J Educ Community Health. 9(4):221-227.
doi: 10.34172/jech.2022.1852
Original Article
Effects of Educational Intervention on Promoting Preventive Behaviors of Cardiovascular Disease Using the Health Belief Model in Oil Regions Workers
Sahar Mohammadnabizadeh 1, *  , Ali Asghar Najafpoor 2, Mohammad Vahedian-Shahroodi 3, 1, Vahid Ghavami 4, 1
, Ali Asghar Najafpoor 2, Mohammad Vahedian-Shahroodi 3, 1, Vahid Ghavami 4, 1
Author information:
1Social Determinants of Health Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
2Department of Environmental Health Engineering, School of Health, Mashhad University of Medical Sciences, Mashhad, Iran
3Department of Health Education and Health Promotion, School of Health, Mashhad University of Medical Sciences, Mashhad, Iran
4Department of Biostatistics, School of Health, Mashhad University of Medical Sciences, Mashhad, Iran
Abstract
Background: Research conducted on oil region workers has shown that numerous ranges of physical stressors together with behavioral patterns can affect the enhancement of cardiovascular disease (CVD). The aim of this study was to investigate the effects of educational intervention to promote the preventive behaviors of CVD using the Health Belief Model (HBM).
Methods: The participant of this quasi-experimental study included 228 workers (114 control and 114 experimental cases) working in oil regions. Data were collected through questionnaires containing demographic information, knowledge, and constructs of HBM. The experimental group received an education with WhatsApp. Workers completed the questionnaires before and after the education and the 3-month follow-up. Data were analyzed using SPSS 24.0.
Results: The t test analyses showed no significant differences between the control and experimental groups at baseline. The results indicated the changes in outcome variables across time for groups. Except for perceived severity and perceived barriers, there were significant interaction effects between the time and group. A significant correlation was found between behavior and health belief subscales and knowledge, except for perceived severity and cues to action.
Conclusion: The findings of this research confirmed the usefulness of the educational intervention based on the HBM and the necessity to apply designed programs to improve preventive behavior adoption. Preventive education with attention to decreasing unhealthy lifestyles must be designed based on the requirements and target group characteristics to prevent CVD risks.
Keywords: Health Belief Model, Educational intervention, Cardiovascular disease
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Mohammadnabizadeh S, Najafpoor AA, Vahedian-Shahroodi M, Ghavami V. Effects of educational intervention on promoting preventive behaviors of cardiovascular disease using the health belief model in oil regions workers. J Educ Community Health. 2022; 9(4):221-227. doi:10.34172/jech.2022.1852
Introduction
Cardiovascular diseases (CVDs) are the most main cause of individuals’ premature mortalities all over the world (1). Some CVD-related risk factors such as age, ethnicity, and family history cannot be changed, while the other parameters can be changed or prevented, including physical inactivity, tobacco exposure, unhealthy diets, high cholesterol, and high blood pressure (2). Behavioral (modifiable) risk factors caused more then 90% CVDs could be decreased through primary prevention (3). According to published reports, more than 48% of people’s mortalities around the world have been caused by CVDs (4). In Iran, CVDs are also known as the main cause of mortality accounting for approximately 39.3% of deaths (5).
Lately, workers’ diseases have been a significant subject of investigation (6). Although there is a wide range of research in this area, there are still gaps in the awareness required to increase efficient workers’ involvement in their health (6). In Iran, a significant part of the manpower of the national Iranian oil regions is dedicated to shift works. In these types of work, workers often work 14 days in a row, daily 12 hours, and then 14 days off in remote areas (7). These types of work have received little attention in the literature although wide-spreading (1). Numerous ranges of physical stressors such as poor air quality, noise, extreme temperatures, and hazardous chemicals, together with behavioral patterns, could contribute to the enhancement of CVD risk factors (8). Studies demonstrated that heart attack is the main reason for death within oil industries (1,9).
In this regard, it is required to monitor the health conditions of workers in order to encourage healthy behaviors. Interventions based on appropriate theories can enhance the effectiveness of behavioral education by indicating which factors influence a behavior (10). The Health Belief Model (HBM) is one of the preventative behavioral theories used to examine individuals’ motivation for performing and adopting a health-related behavior (11). HBM confirms how an individual’s belief in fear of health problems and attitude, as well as the evaluation of barriers and benefits of preventive behaviors, can lead to specific healthy behavior (12). HBM contributes to multiple health promotion behaviors such as decreasing risk in CVD patients, stopping smoking, breast self-examination, and CVD prevention occurrence (13,14).
Based on our knowledge, unfortunately, no significant study has been conducted in the regions of recognizing CVDs and educational interventions among workers under shift work schedules in oil areas. This research aimed to promote the preventive behaviors of CVDs applying HBM among oil region workers.
