J Educ Community Health. 11(4):230-241.
doi: 10.34172/jech.3333
Review Article
Barriers and Facilitators of Acceptance of Mobile Applications Regarding Health-Related Issues in the Elderly: A Systematic Review
Arman Miri 1  , Somaye Karami 1, Maryam Afshari 2, 3, 4, *
, Somaye Karami 1, Maryam Afshari 2, 3, 4, * 
Author information:
1Student Research Committee, Hamadan University of Medical Sciences, Hamadan, Iran
2Social Determinants of Health Research Center, Institute of Health Sciences and Technologies, Hamadan University of Medical Sciences, Hamadan, Iran
3Research Center for Health Sciences, Institute of Health Sciences and Technologies, Hamadan University of Medical Sciences, Hamadan, Iran
4Department of Public Health, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran
Abstract
Background: As technology swiftly advances, especially with the increased use of smartphones and the internet, mobile health (mHealth) emerges as a valuable tool for reducing health problems and improving healthcare services, particularly for the high-risk elderly population. This systematic review was conducted to identify resources and existing information related to factors that influence the acceptance of health-based mobile applications among the elderly, referring to the social-ecological model.
Methods: Studies were searched until October 2023 through electronic databases, including Web of Science, Scopus, PubMed, and Embase. English language studies that had the elderly as their research population and were conducted cross-sectionally were included in the study. The intended studies were categorized through a framework called the ecological model. The Critical Appraisal Checklist for Cross-Sectional Studies (AXIS) tool was used to assess the quality of the articles. In total, twelve studies met the inclusion criteria and were finally chosen to be part of this analysis.
Results: The results revealed that perceived usefulness and ease of understanding were the most common facilitators, and privacy risk was the most common barrier at the intrapersonal level. At the interpersonal and organizational levels, social influence and facilitating conditions were the most influential factors in the acceptance of these applications in the facilitator section, and technical problems were the most influential in the barriers section. Access to services was an important factor that influenced health-based mobile applications for the elderly at the community level. Eight articles were of high quality using the AXIS tool.
Conclusion: The findings from this review are anticipated to guide health policy implementation centers practically, aiding in creating and executing effective policies to encourage the adoption of health-oriented mobile applications from a broad social-ecological viewpoint.
Keywords: Geriatrics, Mobile health applications, Facilitators, Barriers
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Miri A, Karami S, Afshari M. Barriers and facilitators of acceptance of mobile applications regarding health-related issues in the elderly: a systematic review. Educ Community Health. 2024; 11(4):230-241. doi:10.34172/jech.3333
Introduction
Aging is a phenomenon with various biological, psychological, and social aspects (1). Based on United Nations estimates, the global elderly population was about 200 million in 1950, rose to 350 million by 1975, and is projected to surpass 1.1 billion by 2025, marking a 224% increase (2). This event is one of the most striking achievements in human history in terms of improving health, social, and economic indicators over time. These improvements have contributed to a steady increase in life expectancy worldwide (3). Many studies show that as life expectancy increases, so do the risks of chronic diseases, disabilities, and cognitive decline among older adults (4-6). This predicament predicts increased use and demand for specialized health services among this subpopulation (7,8).
Today, technologically supported healthcare is rapidly advancing and providing new tools for health self-management. While older adults are often found to be slow to adopt new technologies, their internet usage is notably increasing each year (9). A rapid and growing trend of smartphone ownership among the elderly has been reported worldwide (10). With the swift advancement of technology, particularly in the realms of smartphones and internet usage, mobile health (mHealth) emerges as a valuable tool for reducing health issues while enhancing healthcare services. Up to now, there has been no universally accepted definition for mobile health. However, the World Health Organization defines mobile health as the practice of medicine and public health supported by mobile devices, personal digital assistants, and other wireless technologies (11). Over 325 000 mobile health applications have been identified that cover various areas of health, medical, and fitness topics (12,13). There is strong evidence showing that mobile health applications effectively enhance self-care, self-management, medication adherence, and self-efficacy. They also lead to positive health outcomes, such as improved sleep quality, diet, physical activity, and mental health (14-17).
A large body of research has confirmed the benefits of mobile health for the elderly (18-21). Studies have shown that incorporating mobile health technology with healthcare professionals’ recommendations can help the elderly maintain a healthy lifestyle. This includes enhancements in daily food intake, sleep quality, and physical activity (13,14). As a result, elderly individuals, especially those with chronic illnesses, experience better self-management and monitoring of their health. Additional benefits include overcoming barriers to treatment, including long hospital wait times, transportation issues, and rising healthcare costs (19,21).
Notwithstanding the several benefits of mobile health among the elderly, this subpopulation also faces certain obstacles. The literature often points out barriers such as usability issues, sensory decline, and unfamiliarity with technology for the elderly. While studies on mobile health acceptance among the elderly are growing, a few of them have focused solely on mobile apps. Many studies have investigated the integration of mobile health with electronic health, including specialized websites, telehealth sessions, fitness trackers, and other tools (14,15,22-24). In addition, some studies have examined the perceptions of the elderly regarding the use of mobile applications for health-related purposes, including perceived facilitators and barriers (14). Although mobile applications hold significant potential to enhance elderly health, their true effectiveness hinges on the users’ acceptance and continuous usage of these technologies (25).
Bronfenbrenner’s ecological model, created in 1979, shows how systemic structures (family, culture, socio-economic status, politics, and psychology) interact to shape human development and behavior. These interconnected elements influence our behavior, life choices, and overall health throughout our lives (26). The mentioned model outlines how environmental influences, from the individual to broader social systems, shape technology acceptance through intrapersonal, interpersonal, organizational, community, and public policy factors. McLeroy et al offered strategies for each level, aiming to change knowledge and behavior, enhance social networks, improve living environments, modify community services, and create or change public policies (27). This model helps understand factors affecting mobile application acceptance among the elderly (28-30). Nonetheless, to the best of our knowledge, none of the studies have thoroughly explored the factors across all five levels of the ecological model. Thus, this systematic review was undertaken from the ecological model perspective to fill this gap. The aims of this review are (1) to identify and synthesize findings from existing literature on factors affecting the acceptance of health applications among the elderly, structured around the ecological model, and (2) to assess the quality of reviewed studies.
Materials and Methods
Search Databases
In this review, all cross-sectional studies that addressed barriers and facilitators in the acceptance of mobile applications for health-related issues among the elderly were included, regardless of their time range and publication status. All cross-sectional studies that mentioned the study outcome of articles, including barriers and facilitators in the acceptance of mobile applications without any publication year restriction and from all over the world, were examined as well. Major international electronic databases, including PubMed, ISI Web of Science, Embase, and Scopus, were reviewed up to October 2023. In addition, the reference list of the selected study was reviewed to find potentially eligible studies. Research strategies from previous reviews on related topics were used to create a comprehensive list of keywords. These search phrases were categorized into four subject groups, namely, (1) ‘Mobile application’ OR ‘mobile app’ etc., (2) ‘Geriatric OR pensioner’ etc., (3) ‘Barrier’ OR ‘Limitation’ etc., and (4) ‘Cross-Sectional’ OR ‘descriptive-analytical’. The detailed search strategy is outlined in Box 1.
