J Educ Community Health. 11(2):75-82.
doi: 10.34172/jech.2162
Original Article
The Effect of Health Belief Model-Based Educational Intervention on Colorectal Cancer Screening among Men Aged 50-70 years
Naser Honaramouz Rodi 1  , Mostafa Nasirzadeh 2
, Mostafa Nasirzadeh 2  , Ali Mehdipour 3
, Ali Mehdipour 3  , Mohammad Asadpour 4, *
, Mohammad Asadpour 4, * 
Author information:
1Department of Health Education and Health Promotion, School of Health, Student Research Committee, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
2Department of Health Education and Health Promotion, School of Health, Occupational Safety and Health Research Center, NICICO, World Safety Organization and Rafsanjan University of Medical Sciences, Rafsanjan, Iran
3Department of Radiology and Medical Physics, Faculty of Paramedicine, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
4Department of Health Education and Health Promotion, School of Health, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
Abstract
Background: One of the most prevalent and lethal cancers worldwide is colorectal cancer. Considering its impact on people’s lives, this study aimed to evaluate the effect of educational intervention (EI) based on the health belief model (HBM) on encouraging men aged 50-70 years in Sangan to undergo colorectal cancer screening (CRCS).
Methods: In this randomized educational trial, two health centers of Sangan were randomly assigned to the control and intervention groups. Then, 53 people from each health center were selected using simple random sampling method. A questionnaire was used as the data collection tool. Therefore, the intervention group received EI based on HBM in four 60-minute training sessions (TSs) in 3 groups of 15-20 people by different teaching methods. Additionally, the practical steps of doing the fecal immunochemical test (FIT) were taught in these sessions. One month after the EI, data were analyzed using SPSS version 18.0.
Results: Before the intervention, there was no significant difference in the constructs of the HBM between the groups (P>0.05), except for the perceived barriers (P=0.009). However, one month after the EI, there were significant differences in the constructs between the groups (P<0.05).
Conclusion: It seems that the EI based on HBM has positive impacts on encouraging people to do FIT for CRC prevention.
Keywords: Intervention, Colorectal cancer, Health Belief Model, Screening
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Honaramouz Rodi N, Nasirzadeh M, Mehdipour A, Asadpour M.The effect of health belief model-based educational intervention on colorectal cancer screening among men aged 50-70 years. J Educ Community Health. 2024; 11(2):75-82. doi:10.34172/jech.2162
Introduction
In 2020, around 10 million deaths (one in six deaths) occurred worldwide due to cancer (1). Colorectal cancer (CRC) is the third most common cancer worldwide (2) and is a major public health problem (3), indicating that an estimated 1.36 million people are affected annually (4). Remarkably, the prevalence of CRC has generally increased in recent decades, and its global burden is expected to rise to more than 2.2 million by 2030 (2). In 2018, Asia had the highest incidence (51.8%) and mortality (52.4%) rates of CRC cases per 100 000 population and disease burden worldwide (3). The incidence of CRC in developing countries as well as Iran is continuously increasing (5). A study reported an age-standardized incidence rate of 8.16 and 6.17 (per 100 000) for CRC in Iranian men and women, respectively (3). These epidemiological changes of CRC in Asia and its growing prevalence can be attributed to lifestyle risk factors such as extreme alcohol consumption, inactive lifestyle, obesity, diabetes, smoking, western lifestyle, increasing population aging, and high consumption of red and processed meat, and so on (6).
Up to 70% of CRC cases can be prevented through lifestyle modification and extensive screening (7). Implementing effective preventive measures against CRC growth, especially among the elderly, is crucial to help control its growing prevalence worldwide. Colorectal cancer screening strategies (CRCS) such as colonoscopy and fecal occult blood testing (FOBT) are effective in preventing CRC and reducing mortality due to early recognition, thus increasing the probability of cancer treatment (2). Routine use of FOBT reduced the risk of death from CRC by 32% (8). Based on the epidemiological data, the incidence and mortality rates of CRC are increasing among people aged 50 years or older. Accordingly, the recommended age range for CRC screening is 50-75 years. Early identification and treatment of CRC have positive effects on reducing the incidence, morbidity, and mortality rates of CRC (3).
Nikbakht et al reported that at least 25.5% of cases were immunochemical fecal occult blood test (IFOBT)-positive, and among them, three cases of cancer were diagnosed. The results of this study will play an important role in developing a CRCS program in the country (9). The results of the study conducted by Hassanlouei et al showed that out of 2.6 million people who participated in the screening program in 2018 and 2019, 3299 (3.09%) and 33583 (2.57%) people had positive results. In 2018, the lowest rate of positive FIT results was observed in Bushehr province (0.59%) and the highest rate was observed in Isfahan city (7.35%) (5). The FOBT detects hemoglobin by immunochemical antibody-based assay fecal immunochemical test (FIT) to human globin, or by guaiac colorimetry to blood. Nowadays, FIT is widely used worldwide (10). In numerous studies, the rate of participation in CRCS by FOBT/FIT has remained low for a variety of reasons such as financial problems, limited service accessibility, screening-induced discomfort, embarrassment, fear, time restrictions, lack of information, fear of cancer diagnosis, low risk perception, inadequate health literacy, social norms, negative attitudes towards screening, key religious, cultural, and gender barriers, lack of medical advice, and lack of prioritization of time for testing (11,12). Thus, it is necessary to identify barriers to screening, motivate people to adhere to primary screening, and identify potential factors that effectively increase the performance of FOBT (13). Despite substantial evidence that CRCS is effective in reducing disease-related mortality, but the screening rate is not acceptable (14). Previous theoretical interventions have been implemented with the aim of increasing the rate of CRCS (11,13). Health education theories have an important role in promoting health, providing information about risk factors, and promoting behavior change (15). Theory-based educational interventions (EIs) can be used to empower and encourage people to perform FOBT (13). The health belief model (HBM) is used to predict the behavior of screening and has been applied as a model for educational programs. The HBM provides an explanation for why people do not participate in health service programs by assessing people’s beliefs and perceptions. HBM constructs are listed in Figure 1 (16).