Materials and Methods
This research is a quasi-experimental investigation. Participants were onshore workers under a shift work schedule (14 days in a row, daily 12 hours, and then 14 days off) in the oil regions in Ahvaz province, southern Iran. Data were collected between September 2021 and January 2022. Two sites were randomly selected from the oil regions. Overall, 228 workers (114 control and 114 experimental cases) were chosen via simple random sampling using the list of workers with software (Figure 1). After receiving ethical approval from Mashhad University of Medical Sciences, the research purpose was described for workers, and consent was also collected from all of them. The criteria of investigation included affirming consent to take part in the research and not being diagnosed with CVDs. The exclusion criteria consisted of incomplete questionnaire answers and participation reluctance in research.
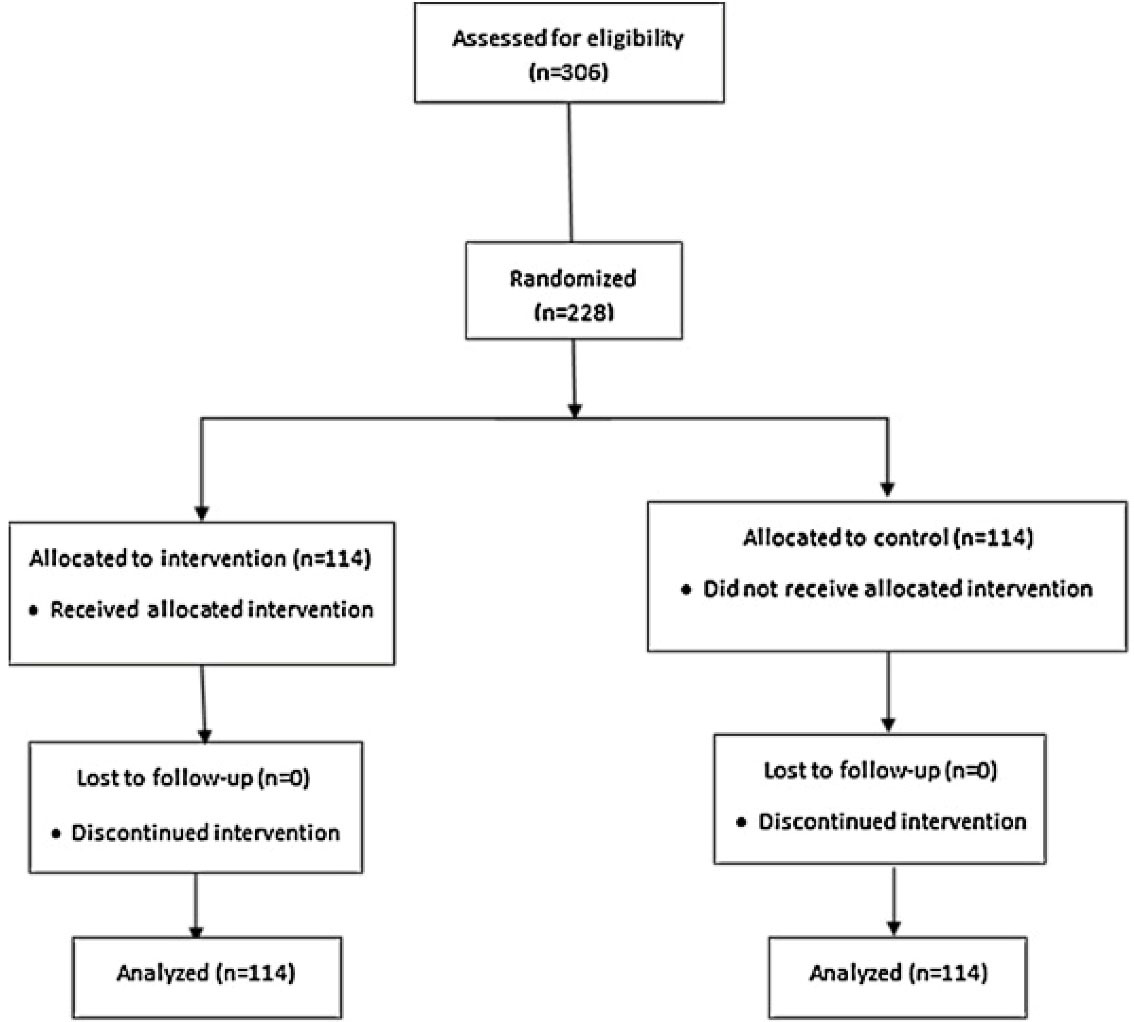
Figure 1.
Protocol of the Intervention Investigation
.
Protocol of the Intervention Investigation
Data collection tools were questionnaires that included demographic characteristics, a knowledge questionnaire, an HBM-based questionnaire, and a prevention behaviors questionnaire.
Demographic information was collected through questionnaires, including age, marital status, and education.