Box 1: Search Strategy
“Mobile application*” OR “mobile app” OR mHealth OR “mobile health” OR Telehealth OR “mobile technology”
AND
Geriatric OR pensioner OR over 60 OR old OR “over sixth” OR older OR elderly OR senior OR “Older adults” OR Elderly OR “Aging population” OR “Older population” OR Aging
AND
Barrier OR Limitation OR Difficulty OR Restriction OR Drawback OR Facilitate OR Motivate OR Promote OR Help OR Ease OR Aid
AND
“Cross–Sectional” OR “descriptive-analytical” OR “Cross Sectional Studies” OR “Cross Sectional” OR “Cross-Sectional Study” OR “Cross Sectional Study” OR “Cross-Sectional Studies” OR “Cross Sectional Analysis” OR “Cross-Sectional Analysis” OR “Cross Sectional Analyses” OR “Cross-Sectional Analyses” OR “Cross-Sectional Survey” OR “Cross Sectional Survey” OR “Prevalence Studies” OR “Prevalence Study”
Data Extraction
In the beginning, one researcher gathered all identified articles from various sources using EndNote software. After merging the articles from all the databases and removing duplicates, two researchers independently reviewed all the articles, excluding those irrelevant to the study subject and entry criteria. The abstracts of the remaining articles were independently assessed by two researchers. Then, the full text of the relevant articles was reviewed, and those fully meeting the entry criteria were identified. Additional articles were included through forward and backward citation reviews. The required data were extracted by two researchers. Any disagreements were resolved through discussion and, if necessary, the opinion of a third researcher. The search results were reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (31) (Figure 1).
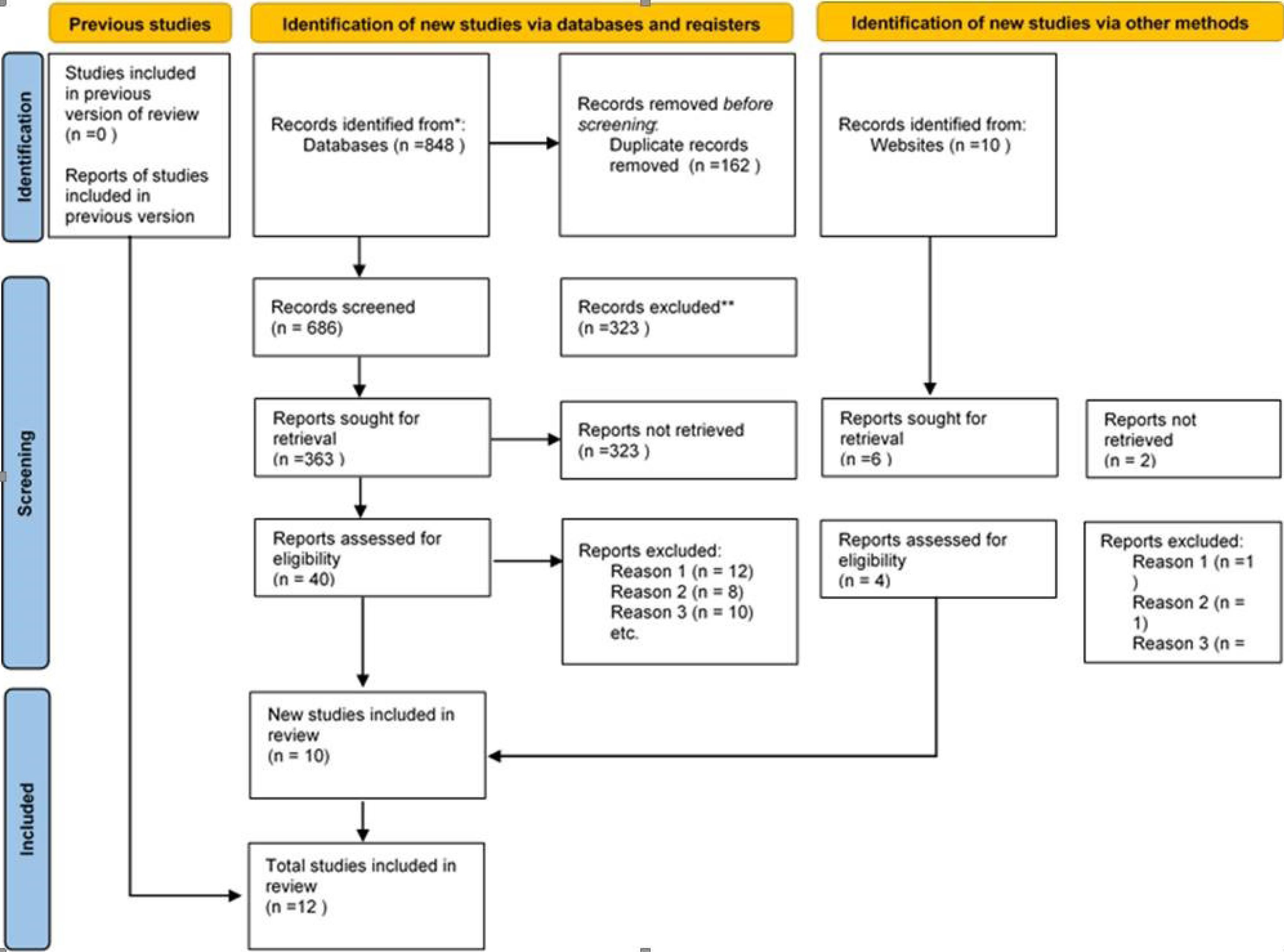
Figure 1.
PRISMA Flow Diagram. Note. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
.
PRISMA Flow Diagram. Note. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Ecological Levels
The Ecological Model of Health Behavior was employed in this research to categorize factors influencing the enactment of protective behaviors (32). The model is structured into individual, interpersonal, organizational, community, and policy and public policy levels. The individual level is associated with an individual’s knowledge, attitudes, and skills. The interpersonal level encompasses interactions and exchanges within a person’s network, including both primary relationships such as family and close friends and larger secondary groups. The organizational level pertains to social institutions that serve as formal authorities and establish public and accepted objectives. The community level involves the relationships that organizations form with one another, often observed in coalitions. Finally, the policy and public policy level is related to policies implemented by local and national governments. The ideal application of this model considers all five levels.
Quality of Studies
The methodological quality of the included articles was independently evaluated by two researchers using the Critical Appraisal Checklist for Cross-Sectional Studies (AXIS). This checklist consists of 20 items focused on methods and reported results, divided into reporting quality, study design quality, and risk of bias categories. Each item is scored as ‘1’ for ‘Yes’ (Y) and ‘0’ for ‘No’ (N) or ‘Don’t Know’ (DK). The total score is calculated as a percentage of all 20 items, with scores above 60% classified as high quality (33,34).
Results
A total of 848 articles were identified in the search process. Additionally, 12 studies were found through manual search. Due to duplication, 162 studies were removed, and 686 studies were screened. In each screening stage of the title and abstract, 323 articles were eliminated. Eventually, out of the remaining 40 articles, 30 studies were removed after full-text review, leaving 10 articles. Of the manually searched articles, two more articles remained, bringing the total number of remaining studies to 12 (Figure 1). Among these articles, four studies were conducted in the Netherlands (31,35-37), three in the United States (38-40),two in China (28,41),one in Iraq (42),one in South Korea (43),and one in Bangladesh (44). All studies were cross-sectional designs according to the study entry criterion. All studies used a self-reported questionnaire method, and the sampling was convenient. The snowball sampling method was used only in one study (31), along with the convenience sampling method (Table 1).
Table 1.