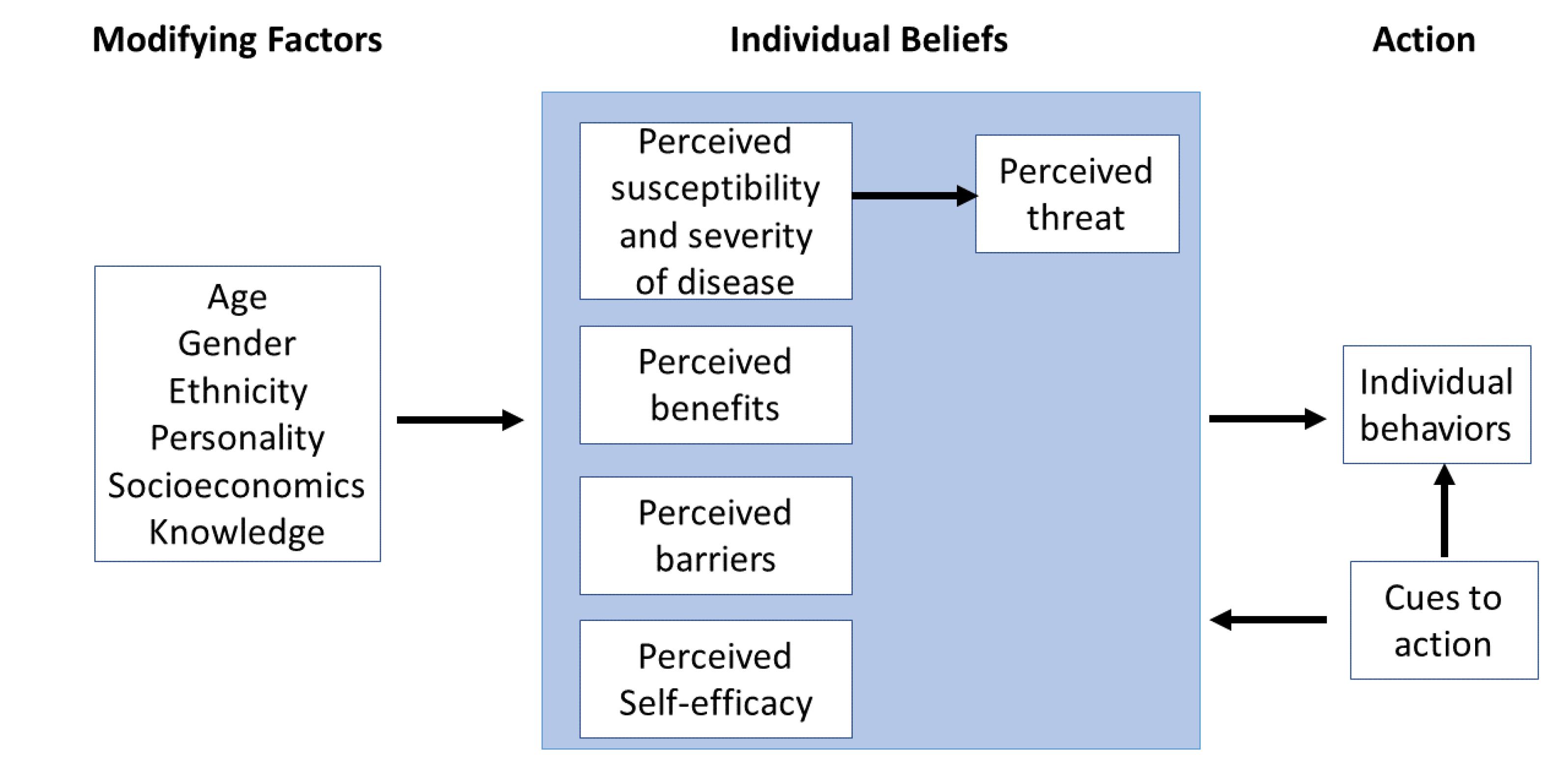
Figure 1.
Components of the HBM (16)
.
Components of the HBM (16)
While studies have utilized HBM to address CRCS, there is limited information on how these constructs affect screening (4,15). Considering the prevalence and mortality rates of CRC, its importance, its impact on the life of the patient and his/her family, the low rate of doing FIT (only 118 out of 589 people had done it), the cultural and religious context of the study area, and the unwillingness of women to cooperate and participate in educational sessions, EI based on HBM was implemented for men aged 50-70 years in Sangan to encourage them to perform CRCS.