The HBM questionnaire, which was made by Sharifzadeh et al, was used to examine the model structures, and its validity was affirmed by them (5). The test-retest reliability examination showed that it was stable over 2 weeks in 30 workers. HBM subscales were also studied, including perceived susceptibility (4 items, Intraclass correlation coefficient [ICC] = 0.80, Cronbach’s alpha = 0.86), perceived severity (n = 6, ICC = 0.84, Cronbach’s alpha = 0.91), perceived benefits (n = 7, ICC = 0.89, Cronbach’s alpha = 0.92), perceived barriers (n = 6, ICC = 0.80, Cronbach’s alpha = 0.91), self-efficacy (n = 6, ICC = 0.70, Cronbach’s alpha = 0.90), and cues to action (n = 5, ICC = 0.68, Cronbach’s alpha = 0.91). To score the items, a 5-point Likert-type scale was used, ranging from strongly disagree (score 1) to strongly agree (score 5), except for perceived barriers that were scored reversely (1 = Strongly agree to 5 = Strongly agree). Five questions of preventive behaviors against CVDs were about appropriate diet (low calorie, fat, and salt, and daily consumption of fruits and vegetables), exercise three times a week for 30 minutes, blood pressure, cholesterol and sugar control, and smoking refrainment (5). The ICC and Cronbach’s alpha for this scale were 0.71 and 0.92, respectively. Further, a 5-point Likert-type scale ranging from never (score 1) to always (score 5) was employed to score the items. Moreover, the items of cardiac-related health knowledge consisted of 38 questions assessed by “I do not know”, “Yes”, and “No” templates (5). Workers completed the questionnaires before and after the education and 3-month follow-up.
The experimental group received education with WhatsApp. A group was formed in WhatsApp for information exchange and forward educational messages (15) via text, figure, video, and voice messages for 4 weeks (Table 1). In the WhatsApp group, workers could interact with each other or professionals by asking questions and making suggestions. Furthermore, as a reminder, messages related to educational matters were available to research participants in the mentioned group.
Table 1.
Components of Intervention, Objectives, and Methods
|
Sessions
|
Objectives
|
A Summary of Topics and Activities
|
Educational Time (min)
|
| 1 |
Knowledge |
-Familiarizing with cardiac problems’ definitions
-Familiarizing with CVD risk factors
-Familiarizing with healthy and unhealthy behaviors |
First week (60) |
| 2 |
Perceived threat (perceived severity and susceptibility) |
- Enhancing workers’ perception of the threat of doing unhealthy behaviors focused on control of CVD risk
-Reporting the CVDs statistics in Iran and around the world
- Describing the negative outcomes of unhealthy behaviors affecting CVDs
-Describing the unhealthy behaviors of those at high risk for CVDs
- Highlighting the critically and seriousness of threat situations such as heavy expenses of treatment |
Second week (60) |
| 3 |
Perceived benefits and barriers |
-Identifying and emphasizing prevention strategies focused on doing proper exercises (exercising at least 30 minutes a day, three times a week), healthy dietary such as eating at least five daily servings of vegetables and fruits and diet of low fat, sugar and salt, checking blood pressure, cholesterol, and sugar, weight control, cessation of smoking, and management of stress
-Describing the effects of prevention behaviors such as feeling better, living longer, being stronger, family would advantage, tension relieve, losing weight, and the like
-Identifying barriers and resolving methods |
Third week (60) |
| 4 |
Self-efficacy |
- Increasing workers’ capability to overcome obstacles in order to carry out healthy behaviors
-Explaining how to break down healthy behaviors into small activities in order to engaged in them more easily
-Sharing experiences of workers who had successfully overcome healthy lifestyle barriers
-Highlighting the effects of carrying out prevention behaviors |
Forth week (60) |
Note. CVD: Cardiovascular disease.
Analysis
Data were analyzed using SPSS 24.0. Changes in outcome variables from baseline through post-intervention and follow-up were measured by a two-way repeated measure ANOVA to demonstrate differences between groups. Mauchly’s test could determine the Greenhouse-Geisser assumptions met for variables. Further, the analysis of Pearson correlation was employed to assess the correlation between preventive behaviors and HBM constructs.
Results
Table 2 presents demographic characteristics. The age range of workers was 25-57. The t-test analysis showed there were no significant differences between the experimental and control groups at baseline (Table 3). The results indicated changes in outcome variables across time for the group. Except for perceived severity and perceived barriers, significant interaction effects were observed between times and groups for the constructs of perceived susceptibility, perceived benefits, self-efficacy, cues to action, knowledge, and behavior.
Table 2.
Worker’s Baseline Characteristics
|
Demographic Characteristics
|
Intervention
|
Control
|
P
Value
|
| Age (year), mean (SD) |
40.60 (5.37) |
40.03 (6.16) |
0.45 |
| Education, No. (%) |
| Diploma |
9 (7.9) |
13 (11.4) |
0.27 |
| Associate degree |
24 (21.1) |
28 (24.6) |
| Bachelor science |
54 (47.4) |
49 (43) |
| Master science |
27 (23.7) |
24 (21.1) |
| Marital status, No. (%) |
| Married |
66 (57.9) |
62 (54.4) |
0.59 |
| Single |
48 (42.1) |
52 (45.6) |
Note. SD: Standard deviation.