Determinants Related to Elderly Intention of Using mHealth Applications
|
Authors/ Country
|
Journal
|
Sampling
Technique
|
Sample Size
|
Determinants Examined in Studies
|
Theoretical Framework
|
Results
|
|
Demographic
|
Individual Level
|
Interpersonal Level
|
Organizational Level
|
Community Level
|
Public Policy Level
|
| Klaver et al/ Netherlands (36) |
JMIR Mhealth Uhealth |
Convenience Sampling |
N = 481 |
Gender, age, education, general health, prior experience with the internet, and prior experience with mHealth |
Perceived risk, privacy risk, performance risk, legal concern, and trust |
- |
- |
- |
- |
The technology acceptance model (TAM) |
- Benefits: Trust, age, gender, education, and health status
- Barriers: Privacy risk, performance risk, and legal concern |
Kurlander et al/
USA (38) |
Am J Manag Care |
Convenience Sampling |
N = 2,256 |
Gender, age, education, race, and comfort using video chat |
Privacy, vision/hearing difficulties,
and low quality of care |
Lack of personal connection with the doctor |
Technical problems of the programs |
|
|
- |
- Facilitator: Age (65–80 years, gender (male),
-Barriers: Lack of privacy, difficulty seeing/hearing,
low quality of care, lack of feeling of personal connection with the doctor, and technical problems of the programs |
| Lee et al/ South Korea (43) |
PLOS ONE |
Convenience Sampling |
N = 207 |
Gender, age, education, occupational status, monthly household income, and living area |
Confidence using mobile health apps, physical limitations, lack of understanding about mobile health apps, and privacy concerns |
- |
Minimizing time and space constraints of conventional healthcare, cost, and lack of support |
Increasing accessibility to manage health |
- |
Innovation diffusion model |
- Benefits: Self-confidence, minimizing time and space constraints of conventional healthcare, and increasing accessibility to manage health
Barriers: Physical limitations, misunderstanding about the mHealth app, cost and privacy concerns, and lack of support |
van Elburg et al/
Netherlands (30) |
BMC Geriatrics |
Convenience Sampling, snowball sampling |
N = 360 |
Age, gender, education, marital status, and living arrangement |
Perceived usefulness, perceived ease of use, attitude toward use, sense of control, feelings of anxiety, personal innovativeness, social relationship, and self-perceived effectiveness |
Subjective norm |
Facilitating circumstances |
Service availability and finance |
- |
Expanded versions of the TAM |
- Benefits: Perceived usefulness, perceived ease of use, attitude toward use, sense of control, personal innovativeness, social relationship, self-perceived effectiveness, subjective norm, facilitating circumstances, and service availability
Barriers: Feelings of anxiety |
| Askari et al/the Netherlands (37) |
J Med Internet Res |
Convenience Sampling |
N = 364 |
Age, gender, education, marital status, and living arrangement |
Perceived usefulness, perceived ease of use, attitude toward use, sense of control, feelings of anxiety, personal innovativeness, social relationship, and self-perceived effectiveness |
Subjective norm |
Facilitating circumstances |
Service availability and finance |
- |
Senior TAM |
- Benefits: Perceived usefulness, perceived ease of use, attitude toward use, sense of control, personal innovativeness, social relationship, self-perceived effectiveness, subjective norm, facilitating circumstances, and service availability
Barriers: Feelings of anxiety |
Bhatia et al/
USA (39) |
Journal of the
American Geriatrics Society |
Convenience Sampling |
N = 278 |
Age, gender, education, marital status, race, annual household income, Insurance, type of telemedicine, and length of telemedicine visit on average |
Convenience of telemedicine, efforts to help understand your health problems, privacy, duration of appointments, poor quality of care, and lack of technological skills |
Ability to communicate |
Technical problems and video quality |
Access to services |
|
|
Benefits: Convenience of telemedicine, the ability to connect, the effort made to help them understand their health issues, the quality of the video, the privacy, the duration of their visit, and accessibility
Barriers: Less confidence, technical difficulties, lower quality of care, relationship building, and lack of technological skills |
Van Elburg et al/
Netherlands (35) |
Front. Public Health |
Convenience sampling |
N = 816 |
Age, gender, education, marital status, and living arrangement |
Perceived usefulness, perceived ease of use, attitude toward use, sense of control, feelings of anxiety, personal innovativeness, and self-effectiveness, |
Subjective norm and social relationships |
Service availability |
Facilitating circumstances |
|
Adapted TAM |
Benefits: Perceived usefulness, perceived ease of use, attitude toward use, sense of control, personal innovativeness, self-effectiveness, service availability, and facilitating circumstances |
Kalicki et al/
USA (40) |
Journal of the
American Geriatrics Society |
Convenience sampling |
N = 873 |
Age, gender, marital status, race, and language |
Cognitive impairment |
|
Ability to pay for mobile applications |
Access to the phone with the ability to install a video call application |
|
|
Barriers: Cognitive impairment, lack of access to a caregiver to assist them with technology, ability to pay for cellular plans, or video-capable device access |
Palas et al/
Bangladesh (44) |
BMC Medical Informatics and decision-making |
Convenience sampling |
N = 493 |
Age, gender, education, and marital status |
Hedonic motivation, habit, and quality of life |
Social influence |
Value for price |
Quality of services |
|
Adapted TAM |
Facilitator: Hedonic motivation, habit, social influence, price value, and service quality |
Xie
et al/
China (28) |
Proceedings of the 2020 HFES 64th International Annual Meeting |
Convenience sampling |
N = 108 |
Age, gender, education, and monthly income |
Perceived usefulness, perceived ease of use, and
literacy using programs |
Impact of healthcare providers |
Smartphone screen |
Access to high-quality information |
|
Adapted TAM |
Facilitator: Perceived usefulness, perceived ease of use, and
literacy of using health programs and providers
Barriers: Smartphone screen and access to quality information |
Lan
et al/
China (41) |
BIBE2020 |
Convenience sampling |
N = 367 |
Age, gender, education, and monthly income |
Performance expectation, effort expectation, pleasure motivation, habit, trust, individualism, and uncertainty avoidance |
Social influence and the power of distance |
Value for money and facilitating conditions |
The quality of services |
Government policy |
Adapted TAM |
Facilitator: Expectation of performance and expectation of effort |
Sarre et al/
Iraq (42) |
Jim |
Convenience sampling |
N = 69 |
Age and gender |
Perceived benefits, perceived ease of use, and
mental norm |
|
Facilitating conditions |
|
|
Adapted TAM |
Facilitator: Perceived benefits, perceived ease of use,
mental norm, age, and gender (moderating variables) |
Based on the data in Table 1, regarding the five levels of the ecological model, five studies (28,31,35,39,44) focused on four levels, while four articles addressed three ecological levels (37,38,40,43). One article addressed one level (36), one article considered two levels (42), and one article (41)took into account all ecological levels. Our analysis revealed that eleven articles addressed the first four levels of the ecological model, while only one article touched upon the fifth level. Additionally, eight of these articles primarily focusing on the first four levels (28,31,35-37,41,42,44) used the technology acceptance theory, while three studies did not use any theory in their study (38-40). Only one study utilized the innovation diffusion theory to advance its study objectives (43). Among the factors influencing the acceptance of mobile health applications at the demographic level, gender was the most examined variable (31,35,36,38), and in all articles, the acceptance of applications was higher among men than women. Moreover, the level of education in two studies (36,43)and age in one study (38) were among the variables affecting the acceptance of applications, and other demographic variables had no effect.
