J Educ Community Health. 11(4):198-206.
doi: 10.34172/jech.2996
Original Article
Strategies to Increase Access to mHealth Wearable Devices for Hypertension Control in African-Born Immigrants: A Risk-Benefit Analysis
Nelson McNova Bryant 1, * 
Author information:
1Department of Public and Community Health, School of Health Sciences, Liberty University, Lynchburg, Virginia, United States
Abstract
Background: Studies on the use of mobile health (mHealth) wearable devices by African Americans to control hypertension have been limited. This study aligns with ongoing efforts to uncover the benefits of using such devices to improve hypertension management in African-born immigrant groups. It focused on long-term strategies to increase access to mHealth wearables. It also analyzed their hypertension risk factors and the challenges of using such devices.
Methods: This causal-comparative study was conducted in 2024 among 100 African-born immigrants aged 45-75 in Arizona’s nine medically underserved primary care areas. A risk-benefit analysis was used to identify the risks associated with uncontrolled hypertension and the benefits of using mHealth wearable devices. Independent samples t-test was used to compare mean arterial pressure (MAP) between the two groups.
Results: The strategies to promote access to mHealth wearable devices for hypertension control in African-born immigrants consisted of government-subsidized smartwatches (33.8%) and unlimited access to mHealth data (29.6%). The most prevalent hypertension risk factors included unhealthy diet (21.7%), physical inactivity (21.7%), and obesity (12.5%). Most participants (51.6%) were overweight. Group 1 participants benefited from using mHealth wearable devices with a lower MAP (99 mm Hg) compared to group 2 (103 mm Hg) (P<0.001).
Conclusion: The findings of this study contributed to the existing knowledge about the most prevalent hypertension risk factors in African-born immigrants and their challenges in managing hypertension. Despite being excluded from major mHealth research, they can benefit from using smartwatches, unlimited access to mHealth data, and medical education to manage hypertension better.
Keywords: African-born immigrants, Hypertension management, mHealth benefits, Risk factors, Smartwatches
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Bryant NM. Strategies to increase access to mHealth wearable devices for hypertension control in African-born immigrants: a risk-benefit analysis. J Educ Community Health. 2024; 11(4):198-206. doi:10.34172/jech.2996
Introduction
Mobile health (mHealth) has received particular attention for efficiently managing chronic diseases as different ethnic and racial groups adopted it.There has been an increasing interest, especially among minority groups in the United States (U.S.), in using mHealth wearable devices to track their health regularly (1,2). Americans use mHealth technology, including smartphone health applications to count their steps and manage their chronic diseases, including hypertension (3). Nevertheless, only a few African-born immigrants use mHealth wearable devices to manage their health conditions and promote wellness (4). African-born immigrants in Arizona mistrust mHealth technology and fear sharing their health data, mainly due to data breaches (5).
Only 35% of Americans diagnosed with hypertension use mHealth wearable devices to monitor their blood pressure (BP) (6). Using mHealth wearable devices to control hypertension has been most popular among adults aged 18-49 with a college education as part of lifestyle interventions (4). Most users have a history of cardiovascular diseases or risk factors. African-born immigrants particularly have a sedentary lifestyle, limited financial resources, and inadequate access to in-person medical services (7,8). They assume that their health outcomes may not be as favorable as other ethnic groups, such as Caucasian Americans. Due to cultural influence, they are significantly less likely to report the awareness of having hypertension and seek medical care (9,10). Hypertension remains the leading risk factor for developing heart diseases and stroke in the world, the U.S., and particularly Arizona. Hypertension affects 1.3 billion adults globally (8,11). In the U.S., 1 in 2 adults, or 116 million Americans (47.3%) are affected, and 67 million Americans (73%) did not achieve BP control, especially African Americans (12).
African-born immigrants lack hypertension monitoring, which leads to cognitive decline, heart failure, myocardial infarction, stroke, kidney damage, chest pain, visual impairments, peripheral artery disease, and hypertensive crisis (13). Proper hypertension monitoring in other demographic groups in the US, especially among adults with inadequate BP control, led to improvement in hypertension self-management and a better quality of life (14,15). The present study aimed to address the lack of long-term strategies for increased accessibility to mHealth wearable devices for hypertension control in African-born immigrants in Arizona. It also assessed their awareness of hypertension risk factors and the benefits of mHealth wearable devices to achieve hypertension control.
Importance of mHealth and mHealth Studies
The users of mHealth wearable devices, such as smartwatches, smartphones, bracelets, and tablets benefit from expanded access to healthcare services (16). As the need for in-person medical visits decreases, costs associated with chronic disease management decrease. These devices help manage hypertension. Their use leads to enhanced patient engagement. They also facilitate personalized care for patients with limited resources from underserved and rural areas (17). They make it easy to collect and analyze real-time health data from patients to identify trends and provide customized treatment plans.