Materials and Methods
This is a randomized educational trial that was done from June 8, 2019, to February 19, 2020, in health centers of Sangan, a city in Khorasan Razavi province, Iran. The total number of people aged 50 to 70 years was 1230 (589 men and 641 women). Services for the residents of Sangan city are provided in 2 health centers by health care providers. The study population included all 50-70-year-old men who had never been screened for CRC by FIT, had never been diagnosed with CRC, and were willing to complete a baseline survey. Exclusion criteria included absenteeism for more than two sessions, unwillingness to continue participating in the research project and EI sessions, and participation in similar training sessions (TSs) over the past year.
At first, two health centers were randomly assigned to the control and intervention groups. Then, 53 people from them were selected using simple random sampling method.
Data collection tool was a valid and reliable questionnaire, derived from the results of other studies with little change including, demographic data, knowledge, perceived susceptibility, severity, benefits, barriers, self-efficacy, and behavior. The validity of the questionnaire was measured using content and face validity and its reliability was measured using Cronbach’s alpha coefficient in previous studies. The reliability of different sections of the questionnaire was calculated to be between 0.71 and 0.89 (12,17).
The questionnaire consisted of 95 questions that were presented in 9 sections as follows. In this questionnaire, 23 questions assessed personal characteristics and demographic information (age, height, weight, marital status, level of education, number of children, economic status, occupation, digestive problems, family history of cancer, type of insurance, intention to perform a FIT, weekly exercise, red meat consumption, fruit consumption, vegetable consumption, history of smoking and hookah). Additionally, 14 questions evaluated knowledge of CRC and its screening methods with a score of 2 for correct answers, a score of 1 for “I don’t have any idea” and a score of 0 for “false” replies. Besides, 7, 16, 9, and 20 questions assessed perceived susceptibility, severity, benefits, and barriers, respectively, which were scored on a five-point Likert scale (“strongly disagree, disagree, no idea, agree, and strongly agree”). Questions 1-5 and 7 measured perceived self-efficiency, which were scored on a five-point Likert scale (“never, a little, no idea, most of the time, and always” from 1 to 5, and in cases where the question was negative, the score was reversed). Finally, the behavior was measured by a question with the following options: “I have done a FIT”, “I have not done the FIT but I’m going to do it”, and “I have not decided to have a FIT”. In the present study, the reliability of knowledge, perceived susceptibility, severity, benefits, barriers, and self-efficacy were 0.68, 0.69, 0.87, 0.73, 0.71, and 0.67, respectively, using Cronbach’s alpha coefficient.
After explaining the objectives of the program, informed written consent was obtained from each participant. Then, the pre-test was done by self-report method and the results were analyzed. EI based on HBM for the intervention group was performed in four 60-minute TSs in 3 groups of 15-20 people by lecture, questions and answers, group discussion, brainstorming methods, and demonstration of the test. The educational content was based on credible and up-to-date data from the Ministry of Health on the importance of early diagnosis, a variety of diagnostic methods for CRC, and FIT (18). The EI was held in the assembly hall of the health center, which was equipped with a video projector and a computer, in the evening shift. The details of the TSs are presented in Table 1.
Table 1.
Details of the Training Sessions
|
Sessions and Duration (min)
|
Objectives
|
Educational Contents
|
Educational Methods
|
Teaching Assistant Tools
|
| The first session/60 minutes |
Promoting the knowledge |
The prevalence of CRC in Iran, people at risk of CRC, the role of lifestyle in the development of CRC, risk factors, the importance of early diagnosis, and FIT |
Lecture with questions and answers |
PowerPoint, video projector, whiteboards |
| The second session/60 minutes |
Arousal of perceived susceptibility and severity |
Increasing the perceived susceptibility and severity of participants by providing information about CRC and consequences of not doing the FIT |
Lecture, group discussion, questions and answers |
PowerPoint, video projector, whiteboards |
| The third session/60 minutes |
Promoting perceived benefits, overcoming and reducing perceived barriers |
The benefits of performing CRCS and FIT and the obstacles to doing it |
Lecture, brainstorming, group discussion, questions and answers |
PowerPoint, video projector, whiteboards |
| The fourth session/60 minutes |
Improving self-efficacy |
Informing participants about performing a FIT and to do so once a year, with or without the supervision of another person |
Lecture with questions and answers and practical demonstration of the test |
PowerPoint, video projector, whiteboards |
A TS was also held with the aim of informing the families of the intervention group to encourage the elderly to perform the FIT. Until one month after the end of the EI, a health message related to CRCS and FIT was sent to the participants every night. Eventually, one month after EI, participants in the two groups filled out the questionnaire again.
The data were analyzed using SPSS version 18.0. Data normality was assessed by Kolmogorov–Smirnov test. Chi-square test was applied to compare qualitative variables in two groups. Independent t-test was used to compare quantitative variables between the two groups. P values less than 0.05 were considered statistically significant. In the present study, 6 participants were removed from the study. Flowchart of the study process and the EI used in this research can be seen in Figure 2.