Table 2 classifies factors that influence the acceptance of mobile health applications in relation to the ecological model (27). Across all levels, there were more facilitators than barriers (25). Four studies (35,41,42,44)only had facilitators who had a significant relationship with acceptance, while for barriers, only one study (40) was in this manner. Further, self-confidence variables in one study were identified as a facilitator (43)but as a barrier in another study (39). In three studies, social relationships were considered a facilitator (creating better relationships) (31,37,44), while in two studies, they were regarded as a barrier (lack of proper communication) (38,39). Furthermore, privacy was perceived as a facilitator (39) in one study but a barrier in three studies (36,38,43). In the section related to facilitator factors, the most factors were access (28,31,35,37,42)and perceived usefulness (31,35,37,39,43), and in the barrier section, they were related to privacy (36,38,43). Ultimately, 23, 3, 4, and 2 facilitator factors were observed at the individual, interpersonal, organizational, and community levels, respectively (a total of 32). Moreover, 10, 1, 3, and 2 barriers were detected at the individual, interpersonal, organizational, and community levels, respectively (a total of 15).
Table 2.
Variables Affecting the Adoption of Mobile Health Programs Based on Ecological Levels
|
Facilitator
|
Barriers
|
|
Individual Level
|
Interpersonal Level
|
Organizational Level
|
Community Level
|
Public Policy Level
|
Individual Level
|
Interpersonal Level
|
Organizational Level
|
Community Level
|
Public Policy Level
|
| Race |
Community relations |
Minimizing the time and place limitations of health care |
Access to services |
- |
Privacy risk |
Feeling of lack of personal connection with the doctor |
Technical problems of the programs |
Access to the phone with the ability to install a video call application |
- |
| Gender |
Impact of healthcare providers |
Facilitating conditions |
The quality of service |
- |
Performance risk |
- |
Lack of support |
Access to high quality information |
- |
| Education level |
Social influence |
Video quality |
- |
- |
Legal concern |
- |
Smartphone screen |
- |
- |
| Self-confidence |
- |
Price value |
- |
- |
Vision/hearing difficulties |
- |
Cost concerns |
- |
- |
| Trust |
- |
- |
- |
- |
Low quality of care |
- |
- |
- |
- |
| Health status |
- |
- |
- |
- |
Lack of understanding of mobile health programs |
- |
- |
- |
- |
| Perceived usefulness |
- |
- |
- |
- |
Feeling anxious |
- |
- |
- |
- |
| Perceived ease of use |
- |
- |
- |
- |
Less confidence |
- |
- |
- |
- |
| Attitude towards use |
- |
- |
- |
- |
Lack of technological skills |
- |
- |
- |
- |
| Sense of control |
- |
- |
- |
- |
Cognitive impairment |
- |
- |
- |
- |
| Personal innovation |
- |
- |
- |
- |
- |
- |
- |
- |
- |
| Perceived self-efficacy |
- |
- |
- |
- |
- |
- |
- |
- |
- |
| Mental norm |
- |
- |
- |
- |
- |
- |
- |
- |
- |
| The convenience of telemedicine |
- |
- |
- |
- |
- |
- |
- |
- |
- |
| Trying to help the elderly understand their health problems |
- |
- |
- |
- |
- |
- |
- |
- |
- |
| Privacy protection |
- |
- |
- |
- |
- |
- |
- |
- |
- |
| The duration of the appointment |
- |
- |
- |
- |
- |
- |
- |
- |
- |
| Internet usage history |
- |
- |
- |
- |
- |
- |
- |
- |
- |
| History of using phone applications |
- |
- |
- |
- |
- |
- |
- |
- |
- |
| Hedonic motivation |
- |
- |
- |
- |
- |
- |
- |
- |
- |
| Habit |
- |
- |
- |
- |
- |
- |
- |
- |
- |
| Literacy using programs |
- |
- |
- |
- |
- |
- |
- |
- |
- |
| Performance expectation |
- |
- |
- |
- |
- |
- |
- |
- |
- |
| Expect value |
- |
- |
- |
- |
- |
- |
- |
- |
- |
The quality and risk of bias of the included studies were assessed using the AXIS. Table 3 presents the results of the quality review of these studies. Four articles (28,38,41,42)received a score lower than 60%, implying that the quality of the articles was low, but the remaining articles were of good quality.
Table 3.
Checking the Quality of Articles
|
Quality Assessment Using the AXIS Tool of Articles Included in This Systematic Review
|
|
Authors (Year)
|
Questions
|
Overall Quality
|
|
Q1
|
Q2
|
Q3
|
Q4
|
Q5
|
Q6
|
Q7
|
Q8
|
Q9
|
Q10
|
Q11
|
Q12
|
Q13
|
Q14
|
Q15
|
Q16
|
Q17
|
Q18
|
Q19
|
Q20
|
| Klaver et al (2021) |
Y |
Y |
Y |
Y |
N |
N |
N |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
N |
Y |
80% |
| Kurlander et al (2021) |
Y |
Y |
N |
Y |
N |
Y |
Y |
N |
N |
Y |
Y |
N |
N |
N |
Y |
N |
N |
Y |
Y |
Y |
50% |
| Lee et al (2020) |
Y |
Y |
N |
Y |
N |
N |
N |
Y |
Y |
Y |
N |
Y |
N |
Y |
Y |
Y |
Y |
Y |
N |
Y |
70% |
| van Elburg et al (2022) |
Y |
Y |
N |
N |
N |
N |
Y |
Y |
Y |
Y |
N |
Y |
N |
Y |
Y |
N |
Y |
Y |
N |
Y |
60% |
| Askari et al (2020) |
Y |
Y |
N |
Y |
Y |
Y |
N |
Y |
Y |
Y |
N |
Y |
N |
N |
Y |
Y |
Y |
Y |
N |
Y |
70% |
| Bhatia et al (2020) |
Y |
Y |
Y |
Y |
Y |
Y |
N |
Y |
Y |
Y |
Y |
Y |
N |
N |
Y |
Y |
Y |
Y |
N |
Y |
80% |
| van Elburg et al (2023) |
Y |
Y |
N |
N |
N |
N |
Y |
Y |
Y |
Y |
N |
Y |
N |
Y |
Y |
N |
Y |
Y |
N |
Y |
60% |
| Kalicki et al (2021) |
Y |
Y |
Y |
Y |
Y |
Y |
N |
Y |
Y |
Y |
N |
Y |
N |
Y |
Y |
Y |
Y |
N |
Y |
N |
75% |
| Palas et al (2022) |
Y |
Y |
Y |
Y |
Y |
Y |
N |
Y |
Y |
Y |
N |
Y |
N |
N |
Y |
Y |
N |
N |
N |
N |
60% |
| Xie et al (2020) |
Y |
Y |
N |
N |
N |
N |
N |
Y |
N |
Y |
Y |
Y |
N |
N |
Y |
Y |
Y |
Y |
N |
Y |
55% |
| Lan et al (2020) |
Y |
Y |
N |
N |
N |
N |
N |
Y |
Y |
Y |
N |
Y |
N |
N |
Y |
Y |
Y |
N |
N |
N |
45% |
| Saare et al (2019) |
Y |
Y |
N |
N |
N |
N |
N |
Y |
N |
Y |
Y |
Y |
N |
N |
Y |
Y |
Y |
Y |
N |
Y |
55% |
Note. Q: Questions; Y: Yes; N: No.
Discussion
This systematic review examined existing studies related to factors that influence the acceptance of mobile health programs among the elderly through the lens of the ecological model created by McLeroy et al (27). Overall, only a few studies (12) met the entry criteria. Only one study (41) evaluated all five levels associated with the levels of the ecological model, which was not related to the acceptance of mobile health programs. According to previous studies, the role of the last level of the ecological model (the policy level) has been highlighted in various areas. For example, in the study by Müller (45), it was found that the acceptance of technology and mobile applications for drivers and people who are more exposed to traffic accidents can be increased through general government policies and reduce these accidents. However, in the field of health and hygiene, countries have spent considerable costs on new technologies to improve the provision of health services, especially among the elderly population (46). However, the goal of these technological advances fails when the technology adopted for the elderly is unacceptable (47). Despite significant achievements in improving life expectancy and health among the elderly, the rate of improvement has not been highly satisfactory, especially in developing countries (48).