Table 3.
Changes in Outcome Variables During Baseline Through Follow-up
|
Variable
|
Time
|
Intervention (n=114)
|
Control (n=114)
|
Groups (
P
Value)
|
Group×Time (
P
Value)
|
| Perceived severity |
Pretest |
1.53 (0.38)aA |
1.50 (0.41)aA |
0.59 |
0.25 |
| Posttest |
1.56 (0.41)aA |
1.51 (0.40)aA |
0.34 |
| Follow-up |
1.59 (0.39)bA |
1.53 (0.38)aA |
0.26 |
| Perceived susceptibility |
Pretest |
1.41 (0.51)aA |
1.39 (0.49)aA |
0.34 |
0.001 |
| Posttest |
1.74 (0.55)bA |
1.40 (0.49)aB |
0.001 |
| Follow-up |
1.78 (0.54)cA |
1.41 (0.48)aB |
0.001 |
| Perceived benefit |
Pretest |
2.44 (0.44)aA |
2.38 (0.45)aA |
0.30 |
0.001 |
| Posttest |
2.56 (0.45)bA |
2.37 (0.43)aB |
0.001 |
| Follow-up |
2.58 (0.45)cA |
2.38 (0.43)aB |
0.001 |
| Perceived barrier |
Pretest |
3.73 (0.24)aA |
3.68 (0.29)aA |
0.08 |
0.06 |
| Posttest |
3.70 (0.50)bA |
3.67 (0.28)aA |
0.66 |
| Follow-up |
3.60 (0.37)cA |
3.66 (0.28)aB |
0.002 |
| Self-efficacy |
Pretest |
2.23 (0.29)aA |
2.22 (0.30)aA |
0.95 |
0.001 |
| Posttest |
2.36 (0.37)bA |
2.24 (0.31)aB |
0.01 |
| Follow-up |
2.38 (0.37)bA |
2.24 (0.32)aB |
0.01 |
| Knowledge |
Pretest |
0.38 (0.14)aA |
0.37 (0.17)aA |
0.57 |
0.001 |
| Posttest |
0.44 (0.13)bA |
0.38 (0.17)aB |
0.002 |
| Follow-up |
0.46 (0.13)cA |
0.39 (0.18)aB |
0.001 |
| Cues to action |
Pretest |
2.08 (0.40)aA |
2.08 (0.41)aA |
0.36 |
0.001 |
| Posttest |
2.24 (0.47)bA |
2.09 (0.42)aB |
0.01 |
| Follow-up |
2.25 (0.47)cA |
2.09 (0.41)aB |
0.02 |
| Behavior |
Pretest |
2.18 (0.39)aA |
2.15 (0.39)aA |
0.61 |
0.001 |
| Posttest |
2.22 (0.49)aA |
2.16 (0.40)aA |
0.36 |
| Follow-up |
2.30 (0.45)bA |
2.17 (0.40)aB |
0.001 |
Note. ANOVA: Analysis of variance.
a,b,c Means with the same letter in each column (different times) are not significantly different according to ANOVA test (P < 0.05); A,B Means with the same letter in row (different groups) for each variable are not significantly different according to 𝑡 test (P < 0.05).
Finally, a statistical correlation was detected between health belief subscales, knowledge, and behavior except for perceived severity and cues to action (Table 4).
Table 4.
Correlation Matrix Among Knowledge, HBM Constructs and Preventive Behaviors
|
Variables
|
Behavior
|
Perceived Barrier
|
Perceived Benefit
|
Self-efficacy
|
Perceived Severity
|
Perceived Susceptibility
|
Cues to Action
|
Knowledge
|
| Behavior |
1 |
-0.279** |
0.146* |
0.355** |
0.113 |
0.236** |
0.120 |
0.329** |
| Perceived barrier |
-0.279** |
1 |
0.009 |
-0.002 |
-0.023 |
-0.092 |
-0.154* |
-0.192** |
| Perceived benefit |
0.146* |
0.009 |
1 |
0.221** |
-0.026 |
0.194** |
0.119 |
0.023 |
| Self-efficacy |
0.355** |
-0.002 |
0.221** |
1 |
0.168* |
0.216** |
0.245** |
0.218** |
| Perceived severity |
0.113 |
-0.023 |
-0.026 |
0.168* |
1 |
0.050 |
0.039 |
0.211** |
| Perceived susceptibility |
0.236** |
-0.092 |
0.194** |
0.216** |
0.050 |
1 |
0.232** |
0.093 |
| Cues to action |
0.120 |
-0.154* |
0.119 |
0.245** |
0.039 |
0.232** |
1 |
0.033 |
| knowledge |
0.329** |
-0.192** |
0.023 |
0.218** |
0.211** |
0.093 |
0.033 |
1 |
Note. HBM: Health belief model; ** Correlation is significant at the 0.01 level (2-tailed); * Correlation is significant at the 0.05 level (2-tailed).