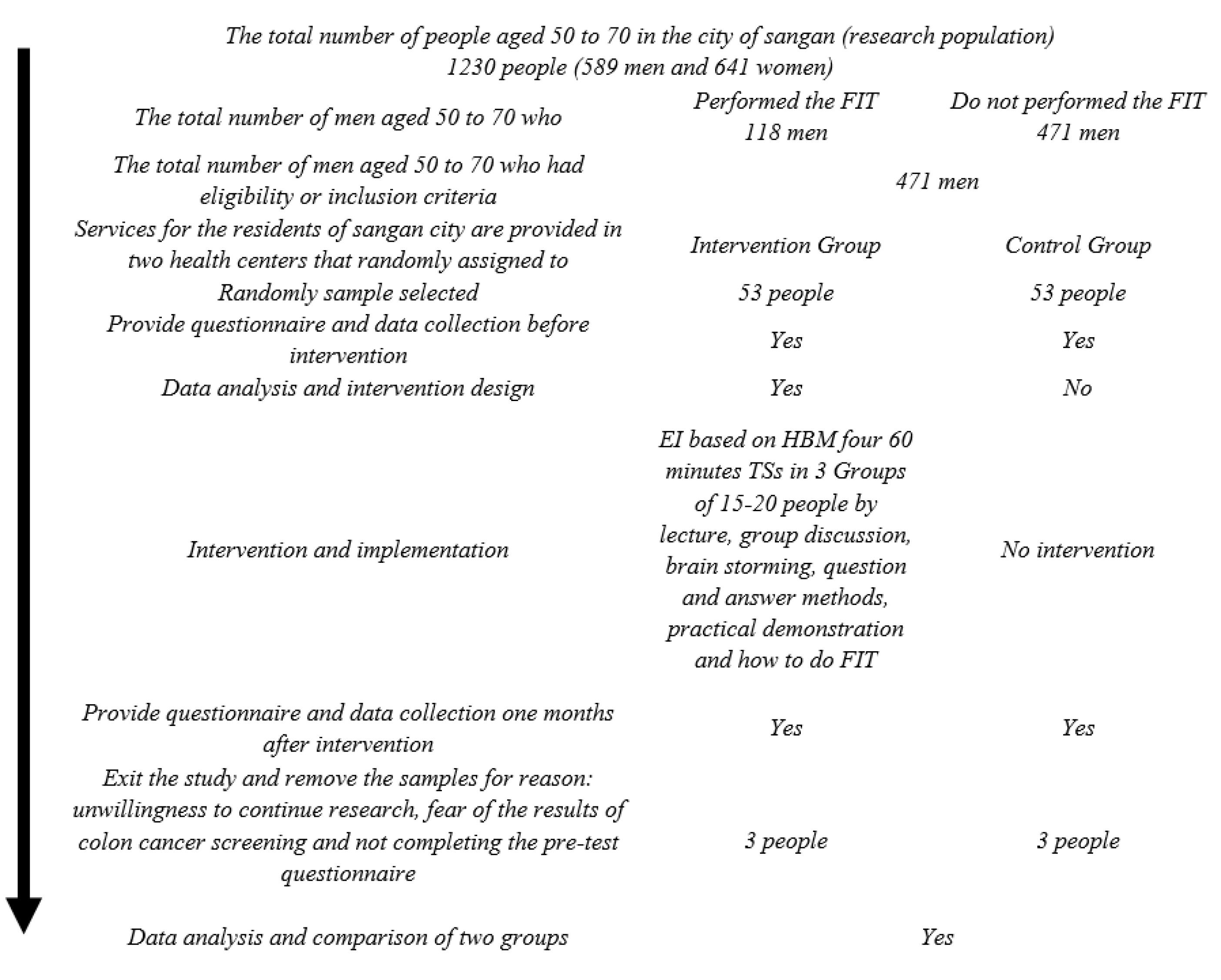
Figure 2.
Flowchart of Study Process and EI Used in this Research
.
Flowchart of Study Process and EI Used in this Research
Results
No significant difference was observed between the two groups in terms of demographic characteristics (Table 2).
Table 2.