In light of the existing gap, Dhagarra et al (49) identified four key areas for policymakers to ensure the acceptance and successful implementation of technology in elderly healthcare services. First, the technology should emphasize its expected benefits for the elderly. Second, service providers should prioritize ease of use and user comfort. Third, trust plays a crucial role in shaping the elderly’s perception of the technology’s usefulness and their willingness to use it. Unlike expected use and ease of use, which can be communicated to the user, trust must be earned over time. The responsibility here lies with governments to build trust among the elderly to provide healthcare services through technology and health-related phone programs. Finally, privacy concerns affect the final acceptance of any technology. Similar to trust, patient privacy concerns should be reduced by executive organizations and the government. The induction of technology in healthcare not only creates value for the elderly but also for the entire social and economic ecosystem. At the community level, the present systematic review also found variables that were more focused on the quality of services and access to these services. Mobile technology offers users the advantage of accessing health information anytime and anywhere, significantly enhancing their efficiency in managing health-related data (50). However, during the review of studies in this systematic review, it was revealed that access to a phone with the ability to install a video call application and access to quality information can also prevent the acceptance of mobile health programs. The major perceived effect of e-health is an improvement in health understanding.
The effects of health application programs on improving the use of health care, such as the impact on care search or improving the ability of the elderly to manage conditions alone, are relatively less common but can have a profound role in the general health of this group (51). This shows that information and communication technologies not only have a great potential for improving the provision of health-related information but also have a significant impact on the general use of health care. However, concerns have been expressed about whether such effects are beneficial or harmful, as controlling the quality of online health sources is a challenge (52). In addition, people are highly different in their health information literacy (53), and this rate is even lower among the elderly than the average population, causing social and health problems (54).Discusses the complexities of accessing health-related services through information and communication technology, highlighting that such access can be both beneficial and problematic. It emphasizes the importance of improving the quality of available health information and enhancing elderly individuals’ ability to critically evaluate it, ensuring that technology adoption encourages engagement rather than discourages it. Additionally, at the organizational level of the ecological model, various facilitators and barriers to technology adoption were identified (55). Among these, certain environmental facilitators play a role in making technology use easier and more effective. A relatively large number of facilitators and barriers were found in the section related to the organizational level of the ecological model. One of these environmental facilitators could facilitate the use of technology (55), so it was among the facilitating factors. Among these factors, external aids in the living environment can be mentioned (56), making the acceptance of mobile health application programs higher.
According to previous studies, the most significant organizational obstacles were associated with cost and the lack of support (57,58). However, in the study by Lee et al (43), only a fifth and a tenth of the participants in the study reported text size or costs as barriers to using health applications, respectively. It seems that these technical or economic barriers have been overcome with improvements in the general environment of information technology. While many devices and services now provide assistive technology and free public Wi-Fi is widely available, users still report needing technical assistance and facing usage challenges. Even when sensory and cost barriers are addressed, about half of the participants in our study, including mobile health app users, felt unsupported in learning how to use these applications. Therefore, health institutions and professionals should consider how to support the elderly in using these apps in society. At the next level of the ecological model (the interpersonal level), social influence was identified as a facilitator, and social relationships were identified as both a facilitator and a barrier. Social influence is defined as the belief of significant others in the individual about the use of a new system (59). Some studies have proven the role of social influence in users’ intention to accept technology (60), use of mobile health-related services (61), use of digital information in health care (30), and an explanation of the acceptance of the elderly from health application services (62). In the study by Chen and Chan (55), the elderly with better social relationships believed that technologies were useful, and they had a greater tendency to use them compared to the elderly with not-so-good social relationships. This may be attributed to the greater support of these elderly from their families and peers and increased opportunities to share their usage experiences with others. These experiences probably have a positive impact on their belief in the usefulness of technology and influence their intention to use such technology.
Previous research also reported that an active lifestyle and participation in social activities may increase the willingness to learn about new things and accept new advancements in technology (63). On the other hand, health-related mobile applications are a barrier for the elderly who prefer in-person visits and care for identifying problems and thorough examination (64). However, in the study by Haleem et al, the elderly wanted telemedicine to remain an option for future visits and minor health issues that do not require a physical examination (65). In the study by Mahajan et al, the elderly were satisfied with health and medical applications due to convenience, easy access, and reduced exposure to infectious diseases (66). Ultimately, the final level of the ecological model (the individual level) had the most facilitator and barrier variables. More or less all the facilitating factors of technology and application acceptance found in this study were related to the intention to use various forms of technology (medical) in other areas, especially for the elderly (55,56,58,67-70). These similarities exist despite differences in the population of people, including individuals from different countries, and have different effect sizes. Moreover, our findings strongly confirmed the three main factors (perceived usefulness, perceived ease, and access) of the technology acceptance model as the main motivators for using medical applications among the elderly (71). This significant finding is noteworthy as the age of these factors dates back to more than 30 years ago, and technology has significantly advanced. Medical applications did not exist at the time of developing this model. It is possible that the elderly population from 1989 simply transferred factors related to their generation to the future; thus, the findings are valid beyond a short-term horizon. Other facilitating factors can be referred to as performance expectancy, effort expectancy, and habit. These results have also been confirmed in previous studies (30,72,73). However, one of the most important individual facilitators was gender. In a study conducted by Faqih in 2022, the impact of gender on the relationship between factors of the technology acceptance model and behavioral intention regarding the use of mobile health applications was specifically examined among the elderly (73).
In this research, several hypotheses were investigated, two of which are noteworthy. (1) “Perceived usefulness” has a greater impact on behavioral intention to adopt mobile health services for men than women, and (2) “perceived ease” has a greater effect on behavioral intention to adopt mobile health services for women than men. Based on the results of the mentioned study, the first hypothesis was not supported, but the second one was confirmed, which is inconsistent with the findings of the study. Firstly, their population does not consist of the elderly. Only 4.6% of their respondents were over 50 years old. Secondly, a large part of the population of this study was made up of participants with relatively high levels of education (65% of participants had a bachelor’s or master’s degree). It can be argued that, given the relatively young and highly educated population, general technical knowledge is expected to be higher. This, in turn, can have a significant impact on both behavioral intention and what is perceived as useful. For example, their second hypothesis can be explained by dividing the social role. Women, when using new technology, instead of performing tasks, attach more importance to ease of use (74). Many variables were identified in terms of barriers at this level of the ecological model. Performance risk states that independent-living elderly who are doubtful whether mobile health applications can meet their health care needs have less inclination to use these applications. This issue further confirms the previously reported findings for the general population and may be more valid for the elderly, as they are likely to be afraid that technologies will replace their healthcare professionals (75). Legal concern is based on the argument that the elderly, who are more concerned about improper law enforcement, have less behavioral inclination to use health-related technologies. This finding contradicts those of previous studies that did not show a statistically significant relationship (76).This lack of relationship can be explained by the fact that in this study, the use of health technologies was more limited among the general population of China in the hospital setting, and legal issues were probably less of a concern for respondents due to specific health laws. It seems that legal and rights concerns about the use of mobile applications in the field of health have received less attention in the scientific literature and form a related area for further research. In addition, a recent study in the Netherlands reported that the acceptance rate of a coronavirus disease 19-tracking app for the elderly was significantly lower than that for younger adults (77). One of their hypotheses for this low acceptance rate was that older people feel they are not adequately protected by a tracking app. The elderly, due to different perceived risk factors, as shown in our study, are not adequately protected, and as a result, have a lower acceptance rate.