Discussion
Lifestyle plays a significant role in CVD development (16). Theory-based interventions such as HBM help health educators to recognize and suggest solutions to barriers that disappoint individuals to do CVD preventive behaviors (17). In our study, HBM-based intervention improved the mean scores of HBM constructs and knowledge in the experimental group and caused them to better perform preventive behaviors. Except for perceived severity and perceived barriers, there were significant interaction effects between times and groups for perceived susceptibility, perceived benefits, self-efficacy, cues to action, knowledge, and behavior.
The previous investigations revealed that individuals did not have enough knowledge and hence had a poor performance against CVD risk factors (18). For example, Jalali et al reported that 65.3% of people in Babol had a low awareness of CVD risk factors. (19) In this study, the knowledge of workers significantly increased after intervention in the experimental group, which is consistent with the results of Tavassoli et al representing that HBM-based intervention could increase the knowledge of CVD preventive behavior (20) Based on the result of this research and that of Sharifzadeh et al (5) regarding a positive correlation between behavior and knowledge, the implementation of educational intervention and knowledge-raising programs can be highly effective in behavior change. Furthermore, one study confirmed that more awareness of risk factors persuades more people to take action for CVD prevention (21). Contrary to the findings of Chatripour et al represented that the HBM-based education did not increase the mean score of knowledge among teachers for CVD prevention (22). Smalley et al found that the majority of college students had enough knowledge and correctly recognized the risk factors of CVD, but they still engaged in high-risk behaviors (23). Therefore, improving knowledge alone is not enough to improve health behaviors, and other factors that can affect preventive behaviors should be considered, along with knowledge.
Levels of workers’perceived susceptibility were low before intervention (mean score 1.41 for the experimental group) and 1.39 (the control group, out of 5.0), implying that workers of this study did not feel susceptible to CVDs. In addition, increased perceived susceptibility was detected in the experimental group after intervention and follow-up, showing the probable effect of education on workers’ behavior. This result is consistent with the findings of a study in the USA, indicating low perceived susceptibility as a cause for patients not attending to their health (24). In contrast, the findings of the research by Chatripour et al revealed that HBM-based education did not increase the mean score of perceived susceptibility among teachers for CVD prevention (22). The disagreement between the results of our investigation and those of other studies could be due to the discrepancy in the study samples, the interval of data collection, study region, type of educational intervention, and the term of education. Moreover, perceived susceptibility was positively correlated with behaviors. Based on the HBM, when individuals believe and understand threatening conditions, they will be more possible to perform behaviors to prevent them from happening (25).
The mean score on the levels of perceived severity was 1.53 (the experimental group) and 1.50 (the control group) out of 5 before the intervention, demonstrating that oil region workers were not that much worried about CVD severity. In our study, the perceived severity of the experimental group was significantly increased at the follow-up. In the study of Saffari et al based on the HBM to modify the risk factors of CVDs, perceived severity improved between the baseline and follow-up (26). Considering these findings, beliefs of perceived severity are necessary in order to make our workers involve in health-promoting behaviors. Conversely, the findings of Chatripour et al revealed that the HBM-based education did not increase the mean score of perceived severity among teachers for CVD prevention (22). However, since the perceived severity structure had generally no significant interaction effects between times and group, more important variables that are more strength predictors of behavior, including self-efficacy, should be more considered in educational programs.
The mean score of perceived benefits was 2.44 and 2.38 out of 5.0 in the experimental and control groups before the intervention, respectively, which means that workers’ perception of the benefits of preventive behaviors against CVDs was closer to the mean. The findings of Babaei-Sis et al confirmed that the theory-based intervention was effective in improving perceived benefits in individuals susceptible to CVDs (27). Moreover, the results demonstrated a significant correlation between preventive behaviors and perceived benefits. The possibility of performing healthy behaviors will increase when individuals have a higher perception of their benefits.
The mean score of perceived barriers was the highest among all the subscales (3.73 and 3.68 out of 5, respectively, in the experimental and control groups before the intervention. Based on our findings, the perceived barrier was decreased significantly after the intervention in the experimental group. Perceived barriers had a significant role in disease prevention among patients who had experienced infarction as well. In this study, time and facility to exercise, changes in dietary patterns in shift work, and lack of healthy foods at the workplace were found to be major barriers. In contrast, Babaei-Sis et al found that after HBM-based intervention, the mean scores of perceived barriers increased in the test group (27). Ghasemi Amraei et al also reported a lack of a considerable effect on perceived barriers among nurses (28). The reason for this difference in the results can be the difference in the method of education, the duration of the study, and the target group. The inverse correlation between behavior and perceived barriers obtained in this study represents that when workers have more behavioral obstacles, they less adopt preventive behaviors of CVDs. The results of Mahalik and Burns demonstrated that people implicated healthier behaviors when they believed there were benefits to cardiac-related healthy behaviors and understand fewer barriers to performing prevented behaviors (29). Therefore, it is probable to increase health behaviors adoption by reducing obstacles.
