Crossref] [ Google Scholar]
- Barratt SM, Leeds JS, Sanders DS. Quality of life in coeliac disease is determined by perceived degree of difficulty adhering to a gluten-free diet, not the level of dietary adherence ultimately achieved. J Gastrointestin Liver Dis 2011; 20(3):241-5. [ Google Scholar]
- Wolf RL, Lebwohl B, Lee AR, Zybert P, Reilly NR, Cadenhead J. Hypervigilance to a gluten-free diet and decreased quality of life in teenagers and adults with celiac disease. Dig Dis Sci 2018; 63(6):1438-48. doi: 10.1007/s10620-018-4936-4 [Crossref] [ Google Scholar]
- Nachman F, del Campo MP, González A, Corzo L, Vázquez H, Sfoggia C. Long-term deterioration of quality of life in adult patients with celiac disease is associated with treatment noncompliance. Dig Liver Dis 2010; 42(10):685-91. doi: 10.1016/j.dld.2010.03.004 [Crossref] [ Google Scholar]
- Usai P, Manca R, Cuomo R, Lai MA, Boi MF. Effect of gluten-free diet and co-morbidity of irritable bowel syndrome-type symptoms on health-related quality of life in adult coeliac patients. Dig Liver Dis 2007; 39(9):824-8. doi: 10.1016/j.dld.2007.05.017 [Crossref] [ Google Scholar]
- Lamba A, Marietta EV, See JA, Larson JJ, King KS, Van Dyke CT. Effect of a gluten-free diet on quality of life in patients with nonclassical versus classical presentations of celiac disease. J Clin Gastroenterol 2020; 54(7):620-5. doi: 10.1097/mcg.0000000000001277 [Crossref] [ Google Scholar]
- Mustalahti K, Lohiniemi S, Collin P, Vuolteenaho N, Laippala P, Mäki M. Gluten-free diet and quality of life in patients with screen-detected celiac disease. Eff Clin Pract 2002; 5(3):105-13. [ Google Scholar]
- Wagner G, Berger G, Sinnreich U, Grylli V, Schober E, Huber WD. Quality of life in adolescents with treated coeliac disease: influence of compliance and age at diagnosis. J Pediatr Gastroenterol Nutr 2008; 47(5):555-61. doi: 10.1097/MPG.0b013e31817fcb56 [Crossref] [ Google Scholar]