This study had some limitations. This systematic review examined cross-sectional studies from the perspective of the ecological model. The model may have certain limitations; for instance, it might not effectively demonstrate the relative importance of different levels and factors. Additionally, other social-ecological models or theories could offer alternative perspectives. Although we created and followed a precise and regular protocol based on the cognitive assumptions related to systematic studies, other studies and reviews that examine studies from other dimensions may have different results. Further, only cross-sectional studies were included in our systematic review; it seems necessary to have other studies that evaluate different types of other studies. Furthermore, the quality assessment using the AXIS tool demonstrated that 4 of the 12 studies were of low quality, indicating that the overall strength of the evidence may be limited.
Conclusion
This study systematically investigated factors influencing the acceptance of mobile health applications among the elderly using an ecological model. It was found that ease of use and perceived usefulness were key predictors of acceptance. In addition, barriers such as privacy concerns and lack of support appeared significant. The study suggests that future interventions should improve services and facilitate conditions to enhance program acceptance. Further, the use of several models may provide more conceptual insight. It also highlights the need for future research to explore effective policies and strategies to improve access to health services, especially for the elderly. The findings are expected to guide decision-making, improve public health, and aid in the development of policies to promote the acceptance of health-based mobile applications.
Authors’ Contributions
Conceptualization: Arman Miri, Maryam Afshari.
Data curation: Arman Miri, Somaye Karami.
Formal analysis: Arman Miri, Somaye Karami, Maryam Afshari.
Investigation: Arman Miri, Somaye Karami, Maryam Afshari.
Methodology: Arman Miri, Maryam Afshari.
Project administration: Maryam Afshari.
Resources: Maryam Afshari.
Supervision: Maryam Afshari.
Original-draft writing: Arman Miri, Maryam Afshari.
Writing–review & editing: Arman Miri, Maryam Afshari.
Competing Interests
None of the authors of this paper had any conflict of interests, including specific financial interests, relationships, or affiliations related to the subject matter or materials included in this manuscript.
Ethical Approval
The study was approved by the Ethics Committee of Hamadan University of Medical Sciences (No. IR.UMSHA.REC.1402.466).
Funding
This work was supported by Hamadan University of Medical Sciences [reference No. 140207045549].
References
- World Health Organization (WHO). WHO Coronavirus (COVID-19). WHO; 2023. Available from: https://covid19.who.int/.
-
Smyer MA, Downs MG. Psychopharmacology: an essential element in educating clinical psychologists for working with older adults. In: Knight BG, Teri L, Wohlford P, Santos J, eds. Mental Health Services for Older Adults: Implications for Training and Practice in Geropsychology. American Psychological Association; 1995. p. 73-83. doi: 10.1037/10184-007.
-
Dhakad M, Saikia N. Regional patterns of adult mortality by sex and place of residence in India. In: Adult Mortality in India: Trends, Socio-economic Disparities and Consequences. Singapore: Springer; 2023. p. 29-44. doi: 10.1007/978-981-99-0002-2_3.
- Brayne C. The elephant in the room - healthy brains in later life, epidemiology and public health. Nat Rev Neurosci 2007; 8(3):233-9. doi: 10.1038/nrn2091 [Crossref] [ Google Scholar]
- Chenery-Morris S. The living end--the future of death, aging and immortality. Nursing Standard 2008; 22(34):30-1. [ Google Scholar]
- Baharin R, Saad S. Ageing population and health care expenditure: evidence using time series analysis. Geografia 2018; 14(4):65-73. doi: 10.17576/geo-2018-1404-06 [Crossref] [ Google Scholar]
- Rowe JW. Chair, Committee on the Future Health Care Workforce for Older Americans Institute of Medicine the National Academies Before the Special Committee on Aging [dissertation]. Mailman School of Public Health; 2008.
- Acharya S, Ghimire S, Jeffers EM, Shrestha N. Health care utilization and health care expenditure of Nepali older adults. Front Public Health 2019; 7:24. doi: 10.3389/fpubh.2019.00024 [Crossref] [ Google Scholar]
- Yang S, Jang JW. Understanding older adults’ internet use and psychological benefits: the moderating role of digital skills. Behav Inf Technol 2024; 43(1):60-71. doi: 10.1080/0144929x.2022.2153082 [Crossref] [ Google Scholar]
- Estacio EV, Whittle R, Protheroe J. The digital divide: examining socio-demographic factors associated with health literacy, access and use of internet to seek health information. J Health Psychol 2019; 24(12):1668-75. doi: 10.1177/1359105317695429 [Crossref] [ Google Scholar]
- Ryu S. Book review: mHealth: new horizons for health through mobile technologies: based on the findings of the second global survey on eHealth (global observatory for eHealth series, volume 3). Healthc Inform Res 2012; 18(3):231-3. doi: 10.4258/hir.2012.18.3.231 [Crossref] [ Google Scholar]
- West JH, Hall PC, Hanson CL, Barnes MD, Giraud-Carrier C, Barrett J. There’s an app for that: content analysis of paid health and fitness apps. J Med Internet Res 2012; 14(3):e72. doi: 10.2196/jmir.1977 [Crossref] [ Google Scholar]
- Heart T, Kalderon E. Older adults: are they ready to adopt health-related ICT?. Int J Med Inform 2013; 82(11):e209-31. doi: 10.1016/j.ijmedinf.2011.03.002 [Crossref] [ Google Scholar]
- Changizi M, Kaveh MH. Effectiveness of the mHealth technology in improvement of healthy behaviors in an elderly population-a systematic review. Mhealth 2017; 3:51. doi: 10.21037/mhealth.2017.08.06 [Crossref] [ Google Scholar]
- Thiruvanackan K, Mohd Yusof M. Evaluation of mobile health application (mHealth) from the pharmacist perspective. Journal of Information System and Technology Management 2017; 2(6):31-54. [ Google Scholar]