In this investigation, increased workers’ self-efficacy was detected in the experimental group, highlighting the possible influence of education on workers’ behavior. Additionally, the results demonstrated a positive correlation between behaviors and self-efficacy, indicating that most workers believed that they could make necessary CVD-preventive behaviors when they had a greater chance. If people believe that the new behaviors are effective, and think that they are able to do them, they will probably attempt the new behaviors are higher. Numerous previous investigations about self-efficacy reported similar results (16). In contrast, Babaei-Sis et al showed that after the HBM-based intervention, the mean scores of self-efficacy had not significantly increased in the experimental group (27). The disagreement between the results of our study and those of others could be the discrepancy in the study samples, interval of data collection, study region, type of educational intervention, and the term of education.
Based on our finding, the cues to action subscale was significantly increased after interventions in the experimental group. Physicians’ information, healthy lifestyle coverage via media, society leaders’ messages, information cultural, and family and social support were all reported as cues to action, which had an important role as information sources to perform health behaviors (30). In studies by Khani Jeihooni et al (31) and Rahimi et al (32), educational programs increased the scores of cues to action. However, in the study by Saffari et al, education according to HBM to improve CVDs risk factors did not have a significant effect on the cues to action structure after intervention (26).
Although no significant changes in behavior were observed in the experimental group between the pretest and posttest, the levels of behavior remained higher at the follow-up than post-intervention. The reason for this may be that participants in the 3-month follow-up period attempted to further increase their ability to perform protective and preventive behaviors against CVD due to educational interventions. These types of interventions can be useful for improving people’s ability to recognize barriers and possible solutions and are successful in attaining and maintaining objectives. Mohammadi et al concluded that after the HBM-based intervention, the mean scores of CVD preventive behaviors had increased in the test group (33). In another study, HBM-based education improved the police officers’ CVD behavior (26).
Performing a theory-based intervention for oil region workers, who are at risk of CVDs, was one of the benefits of this research. Based on the mentioned studies on CVD preventive behaviors, research on such behaviors among high-risk populations should receive the necessary attention. In addition, knowledge was applied to the main HBM constructs in this study. Attention to research among oil workers under a shift work schedule without enough related knowledge and high exposure to CVD risk factors is another strength of the present study.
Some recommendations should be suggested while considering the results of this study. Given the measures of exercise, stress, blood glucose, lipid, blood pressure profile, and pattern of dietary, along with behavioral factors, can prepare a better concept of the education impact in future research. Furthermore, we just followed the workers for 3 months after the education; thus, long-term follow-ups can present different findings.
Limitations
This study had some limitations. This investigation relied on a self-report HBM questionnaire, which introduces the probability of biased results such as recall bias. Further, considering that the present study was conducted at the time of the corona epidemic, to comply with health protocols and prevent disease transmission, the education were conducted in absentia and through WhatsApp; perhaps face-to-face training could have a greater impact on the results of promoting preventive behaviors.
Conclusion
The findings of this research confirmed the usefulness of the educational intervention based on HBM and the necessity to apply designed programs to improve CVD preventive behavior adoption. The HBM-based intervention improved the mean scores of HBM constructs and knowledge in the experimental group and could better persuade this group to perform preventive behaviors. Preventive education with attention to decreasing unhealthy lifestyles must be designed based on the requirements and the target group characteristics to prevent the CVD risks.
Acknowledgements
The authors gratefully acknowledge the financial support of the Social Determinants of Health Research Center, Mashhad University of Medical Sciences, Mashhad, Iran, and the Research Chancellor of Mashhad University of Medical Sciences.
Author Contributions
Conceptualization: Sahar Mohammadnabizadeh, Mohammad Vahedian-Shahroodi.
Data curation: Sahar Mohammadnabizadeh.
Formal Analysis: Sahar Mohammadnabizadeh, Vahid Ghavami.
Investigation: Sahar Mohammadnabizadeh, Ali Asghar Najafpoor, Mohammad Vahedian-Shahroodi.
Methodology: Sahar Mohammadnabizadeh, Vahid Ghavami.
Project administration: Sahar Mohammadnabizadeh, Mohammad Vahedian-Shahroodi.
Software: Sahar Mohammadnabizadeh, Vahid Ghavami.
Supervision: Sahar Mohammadnabizadeh, Ali Asghar Najafpoor, Mohammad Vahedian-Shahroodi.
Validation: Sahar Mohammadnabizadeh, Ali Asghar Najafpoor.
Visualization: Sahar Mohammadnabizadeh, Mohammad Vahedian-Shahroodi.
Writing – original draft: Sahar Mohammadnabizadeh.
Writing – review & editing: Sahar Mohammadnabizadeh.
Conflict of Interests
The authors declare that they have no competing interests.
Ethical Permissions
The study was approved by the Ethics Board of Mashhad University of Medical Sciences (Number IR.MUMS.REC.1400.110).