Demographic Information in Two Groups before the Intervention
|
Qualitative variables
|
Intervention group No. (%)
|
Control group No. (%)
|
P
value*
|
| A visit to the doctor due to digestive problems |
Yes |
17 (34) |
13 (26) |
0.26 |
| No |
33 (66) |
37 (74) |
| Marital status |
Single |
50 (100) |
1 (2) |
0.5 |
| Married |
33 (66) |
49 (98) |
| Family history of cancer |
Yes |
17 (34) |
12 (24) |
0.19 |
| No |
33 (66) |
38 (76) |
| Intention to perform FIT |
Yes |
19 (38) |
17 (34) |
0.42 |
| No |
31 (62) |
33 (66) |
| Weekly exercise |
I don't exercise. |
22 (38) |
26 (52) |
0.26 |
| Less than 150 minutes |
17 (44) |
19 (38) |
| 150 minutes and more |
11 (22) |
5 (10) |
| Red meat consumption per week |
1-2 times |
40 (80) |
40 (80) |
1 |
| 3-4 times |
9 (18) |
9 (18) |
| Daily and more |
1 (2) |
1 (2) |
| Fruit consumption per week |
1-2 times |
8 (16) |
12 (24) |
0.13 |
| 3-4 times |
17 (34) |
24 (48) |
| Daily and more |
25 (50) |
14 (28) |
| Vegetable consumption per week |
1-2 times |
16 (32) |
20 (40) |
0.21 |
| 3-4 times |
24 (48) |
26 (52) |
| Daily and more |
10 (20) |
4 (8) |
| Cigarette consumption |
Yes |
3 (6) |
7 (14) |
0.16 |
| No |
47 (94) |
43 (86) |
| Hookah consumption |
Yes |
2 (4) |
3 (6) |
0.50 |
| No |
48 (96) |
47 (94) |
|
|
|
Mean±SD
|
Mean±SD
|
P
value **
|
| Age |
|
55.62 ± 4.59 |
57.06 ± 4.97 |
0.14 |
| Number of children |
|
4.00 ± 1.48 |
4.04 ± 1.18 |
0.91 |
| Body mass index |
|
25.08 ± 3.24 |
24.62 ± 3.69 |
0.51 |
* Chi-square test; ** Independent t-test.
SD, Standard deviation.
Before the EI, significant differences were not observed in the mean scores of the knowledge and other HBM constructs between the two groups, except for perceived barriers (P > 0.05). However, one month after the EI, significant differences were observed in these constructs between the two groups (P < 0.05). Additionally, the results of the paired t-test showed that after the intervention, the scores of all constructs in the intervention group improved, and the mean score of perceived barriers decreased significantly (Table 3).
Table 3.
Comparison of the Mean ± SD Scores of HBM Constructs in the Two Groups
|
Constructs
|
Group
|
Before the Intervention
(Mean±SD)
|
One Month After the Intervention (Mean±SD)
|
P
Value *
|
Changes in Mean Score
|
Knowledge
0-28 |
Intervention |
18.54 ± 4.25 |
22.02 ± 2.52 |
< 0.0001 |
3.48 ± 4.20 |
| Control |
17.8 ± 2.8 |
17.8 ± 3.2 |
0.90 |
-0.02 ± 2.42 |
|
P value** |
|
0.31 |
< 0.0001 |
|
< 0.0001 |
Perceived susceptibility
7-45 |
Intervention |
22.0 ± 3.33 |
27.14 ± 1.85 |
< 0.0001 |
5.14 ± 3.19 |
| Control |
21.14 ± 2.87 |
21.28 ± 1.94 |
0.62 |
0.12 ± 1.72 |
|
P value** |
|
0.17 |
< 0.0001 |
|
< 0.0001 |
Perceived severity
16-80 |
Intervention |
54.68 ± 9.35 |
70.82 ± 5.73 |
< 0.0001 |
16.14 ± 9.40 |
| Control |
57.46 ± 8.41 |
57.58 ± 7.93 |
0.82 |
0.12 ± 3.63 |
|
P value** |
|
0.12 |
< 0.0001 |
|
< 0.0001 |
Perceived benefits
9-45 |
Intervention |
36.54 ± 4.28 |
41.92 ± 1.86 |
< 0.0001 |
5.38 ± 3.83 |
| Control |
36.34 ± 3.87 |
37.44 ± 3.53 |
0.01 |
1.1 ± 1.53 |
|
P value** |
|
0.81 |
< 0.0001 |
|
< 0.0001 |
Perceived barriers
20-100 |
Intervention |
54.34 ± 10.96 |
31.02 ± 6.87 |
< 0.0001 |
-23.32 ± 11.87 |
| Control |
59.82 ± 9.50 |
58.28 ± 9.43 |
0.008 |
-1.54 ± 3.97 |
|
P value** |
|
0.009 |
0.0001 |
|
< 0.0001 |
Self-efficacy
7-35 |
Intervention |
21.74 ± 4.71 |
30.92 ± 1.75 |
< 0.0001 |
9.18 ± 4.62 |
| Control |
21.46 ± 3.81 |
21.64 ± 4.41 |
0.73 |
0.18 ± 3.77 |
|
P value** |
|
0.74 |
< 0.0001 |
|
< 0.0001 |
* Paired t-test; ** Independent t-test
Before the EI, none of the participants had performed the FIT, but after the EI, 70% of participants in the intervention group and only 4% in the control group performed the FIT. The results of the chi-square test showed a significant difference between the two groups (P < 0.0001) (Table 4).
Table 4.
Frequency Distribution of Performing FIT in the Two Groups
|
Variable/group
|
Before intervention
|
One Months After Intervention
|
Intervention
No. (%)
|
Control
No. (%)
|
Intervention
No. (%)
|
Control
No. (%)
|
| Yes, I have done a FIT. |
0 (0) |
0(0) |
35(70) |
2(4) |
| No, I have not done the FIT but I am going to do it. |
19 (38) |
17(34) |
13(26) |
22(44) |
| No, I have not decided to have a FIT. |
31(62) |
33(66) |
2(4) |
26(52) |
|
P value* |
0.25 |
< 0.0001 |
Discussion
Screening tests are of crucial importance in diagnosing colorectal cancer. It is essential to study the factors affecting CRCS and design EIs based on theoretical frameworks and models such as HBM (19). In our study, after the implementation of the EI, the knowledge score in the intervention group increased by about 4 points, which is in line with the findings of other studies (19-23). Knowledge is an indispensable part of any behavior change (22). After the pre-test analysis, educational needs were identified in the field of knowledge that included successful treatment for bowel cancer, signs of CRC, and the impact of family history, smoking, and inactivity on the incidence of CRC. They were taught by lecturing and questions and answers methods, which increased the subjects’ knowledge in the intervention group.