- Nasir S, Goto R, Kitamura A, Alafeef S, Ballout G, Hababeh M. Dissemination and implementation of the e-MCHHandbook, UNRWA’s newly released maternal and child health mobile application: a cross-sectional study. BMJ Open 2020; 10(3):e034885. doi: 10.1136/bmjopen-2019-034885 [Crossref] [ Google Scholar]
- Barber T, Sharif B, Teare S, Miller J, Shewchuk B, Green LA. Qualitative study to elicit patients’ and primary care physicians’ perspectives on the use of a self-management mobile health application for knee osteoarthritis. BMJ Open 2019; 9(1):e024016. doi: 10.1136/bmjopen-2018-024016 [Crossref] [ Google Scholar]
- Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health 2013; 38(5):976-93. doi: 10.1007/s10900-013-9681-1 [Crossref] [ Google Scholar]
- Agyemang-Duah W, Peprah C, Peprah P. Barriers to formal healthcare utilisation among poor older people under the livelihood empowerment against poverty programme in the Atwima Nwabiagya district of Ghana. BMC Public Health 2019; 19(1):1185. doi: 10.1186/s12889-019-7437-2 [Crossref] [ Google Scholar]
- Doetsch J, Pilot E, Santana P, Krafft T. Potential barriers in healthcare access of the elderly population influenced by the economic crisis and the troika agreement: a qualitative case study in Lisbon, Portugal. Int J Equity Health 2017; 16(1):184. doi: 10.1186/s12939-017-0679-7 [Crossref] [ Google Scholar]
- Chang AY, Skirbekk VF, Tyrovolas S, Kassebaum NJ, Dieleman JL. Measuring population ageing: an analysis of the Global Burden of Disease Study 2017. Lancet Public Health 2019; 4(3):e159-67. doi: 10.1016/s2468-2667(19)30019-2 [Crossref] [ Google Scholar]
- Alley S, van Uffelen JG, Schoeppe S, Parkinson L, Hunt S, Power D. Efficacy of a computer-tailored web-based physical activity intervention using Fitbits for older adults: a randomised controlled trial protocol. BMJ Open 2019; 9(12):e033305. doi: 10.1136/bmjopen-2019-033305 [Crossref] [ Google Scholar]
- Salim MH, Ali NM, Mohd Noah SA. Mobile application on healthy diet for elderly based on persuasive design. Int J Adv Sci Eng Inf Technol 2017; 7(1):222-7. doi: 10.18517/ijaseit.7.1.1725 [Crossref] [ Google Scholar]
- Vanoh D, Shahar S, Razali R, Ali NM, Abdul Manaf Z, Mohd Noah SA. The effectiveness of a web-based health education tool, WESIHAT 20, among older adults: a randomized controlled trial. J Alzheimers Dis 2019; 70(s1):S255-S70. doi: 10.3233/jad-180464 [Crossref] [ Google Scholar]
- Zhao J, Freeman B, Li M. Can mobile phone apps influence people’s health behavior change? An evidence review. J Med Internet Res 2016; 18(11):e287. doi: 10.2196/jmir.5692 [Crossref] [ Google Scholar]
- Bronfenbrenner U. Ecological models of human development. International Encyclopedia of Education 1994; 3(2):37-43. [ Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q 1988; 15(4):351-77. doi: 10.1177/109019818801500401 [Crossref] [ Google Scholar]
- Xie Z, Or CK. Acceptance of mHealth by elderly adults: a path analysis. Proc Hum Factors Ergon Soc Annu Meet 2020; 64(1):755-9. doi: 10.1177/1071181320641174 [Crossref] [ Google Scholar]
- Hoque R, Sorwar G. Understanding factors influencing the adoption of mHealth by the elderly: an extension of the UTAUT model. Int J Med Inform 2017; 101:75-84. doi: 10.1016/j.ijmedinf.2017.02.002 [Crossref] [ Google Scholar]
- van Elburg FR, Klaver NS, Nieboer AP, Askari M. Gender differences regarding intention to use mHealth applications in the Dutch elderly population: a cross-sectional study. BMC Geriatr 2022; 22(1):449. doi: 10.1186/s12877-022-03130-3 [Crossref] [ Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151(4):264-9. doi: 10.7326/0003-4819-151-4-200908180-00135 [Crossref] [ Google Scholar]
- Sallis JF, Owen N, Fisher E. Ecological models of health behavior. In: Health Behavior: Theory, Research, and Practice. Jossey-Bass; 2008.
- Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open 2016; 6(12):e011458. doi: 10.1136/bmjopen-2016-011458 [Crossref] [ Google Scholar]
- Veenhof C, Huisman PA, Barten JA, Takken T, Pisters MF. Factors associated with physical activity in patients with osteoarthritis of the hip or knee: a systematic review. Osteoarthritis Cartilage 2012; 20(1):6-12. doi: 10.1016/j.joca.2011.10.006 [Crossref] [ Google Scholar]
- van Elburg FR, van de Klundert J, Nieboer AP, Askari M. The intention to use mHealth applications among Dutch older adults prior and during the COVID pandemic. Front Public Health 2023; 11:1130570. doi: 10.3389/fpubh.2023.1130570 [Crossref] [ Google Scholar]
- Klaver NS, van de Klundert J, van den Broek R, Askari M. Relationship between perceived risks of using mHealth applications and the intention to use them among older adults in the Netherlands: cross-sectional study. JMIR Mhealth Uhealth 2021; 9(8):e26845. doi: 10.2196/26845 [Crossref] [ Google Scholar]
- Askari M, Klaver NS, van Gestel TJ, van de Klundert J. Intention to use medical apps among older adults in the Netherlands: cross-sectional study. J Med Internet Res 2020; 22(9):e18080. doi: 10.2196/18080 [Crossref] [ Google Scholar]
- Kurlander JE, Kullgren JT, Adams MA, Malani PN, Kirch M, Solway E. Interest in and concerns about telehealth among adults aged 50 to 80 years. Am J Manag Care 2021; 27(10):415-22. doi: 10.37765/ajmc.2021.88759 [Crossref] [ Google Scholar]
- Bhatia R, Gilliam E, Aliberti G, Pinheiro A, Karamourtopoulos M, Davis RB. Older adults’ perspectives on primary care telemedicine during the COVID-19 pandemic. J Am Geriatr Soc 2022; 70(12):3480-92. doi: 10.1111/jgs.18035 [Crossref] [ Google Scholar]
- Kalicki AV, Moody KA, Franzosa E, Gliatto PM, Ornstein KA. Barriers to telehealth access among homebound older adults. J Am Geriatr Soc 2021; 69(9):2404-11. doi: 10.1111/jgs.17163 [Crossref] [ Google Scholar]
-
Lan Z, Liu H, Yang C, Liu X, Sorwar G. Investigating influencing factors of Chinese elderly users’ intention to adopt mHealth based on the UTAUT2 model. In: Proceedings of the Fourth International Conference on Biological Information and Biomedical Engineering. New York, NY: Association for Computing Machinery; 2020. p. 1-5. doi: 10.1145/3403782.3403798.