Funding/Support
The authors received no funding for this project.
References
- Mannocci A, Pignalosa S, Saulle R, Sernia S, De Sanctis S, Consentino M. Prevalence of major cardiovascular risk factors among oil and gas and energy company workers. Ann Ist Super Sanita 2015; 51(2):148-53. doi: 10.4415/ann_15_02_13 [Crossref] [ Google Scholar]
- Gordon T, Kannel WB. Multiple risk functions for predicting coronary heart disease: the concept, accuracy, and application. Am Heart J 1982; 103(6):1031-9. doi: 10.1016/0002-8703(82)90567-1 [Crossref] [ Google Scholar]
- Jorvand R, Haeri Mehrizi AA, Sadeghirad K, Gholami OA, Ansarian Z, Ghofranipour F. Risk factors for cardiovascular diseases among employees of Ilam University of Medical Sciences. Health Educ Health Promot 2018; 6(4):143-7. doi: 10.29252/hehp.6.4.143 [Crossref] [ Google Scholar]
- Azizi F, Hatami H, Janghorbani M. Epidemiology and Control of Common Diseases in Iran. Tehran: Eshtiagh Publications; 2000. p. 602-16.
- Sharifzadeh G, Moodi M, Mazhari Majd H, Musaee I. Application of health belief model in predicting preventive behaviors against cardiovascular disease in individuals at risk. J Health Sci Technol 2017; 1(2):64-9. [ Google Scholar]
- Vianna LCR, Ferreira AP, de Vasconcellos LCF, Bonfatti RJ, de Oliveira MHB. Occupational Health Surveillance: a study in the light of Ministerial Directive nº 3120/98. Saúde Debate 2017; 41(114):786-800. doi: 10.1590/0103-1104201711409 [Crossref] [ Google Scholar]
- Sadeghniiat-Haghighi K, Mehrabinejad MM, Hajighaderi A, Najafi A, Rahimi-Golkhandan A, Zahabi A. Shift work disorder, Insomnia, and depression among offshore oil rig workers. Iran J Psychiatry 2021; 16(2):162-7. doi: 10.18502/ijps.v16i2.5817 [Crossref] [ Google Scholar]
- Parkes KR. Demographic and lifestyle predictors of body mass index among offshore oil industry workers: cross-sectional and longitudinal findings. Occup Med (Lond) 2003; 53(3):213-21. doi: 10.1093/occmed/kqg037 [Crossref] [ Google Scholar]
- Tsai SP, Wendt JK, Ahmed FS, Donnelly RP, Strawmyer TR. Illness absence patterns among employees in a petrochemical facility: impact of selected health risk factors. J Occup Environ Med 2005; 47(8):838-46. doi: 10.1097/01.jom.0000169091.28589.8a [Crossref] [ Google Scholar]
- Mohammad Nabizadeh S, Taymoori P, Hazhir MS, Shirazi M, Roshani D. Educational intervention based on protection motivation theory to improve vitamin E and C consumption among Iranian factory workers. J Clin Diagn Res 2018; 12(10):1-6. doi: 10.7860/jcdr/2018/37056.12079 [Crossref] [ Google Scholar]
- Coe AB, Gatewood SB, Moczygemba LR, Goode JV, Beckner JO. The use of the health belief model to assess predictors of intent to receive the novel (2009) H1N1 influenza vaccine. Innov Pharm 2012; 3(2):1-11. doi: 10.24926/iip.v3i2.257 [Crossref] [ Google Scholar]
- Abood DA, Black DR, Feral D. Nutrition education worksite intervention for university staff: application of the health belief model. J Nutr Educ Behav 2003; 35(5):260-7. doi: 10.1016/s1499-4046(06)60057-2 [Crossref] [ Google Scholar]
- Mirzaei H, Shojaeizadeh D, Tol A, Ghasemi Ghale Ghasemi S, Shirzad M. Application of health belief model (HBM) to promote preventive behaviors against iron-deficiency anemia among female students of high school Fereydan city: a quasi-experimental study. Iran J Health Educ Health Promot 2017; 5(4):260-9. doi: 10.30699/acadpub.ijhehp.5.4.260.[Persian] [Crossref] [ Google Scholar]
- Tavakoli HR, Dini-Talatappeh H, Rahmati-Najarkolaei F, Gholami Fesharaki M. Efficacy of HBM-based dietary education intervention on knowledge, attitude, and behavior in medical students. Iran Red Crescent Med J 2016; 18(11):e23584. doi: 10.5812/ircmj.23584 [Crossref] [ Google Scholar]
- Javadi H. Prevention of Cardiovascular Diseases. Qazvin University of Medical Sciences: Hadith Today; 2004. p. 100.
- Baghianimoghadam MH, Mirzaei M, Rahimdel T. Role of health beliefs in preventive behaviors of individuals at risk of cardiovascular diseases. J Health Syst Res 2013;8(7):1151-8. [Persian].