Perceived susceptibility and severity include people’s subjective understanding of the risk that harms their health and the individual’s perception of the degree of harm, or a more dangerous situation resulting from a specific behavior that can be the result of a disease (16). It is believed that this construct is a prerequisite and a necessary stimulus for the formation of preventive behaviors (16,23). The EI caused the subjects in the intervention group to feel more susceptible and understand the consequences and severity of the disease. Our findings are in line with the results of the study by Hatami et al (3), indicating that the perceived severity of the participants increased significantly after the intervention by using audiovisual CDs, and the results of the study by Rakhshanderouet al (24). The increase in perceived susceptibility and severity score in this study is likewise compatible with the findings of several other studies (19,22,23). However, the results of this study regarding the perceived severity after the EI are not aligned with the results of the study by Alavi Langroodi et al (25). We used strategies, such as highlighting the risks of CRC, to increase the perceived susceptibility and severity of the participants to perform FIT. It is recommended that a training program should be implemented to improve the perception and change the attitude of 50-year-old men about the negative consequences of not having FIT and its effects on various aspects of quality of life (individual, physical, social, economic, and family).
The EI increased the mean score of perceived benefits, which is similar to the results of the studies conducted by Hatami et al (3), Rawl et al (23), and Khazaei et al (22), indicating that EI increased perceived benefits and barriers to screening for CRC, and is aligned with the results of Temucin and Nahcivan (26). It is possible that the pre-test played a role in motivating and attracting the attention of the participants of the control group to learn the benefits of screening, and as a result, their perceived benefits score increased after the intervention.
The findings also showed a greater decrease in the score of perceived barriers in the intervention group compared with the control, which is similar to the results of studies by Hatami et al (3), Rawl et al (23), Khazaei et al (22), and Temucin and Nahcivan (26), indicating that following the screening program, their scores of perceived barriers were reduced. However, it is not consistent with the results of studies by Rakhshanderou et al (24) and Alavi Langroodi et al (25), indicating a difference in the mean score of perceived barriers between the two groups. To reduce barriers, it was assured that this test was free and these tests were performed by professionals of the same gender.
The current educational program caused a significant improvement in the self-efficacy score of the intervention group participants. These changes were similar to the results of other previous studies (3,19,24). People with high perceived self-efficacy are more committed to spending more time to overcome possible obstacles and participate in programs and activities in difficulties and problems (16,19). Due to the low self-efficacy of the intervention group and based on the analysis of educational needs for the intervention group in performing FIT and their ability to perform this test at any time and in any place with or without the supervision of another person, the practical steps of performing the test were taught to the participants.
At the beginning of the program, none of the participants performed the FIT and only 38% in the intervention and 34% in the control group intended to perform the test, indicating no significant difference between the two groups. However, after the EI, 70% of the participants in the intervention group and only 4% of the participants in the control group performed the FIT, indicating the effect of EI designed by researchers on the participation rate of the intervention group in the FIT. The results of our study are consistent with those of the study by Gholampour et al (19), indicating that 74% of the participant in the intervention group and 6% in the control group had FOBT done after the intervention (19). In their study, Khani Jeihooni et al (13) reported that the rate of participation in the FOBT in the intervention group was 5 times higher than that of the control group. Additionally, Khazaei et al (22) stated that the rate of participation in occult blood testing significantly increased in the intervention group in comparison with the control group. However, the results of this study were not consistent with the findings of Walsh et al (27), indicating no statistically significant difference in CRC screening rates between the two groups, and the results of Arnold et al, indicating that there were not significant differences in FIT completion between those receiving an automated call and those receiving a personal call (28).
The strengths of this study include objective measurement of CRCS behavior, existence of the control group, random assignment of participants, use of appropriate methods, and engaging support providers like family members. One of the limitations of this study was the cultural and religious context of the study area and the unwillingness of women to cooperate and participate in educational sessions that were removed from the study. Another limitation of this study was the use of a self-report method. Additionally, follow-up was performed just one month after the EI. It is suggested that other researchers select the study participants from all individuals aged 50 to 70 years so that the results can be generalized to the whole community.
Conclusion
Design and implementation of EI based on HBM had positive impacts on the individuals’ knowledge, perceived severity, susceptibility, benefits, and their perceived barriers in order to empower and encourage people to perform CRCS and do FIT for CRC prevention. Consequently, the officials of Sangan Health Center and other health centers are recommended to use the constructs of the HBM to encourage men and women aged 50 to 70 to perform FIT.
Acknowledgements
The authors gratefully acknowledge all primary care providers at the participating health centers, without whose involvement this study could not have been done. We sincerely thank our participants for their collaboration in this study and all those who helped us in this research.
Authors’ Contribution
Conceptualization: Mohammad Asadpour, Mostafa Nasirzadeh.