- Saare MA, Hussain A, Yue WS. Conceptualizing mobile health application use intention and adoption among Iraqian older adults: from the perspective of expanded technology acceptance model. Int J Interact Mob Technol 2019; 13(10):28-41. doi: 10.3991/ijim.v13i10.11285 [Crossref] [ Google Scholar]
- Lee M, Kang D, Yoon J, Shim S, Kim IR, Oh D. The difference in knowledge and attitudes of using mobile health applications between actual user and non-user among adults aged 50 and older. PLoS One 2020; 15(10):e0241350. doi: 10.1371/journal.pone.0241350 [Crossref] [ Google Scholar]
- Palas JU, Sorwar G, Hoque MR, Sivabalan A. Factors influencing the elderly’s adoption of mHealth: an empirical study using extended UTAUT2 model. BMC Med Inform Decis Mak 2022; 22(1):191. doi: 10.1186/s12911-022-01917-3 [Crossref] [ Google Scholar]
- Müller JM. Comparing technology acceptance for autonomous vehicles, battery electric vehicles, and car sharing—a study across Europe, China, and North America. Sustainability 2019; 11(16):4333. doi: 10.3390/su11164333 [Crossref] [ Google Scholar]
- Almalki ZS, Simsim DA. The role of health technology in transforming healthcare delivery and enhancing spending efficiency. Global Journal of Medical Therapeutics 2020; 2(3):11-5. doi: 10.46982/gjmt.2020.107 [Crossref] [ Google Scholar]
- Fitzgerald M, Kruschwitz N, Bonnet D, Welch M. Embracing digital technology: a new strategic imperative. MIT Sloan Manag Rev 2014; 55(2):1. [ Google Scholar]
- Foreman KJ, Marquez N, Dolgert A, Fukutaki K, Fullman N, McGaughey M. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet 2018; 392(10159):2052-90. doi: 10.1016/s0140-6736(18)31694-5 [Crossref] [ Google Scholar]
- Dhagarra D, Goswami M, Kumar G. Impact of trust and privacy concerns on technology acceptance in healthcare: an Indian perspective. Int J Med Inform 2020; 141:104164. doi: 10.1016/j.ijmedinf.2020.104164 [Crossref] [ Google Scholar]
- Wu IL, Li JY, Fu CY. The adoption of mobile healthcare by hospital’s professionals: an integrative perspective. Decis Support Syst 2011; 51(3):587-96. doi: 10.1016/j.dss.2011.03.003 [Crossref] [ Google Scholar]
- Baker L, Wagner TH, Singer S, Bundorf MK. Use of the internet and e-mail for health care information: results from a national survey. JAMA 2003; 289(18):2400-6. doi: 10.1001/jama.289.18.2400 [Crossref] [ Google Scholar]
- Fiksdal AS, Kumbamu A, Jadhav AS, Cocos C, Nelsen LA, Pathak J. Evaluating the process of online health information searching: a qualitative approach to exploring consumer perspectives. J Med Internet Res 2014; 16(10):e224. doi: 10.2196/jmir.3341 [Crossref] [ Google Scholar]
- Tonsaker T, Bartlett G, Trpkov C. Health information on the internet: gold mine or minefield?. Can Fam Physician 2014; 60(5):407-8. [ Google Scholar]
- Akhtyan AG, Anikeeva OA, Sizikova VV, Shimanovskaya YV, Starovoitova LI, Medvedeva GP. Information literacy of older people: social aspects of the problem. Int J Civ Eng Technol 2018; 9(11):1789-99. [ Google Scholar]
- Chen K, Chan AH. Gerontechnology acceptance by elderly Hong Kong Chinese: a senior technology acceptance model (STAM). Ergonomics 2014; 57(5):635-52. doi: 10.1080/00140139.2014.895855 [Crossref] [ Google Scholar]
- Ryu MH, Kim S, Lee E. Understanding the factors affecting online elderly user’s participation in video UCC services. Comput Human Behav 2009; 25(3):619-32. doi: 10.1016/j.chb.2008.08.013 [Crossref] [ Google Scholar]
- Wildenbos GA, Peute L, Jaspers M. Aging barriers influencing mobile health usability for older adults: a literature-based framework (MOLD-US). Int J Med Inform 2018; 114:66-75. doi: 10.1016/j.ijmedinf.2018.03.012 [Crossref] [ Google Scholar]
- Cajita MI, Hodgson NA, Lam KW, Yoo S, Han HR. Facilitators of and barriers to mHealth adoption in older adults with heart failure. Comput Inform Nurs 2018; 36(8):376-82. doi: 10.1097/cin.0000000000000442 [Crossref] [ Google Scholar]
- Wills MJ, El-Gayar OF, Bennett D. Examining healthcare professionals’ acceptance of electronic medical records using UTAUT. Issues in Information Systems 2008; 9(2):396-401. doi: 10.48009/2_iis_2008_396-401 [Crossref] [ Google Scholar]
- Nisha N, Iqbal M, Rifat A, Idrish S. Exploring the role of service quality and knowledge for mobile health services. International Journal of E-Business Research (IJEBR) 2016; 12(2):45-64. doi: 10.4018/ijebr.2016040104 [Crossref] [ Google Scholar]
-
Yin M, Li Q, Qiao Z. A study on consumer acceptance of online pharmacies in China. In: Proceedings of the 18th Annual International Conference on Electronic Commerce: E-Commerce in Smart Connected World. New York, NY: Association for Computing Machinery; 2016. p. 1-8. doi: 10.1145/2971603.2971616.
- Bhattacherjee A, Hikmet N. Reconceptualizing organizational support and its effect on information technology usage: evidence from the health care sector. J Comput Inf Syst 2008; 48(4):69-76. doi: 10.1080/08874417.2008.11646036 [Crossref] [ Google Scholar]
- Werner JM, Carlson M, Jordan-Marsh M, Clark F. Predictors of computer use in community-dwelling, ethnically diverse older adults. Hum Factors 2011; 53(5):431-47. doi: 10.1177/0018720811420840 [Crossref] [ Google Scholar]
- Li KY, Marquis LB, Malani PN, Solway E, Kirch M, Singer D. Perceptions of telehealth among older US adults during the COVID-19 pandemic: a national survey. J Telemed Telecare 2025; 31(1):55-63. doi: 10.1177/1357633x231166031 [Crossref] [ Google Scholar]
- Haleem A, Javaid M, Singh RP, Suman R. Telemedicine for healthcare: capabilities, features, barriers, and applications. Sens Int 2021; 2:100117. doi: 10.1016/j.sintl.2021.100117 [Crossref] [ Google Scholar]
- Mahajan V, Singh T, Azad C. Using telemedicine during the COVID-19 pandemic. Indian Pediatr 2020; 57(7):658-61. doi: 10.1007/s13312-020-1895-6 [Crossref] [ Google Scholar]
- van Velsen L, Evers M, Bara CD, Op den Akker H, Boerema S, Hermens H. Understanding the acceptance of an eHealth technology in the early stages of development: an end-user walkthrough approach and two case studies. JMIR Form Res 2018; 2(1):e10474. doi: 10.2196/10474 [Crossref] [ Google Scholar]
- Hendrikx HC, Pippel S, van de Wetering R, Batenburg RS. Expectations and attitudes in eHealth: a survey among patients of Dutch private healthcare organizations. Int J Healthc Manag 2013; 6(4):263-8. doi: 10.1179/2047971913Y.0000000050 [Crossref] [ Google Scholar]
-
Renaud K, van Biljon J. Predicting technology acceptance and adoption by the elderly: a qualitative study. In: Proceedings of the 2008 Annual Research Conference of the South African Institute of Computer Scientists and Information Technologists on IT Research in Developing Countries: Riding the Wave of Technology. New York, NY: Association for Computing Machinery; 2008. p. 210-9. doi: 10.1145/1456659.1456684.
-
van Biljon J, Renaud K. A qualitative study of the applicability of technology acceptance models to senior mobile phone users. In: Advances in Conceptual Modeling–Challenges and Opportunities. Berlin, Heidelberg: Springer; 2008. doi: 10.1007/978-3-540-87991-6_28.
- Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q 1989; 13(3):319-40. doi: 10.2307/249008 [Crossref] [ Google Scholar]
- Quaosar G, Hoque MR, Bao Y. Investigating factors affecting elderly’s intention to use m-Health services: an empirical study. Telemed J E Health 2018; 24(4):309-14. doi: 10.1089/tmj.2017.0111 [Crossref] [ Google Scholar]
- Faqih KMS. Investigating the adoption of an innovation using an Extended UTAUT Model: the case of mobile learning technology. Journal of Theoretical and Applied Information Technology 2022; 100(17):5600-31. [ Google Scholar]
- Zhang J. Exploring drivers in the adoption of mobile commerce in China. J Am Acad Bus 2009; 15(1):64-9. [ Google Scholar]
- Apolinário-Hagen J, Hennemann S, Fritsche L, Drüge M, Breil B. Determinant factors of public acceptance of stress management apps: survey study. JMIR Ment Health 2019; 6(11):e15373. doi: 10.2196/15373 [Crossref] [ Google Scholar]
- Deng Z, Hong Z, Ren C, Zhang W, Xiang F. What predicts patients’ adoption intention toward mHealth services in China: empirical study. JMIR Mhealth Uhealth 2018; 6(8):e172. doi: 10.2196/mhealth.9316 [Crossref] [ Google Scholar]
- Jonker M, de Bekker-Grob E, Veldwijk J, Goossens L, Bour S, Rutten-Van Mölken M. COVID-19 contact tracing apps: predicted uptake in the Netherlands based on a discrete choice experiment. JMIR Mhealth Uhealth 2020; 8(10):e20741. doi: 10.2196/20741 [Crossref] [ Google Scholar]