Therefore, mHealth studies play pivotal roles in advancing digital knowledge, focusing on smart wearable devices to improve patient health outcomes (16). These studies contribute to evaluating the effectiveness of different smart wearable devices and the clinical implications of mHealth interventions in various population groups. Similar studies have explored strategies for increased access to smart wearable devices to manage hypertension in a specific population group (4,15). Other mHealth studies emphasize data privacy and security, which are important to protect sensitive health information of patients (17). Interactive mHealth interventions help patients with inadequate hypertension control achieve a three times greater BP reduction than similar patients who do not use mHealth interventions (14).
It is crucial to emphasize the implication of mHealth in the context of hypertension management in African-born immigrants, who are the central focus of this study. The use of mHealth wearable devices by African-born immigrants was investigated as they have the potential to help them manage hypertension efficiently (7). Such devices contribute to behavior changes in African-born immigrants as they leverage this technology to address their unique challenges, including a sedentary lifestyle and a lack of hypertension awareness (9). African-born immigrants can regularly monitor their BP and receive reminders to take their scheduled antihypertensives. They can also help improve provider-patient relationships due to personalized care.
Nevertheless, the application of mHealth interventions to improve hypertension management in African-born immigrants as a distinct sub-group has been limited (9). Their risk factors and the benefits of using mHealth wearable devices, especially in Arizona, are not fully understood. This study aligns with efforts to bridge the ethnic differences in understanding hypertension management. Substantial ethnic disparities lead to poor hypertension control rates (> 140/90 mm Hg) in African Americans whereas Caucasian Americans achieve better hypertension control rates (< 130/80 mm Hg) (18). There is still a gap in research on the strategies to make mHealth wearable devices more accessible to African-born immigrants in Arizona to achieve hypertension control (16,17).Over the last decade, only 39% of African Americans achieved hypertension control while 49% of their non-Hispanic Caucasian counterparts could manage it (19-22).
The study is an opportunity to integrate African-born immigrants’ differences in applying mHealth tools to manage chronic hypertension. It aimed to investigate the strategies to increase access to mHealth wearable devices for African-born immigrants in the U.S. It also analyzed the risk factors and benefits of using such devices to improve hypertension control. Three research questions guided the study:
-
RQ1: What are the prevalent risk factors leading to hypertension among African-born immigrants?
-
RQ2: What are the benefits of using mHealth wearable devices for African-born immigrants?
-
RQ3: How can mHealth wearable devices be more accessible to African-born immigrants?
Materials and Methods
Study Design
This study used a causal-comparative research design to investigate the long-term strategies to increase access to mHealth wearable devices for hypertension control among African-born immigrants in Arizona. It used a risk-benefit analysis to identify the risks associated with uncontrolled hypertension and the benefits of using mHealth wearable devices to counter these risks. It targeted African-born immigrants aged 45-75 residing in Maricopa county, Arizona. All 100 participants were randomly divided into two equal groups and completed the study.
Half of the 100 research participants (the mHealth group or group 1) used mHealth wearable devices for six weeks (12 hours a day from 8 AM to 8 PM). The investigator gave a free and calibrated Dafit smartwatch ($55 value) to all 50 research participants in group 1. The other half (the usual care group) did not use mHealth wearable devices (group 2). The investigator instructed group 2 participants to use manual BP monitoring devices, such as a sphygmomanometer, to check their BP twice daily for six weeks. A free Dafit smartwatch ($55 value) was randomly given as a prize at the end of the study to select 25 out of 50 participants in group 2 to motivate them to sign up for the study. No financial incentives or payment was given to participate in the study. This study is the second part of the research series on a causal relationship between the use of mobile health wearable devices and improved hypertension management in African-born immigrants in Arizona.
Study Setting and Participants
The study was conducted in 2024 in Maricopa county, Arizona, U.S. Maricopa is the largest and most populous county in Arizona, with a population of 4.4 million. The total population of Arizona state is 7.35 million (23). The target population was distributed across nine medically underserved primary care areas (MUAs) in Maricopa County designated by the Arizona Department of Health Services to promote access to essential community health services (11). These areas were referred to as strata, which included the cities and towns of Buckeye, El Mirage, Glendale, Guadalupe, Laveen, Tolleson, Peoria, Phoenix, and Tempe. The study population of interest consisted of African-born immigrants aged 45-75 years who were diagnosed with hypertension. This age group was selected because it is more associated with hypertension than younger populations. It is estimated that 2698 (64%) of these African-born immigrants with hypertension live in Maricopa County (23,24).