Data Curation: Naser Honaramouz Rodi.
Formal analysis: Mohammad Asadpour.
Funding acquisition: Mohammad Asadpour.
Investigation: Naser Honaramouz Rodi, Mostafa Nasirzadeh.
Methodology: Mostafa Nasirzadeh, Ali Mehdipour.
Project administration: Mohammad Asadpour, Mostafa Nasirzadeh.
Resources: Naser Honaramouz Rodi.
Software: Mohammad Asadpour.
Supervision: Mohammad Asadpour.
Validation: Mohammad Asadpour, Mostafa Nasirzadeh.
Visualization: Naser Honaramouz Rodi.
Writing–original draft: Mohammad Asadpour, Mostafa Nasirzadeh, Naser Honaramouz Rodi, Ali Mehdipour.
Writing–review & editing: Mohammad Asadpour, Mostafa Nasirzadeh, Naser Honaramouz Rodi, Ali Mehdipour.
Competing Interests
The authors have no conflict of interests associated with the material presented in this paper.
Ethical Approval
This study was approved by the Ethics Committee of the Vice Chancellor for Research and Technology of Rafsanjan University of Medical Sciences (IR.RUMS.REC.1398.168).
Funding
This study was funded by Rafsanjan University of Medical Sciences, Rafsanjan, Iran.
References
- World Health Organization (WHO). Cancer, Key Fact. Available from: https://www.who.int/news-room/fact-sheets/detail/cancer. Updated February 3, 2022. Accessed May 13, 2022.
- So WK, Law BM, Choi KC, Chan DN, Chan CW. A family-based multimedia intervention to enhance the uptake of colorectal cancer screening among older South Asian adults in Hong Kong: a study protocol for a cluster randomized controlled trial. BMC Public Health 2019; 19(1):652. doi: 10.1186/s12889-019-6995-7 [Crossref] [ Google Scholar]
- Hatami T, Noroozi A, Tahmasebi R, Rahbar A. Effect of multimedia education on nutritional behaviour for colorectal cancer prevention: an application of health belief model. Malays J Med Sci 2018; 25(6):110-20. doi: 10.21315/mjms2018.25.6.11 [Crossref] [ Google Scholar]
- Lin TY, Chuang ST, Huang SF, Hsu HP, Lu LT, Guo JL. Likelihood of a fecal occult blood test uptake among older adults: comparisons between health professionals and healthcare volunteers based on the health belief model. BMC Geriatr 2019; 19(1):51. doi: 10.1186/s12877-019-1067-5 [Crossref] [ Google Scholar]
- Hassanlouei B, Ostovar A, Motevalian SA, Ghanbari Motlagh A, Moradi Y, Salehi M. Colorectal cancer screening program results in Iran. Med J Islam Repub Iran 2022; 36:118. doi: 10.47176/mjiri.36.118 [Crossref] [ Google Scholar]
- Onyoh EF, Hsu WF, Chang LC, Lee YC, Wu MS, Chiu HM. The rise of colorectal cancer in Asia: epidemiology, screening, and management. Curr Gastroenterol Rep 2019; 21(8):36. doi: 10.1007/s11894-019-0703-8 [Crossref] [ Google Scholar]
- Miller CA, Lafata JE, Thomson MD. The effects of personalizing colorectal cancer risk communication on risk perceptions and health behavior intentions: a randomized trial of average-risk adults. J Cancer Educ 2021; 36(4):719-27. doi: 10.1007/s13187-020-01694-5 [Crossref] [ Google Scholar]
- Lee SY, Lee EE. Access to health care, beliefs, and behaviors about colorectal cancer screening among Korean Americans. Asian Pac J Cancer Prev 2018; 19(7):2021-7. doi: 10.22034/apjcp.2018.19.7.2021 [Crossref] [ Google Scholar]
- Nikbakht HA, Shokri-Shirvani J, Ashrafian-Amiri H, Ghaem H, Jafarnia A, Alijanpour S. The first screening program for colorectal cancer in the North of Iran. J Gastrointest Cancer 2020; 51(1):165-71. doi: 10.1007/s12029-019-00226-9 [Crossref] [ Google Scholar]
- Ferlizza E, Solmi R, Miglio R, Nardi E, Mattei G, Sgarzi M. Colorectal cancer screening: assessment of CEACAM6, LGALS4, TSPAN8 and COL1A2 as blood markers in faecal immunochemical test negative subjects. J Adv Res 2020; 24:99-107. doi: 10.1016/j.jare.2020.03.001 [Crossref] [ Google Scholar]
- Kazi E, Sareshwala S, Ansari Z, Sahota D, Katyal T, Tseng W. Promoting colorectal cancer screening in South Asian Muslims living in the USA. J Cancer Educ 2021; 36(4):865-73. doi: 10.1007/s13187-020-01715-3 [Crossref] [ Google Scholar]
- Javadzade SH, Reisi M, Mostafavi F, Babaei Heydarabadi A, Tavassoli E, Sharifirad G. Barriers related to fecal occult blood test for colorectal cancer screening in moderate risk individuals. J Educ Health Promot 2014; 3:120. doi: 10.4103/2277-9531.145928 [Crossref] [ Google Scholar]
- Khani Jeihooni A, Kashfi SM, Shokri A, Kashfi SH, Karimi S. Investigating factors associated with FOBT screening for colorectal cancer based on the components of health belief model and social support. Asian Pac J Cancer Prev 2017; 18(8):2163-9. doi: 10.22034/apjcp.2017.18.8.2163 [Crossref] [ Google Scholar]
- Williams RM, Wilkerson T, Holt CL. The role of perceived benefits and barriers in colorectal cancer screening in intervention trials among African Americans. Health Educ Res 2018; 33(3):205-17. doi: 10.1093/her/cyy013 [Crossref] [ Google Scholar]
- Khodaveisi M, Vesali Fallah S, Amini R, Tapak L. Effect of education based on the health belief model on treatment adherence in patients with heart valve replacement surgery. J Educ Community Health 2023; 10(1):35-42. doi: 10.34172/jech.2023.1958 [Crossref] [ Google Scholar]
- Glanz K, Rimer BK, Viswanath K. Health Behavior: Theory, Research, and Practice. 5th ed. Jossey-Bass; 2015. p. 512.