- Mohammad Nabizadeh S, Taymoori P, Shahmoradi B, Shirazi M. Mediators of behavior change in intervention on vitamins E and C consumption based on protection motivation theory. J Biochem Technol 2018; 9(2):83-9. [ Google Scholar]
- Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L. Health consequences of obesity. Arch Dis Child 2003; 88(9):748-52. doi: 10.1136/adc.88.9.748 [Crossref] [ Google Scholar]
- Jalali SF, Ghassemzadeh M, Mouodi S, Javanian M, Akbari Kani M, Ghadimi R. Epidemiologic comparison of the first and second waves of coronavirus disease in Babol, North of Iran. Caspian J Intern Med 2020; 11(Suppl 1):544-50. doi: 10.22088/cjim.11.0.544 [Crossref] [ Google Scholar]
- Tavassoli E, Hasanzadeh A, Ghiasvand R, Tol A, Shojaezadeh D. Effect of health education based on the health belief model on improving nutritional behavior aiming at preventing cardiovascular disease among housewives in Isfahan. Journal of School of Public Health & Institute of Public Health Research 2010;8(3):11-23. [Persian].
- Mosca L, Mochari H, Christian A, Berra K, Taubert K, Mills T. National study of women’s awareness, preventive action, and barriers to cardiovascular health. Circulation 2006; 113(4):525-34. doi: 10.1161/circulationaha.105.588103 [Crossref] [ Google Scholar]
- Chatripour R, Shojaeizadeh D, Tol A, Sayehmiri K, Asfeia A, Kia F. The impact of teacher education on promoting knowledge, attitude and performance of students in prevention of cardiovascular diseases: application of the HBM model. Razi J Med Sci 2016;23(146):26-35. [Persian].
- Smalley SE, Wittler RR, Oliverson RH. Adolescent assessment of cardiovascular heart disease risk factor attitudes and habits. J Adolesc Health 2004; 35(5):374-9. doi: 10.1016/j.jadohealth.2004.01.005 [Crossref] [ Google Scholar]
- Graziani C, Rosenthal MP, Diamond JJ. Diabetes education program use and patient-perceived barriers to attendance. Fam Med 1999; 31(5):358-63. [ Google Scholar]
- Idyan Z, Thato R. Determinants of preventive behaviors for coronary artery disease among adults in Aceh province, Indonesia. J Health Res 2017; 31(2):109-17. doi: 10.14456/jhr.2017.14 [Crossref] [ Google Scholar]
- Saffari M, Sanaeinasab H, Jafarzadeh H, Sepandi M, O’Garo KN, Koenig HG. Educational intervention based on the health belief model to modify risk factors of cardiovascular disease in police officers in Iran: a quasi-experimental study. J Prev Med Public Health 2020; 53(4):275-84. doi: 10.3961/jpmph.20.095 [Crossref] [ Google Scholar]
- Babaei-Sis M, Ranjbaran S, Mahmoodi H, Babazadeh T, Moradi F, Mirzaeian K. The effect of educational intervention of life style modification on blood pressure control in patients with hypertension. J Educ Community Health 2016; 3(1):12-9. doi: 10.21859/jech-03012 [Crossref] [ Google Scholar]
- Ghasemi Amraei S, Malekshahi F, Goudarzi F, Ebrahimzadeh F. Using an educational program based on health belief model to improve the preventive behaviors of nurses against cardiovascular diseases. J Educ Health Promot 2020; 9:100. doi: 10.4103/jehp.jehp_620_19 [Crossref] [ Google Scholar]
- Mahalik JR, Burns SM. Predicting health behaviors in young men that put them at risk for heart disease. Psychol Men Masc 2011; 12(1):1-12. doi: 10.1037/a0021416 [Crossref] [ Google Scholar]
- Gany FM, Gill PP, Ahmed A, Acharya S, Leng J. “Every disease…man can get can start in this cab”: focus groups to identify south Asian taxi drivers’ knowledge, attitudes and beliefs about cardiovascular disease and its risks. J Immigr Minor Health 2013; 15(5):986-92. doi: 10.1007/s10903-012-9682-7 [Crossref] [ Google Scholar]
- Khani Jeihooni A, Askari A, Kashfi SM, Khiyali Z, Kashfi SH, Safari O. Application of health belief model in prevention of osteoporosis among primary school girl students. Int J Pediatr 2017; 5(11):6017-29. doi: 10.22038/ijp.2017.25144.2130 [Crossref] [ Google Scholar]
- Rahimi T, Shojaei S, Mousavi Miyandashti Z, Amini Z, Khazir Z. Promotion of preventive behaviors of cardiovascular diseases using health belief model in women referring to health centers in Qom, Iran. Qom Univ Med Sci J 2017;10(12):35-44. [Persian].
- Mohammadi N, Soltani N, Amini R, Tapak L. The effect of education based on health belief model on preventive behaviors towards cardiovascular disease. Sci J Hamadan Nurs Midwifery Fac 2018;26(4):227-36. [Persian].