- Javadzade SH, Reisi M, Mostafavi F, Hasanzade A, Shahnazi H, Sharifirad G. Factors associated with the fecal occult blood testing for colorectal cancer screening based on health belief model structures in moderate risk individuals, Isfahan, 2011. J Educ Health Promot 2012; 1:18. doi: 10.4103/2277-9531.99218 [Crossref] [ Google Scholar]
- Kosha A, Najmi M, Mahdavi Hezaveh AR, Moghithi A, Mutlat AG, YarAhmadi S, et al. The set of basic interventions for non-communicable diseases in Iran’s primary health care system (IRAPEN). Tehran: Mojassameh, Ministry of Health and Medical Education, Department of Health, Non-communicable diseases management office; 2017. p. 119.
- Gholampour Y, Jaderipour A, Khani Jeihooni A, Kashfi SM, Afzali Harsini P. The effect of educational intervention based on health belief model and social support on the rate of participation of individuals in performing fecal occult blood test for colorectal cancer screening. Asian Pac J Cancer Prev 2018; 19(10):2777-87. doi: 10.22034/apjcp.2018.19.10.2777 [Crossref] [ Google Scholar]
- Ghobadi Dashdebi K, Noroozi A, Tahmasebi R. Factors predicting fecal occult blood testing among residents of Bushehr, Iran, based on the health belief model. Asian Pac J Cancer Prev 2016; 17(S3):17-22. doi: 10.7314/apjcp.2016.17.s3.17 [Crossref] [ Google Scholar]
- Mojica CM, Morales-Campos DY, Carmona CM, Ouyang Y, Liang Y. Breast, cervical, and colorectal cancer education and navigation: results of a community health worker intervention. Health Promot Pract 2016; 17(3):353-63. doi: 10.1177/1524839915603362 [Crossref] [ Google Scholar]
- Khazaei S, Salmani F, Moodi M. Evaluation of health belief model-based educational intervention on colorectal cancer screening behavior at South Khorasan, Iran. J Educ Health Promot 2022; 11:52. doi: 10.4103/jehp.jehp_279_21 [Crossref] [ Google Scholar]
- Rawl SM, Skinner CS, Perkins SM, Springston J, Wang HL, Russell KM. Computer-delivered tailored intervention improves colon cancer screening knowledge and health beliefs of African-Americans. Health Educ Res 2012; 27(5):868-85. doi: 10.1093/her/cys094 [Crossref] [ Google Scholar]
- Rakhshanderou S, Maghsoudloo M, Safari-Moradabadi A, Ghaffari M. Theoretically designed interventions for colorectal cancer prevention: a case of the health belief model. BMC Med Educ 2020; 20(1):270. doi: 10.1186/s12909-020-02192-4 [Crossref] [ Google Scholar]
- Alavi Langroodi SM, Fallahzadeh H, Mostafavi F. The effect of education based on health belief model on knowledge and attitude of health care workers towards colon cancer screening in Yazd, Iran. J Health Syst Res 2019; 15(3):177-83. doi: 10.48305/hsr.2020.15.3.109 [Crossref] [ Google Scholar]
- Temucin E, Nahcivan NO. The effects of the nurse navigation program in promoting colorectal cancer screening behaviors: a randomized controlled trial. J Cancer Educ 2020; 35(1):112-24. doi: 10.1007/s13187-018-1448-z [Crossref] [ Google Scholar]
- Walsh J, Potter M, Salazar R, Ozer E, Gildengorin G, Dass N. PreView: a randomized trial of a multi-site intervention in diverse primary care to increase rates of age-appropriate cancer screening. J Gen Intern Med 2020; 35(2):449-56. doi: 10.1007/s11606-019-05438-0 [Crossref] [ Google Scholar]
- Arnold CL, Rademaker AW, Morris JD, Ferguson LA, Wiltz G, Davis TC. Follow-up approaches to a health literacy intervention to increase colorectal cancer screening in rural community clinics: a randomized controlled trial. Cancer 2019; 125(20):3615-22. doi: 10.1002/cncr.32398 [Crossref] [ Google Scholar]