Study Procedures
Recruitment and Informed Consent
The investigator reached out to African-born immigrants’ agencies to explain the purpose of this study and to recruit 100 participants. The investigator distributed research recruitment flyers and attended community events to recruit participants (see Supplementary file 1, Section A). The target participants scanned a QR code on the recruitment flyers and signed the consent form before participating in the study (see Supplementary file 1, Section B).
Inclusion Criteria
African-born immigrants aged 45-75 years who were diagnosed with hypertension in the last three years were eligible to participate in the study. Other inclusion criteria included having a reading level of third grade to answer the study questions and living in Maricopa county (23). The exclusion criteria consisted of not having hypertension, inability to take BP independently, being younger than 45 or older than 75 years old, being unable to read at a third-grade level to complete the questionnaire independently, and moving outside Maricopa MUAs at the time of data collection.
Procedure
Stratified random sampling method was used to select 100 participants. Participants were randomly selected from 2698 African-born immigrants in nine MUAs. The investigator used the following formula to determine the target sample size (nh) in each stratum:
Nh denotes the sample size, N denotes the population size, and n denotes the stratum size.
Half (N = 50) of the study participants were randomly assigned to the mHealth group (group 1) and the other half (N = 50) to the usual care group (group 2).
Data Collection Measures
This study used self-designed BP forms and questionnaires to collect information from participants. Each group received a different form and questionnaire with predetermined questions. All participants recorded their BP levels on BP forms (see Section C for group 1 and Section D for group 2, Supplementary file 1) on the first day of participation in the study, at the end of two, four, and six weeks. Participants also completed an electronic questionnaire via encrypted Google Forms (see Section E, Supplementary file 1) for group 1 and (see Section F, Supplementary file 1) for group 2. The questionnaire consisted of 21 questions for group 1 and 17 questions for group 2 and took approximately 20 minutes for all participants. Data collection was done between January and April 2024.
Data Analysis
Data analysis was done using the Statistical Package for the Social Sciences (SPSS) version 29.0. The independent samples t-test was used to compare mean arterial pressure (MAP) between group 1 and group 2. The assumptions of normality and equal variance for the t-test were satisfied in this study. The P values of the Kolmogorov-Smirnov test were P = 0.57 for group 1 and P = 0.009 for group 2. The normal distribution assumption was satisfied in group 2. There was a slight deviation (0.9%) from a normal distribution in group 1 because of two outliers. However, there was no significant violation of normality assumption due to the large sample size. The homogeneity assumption (equal variance) was also satisfied as the P values of Levene’s test for both groups were P > 0.05.
Results
The study analyzed the risk factors for developing hypertension among African-born immigrants before their participation. None of the participants had used mHealth wearable devices before they joined the study.
The Risk Factors Leading to Hypertension Diagnosis in African-born Immigrants
Table 1 shows the most predominant risk factors that the participants had before being diagnosed with hypertension (RQ1). The significant risk factors were unhealthy diet and physical inactivity, which accounted for 19.7% each. Both risk factors were reported by 26 respondents (n = 26). The second leading risk factor was obesity or being overweight (n = 15, 12.5%). The third most common risk factor for hypertension was elevated BP (n = 11, 9.2%). The least prevalent risk factor identified by the participants was consuming too much alcohol (n = 6, 5%), followed by diabetes mellitus (n = 7, 5.8%).
Table 1.
Frequency of Risk Factors before Hypertension Diagnosis
|
|
Responses
|
|
No.
|
Percent
|
| Risk factors before the diagnosis of hypertensiona |
Unhealthy diet |
26 |
21.7 |
| Too much salt intake |
12 |
10.0 |
| Physical inactivity |
26 |
21.7 |
| Obesity/overweight |
15 |
12.5 |
| Too much alcohol |
6 |
5.0 |
| Diabetes mellitus |
7 |
5.8 |
| Elevated (High) BP |
11 |
9.2 |
| Sleep apnea |
9 |
7.5 |
| Elevated heart rate |
8 |
6.7 |
| Total |
120 |
100.0 |
a Dichotomy group tabulated at value 1.
Research participants also identified other risk factors leading to hypertension, including smoking status, body mass index (BMI), MAP, and the frequency of BP monitoring.Only 2.1% of respondents (n = 2) reported that they were either smoking or vaping at the time of data collection. The investigator noted in the limitations of the study other relevant risk factors that were not explored in this study, including environmental or interpersonal factors, such as social support.
Figure 1 showed that the most prevalent BMI category among research participants was 24.4 kg/m2 (16.3%). The second most common BMI category was 24.8 kg/m2 (13.8%). Most research participants (51.6%) were either overweight or obese based on BMI values ranging from 25.9 kg/m2 to 41.6 kg/m2. Only 1.3% of research participants were underweight, with a BMI of 17.2 kg/m2. The MAP of the participants was 102 ± 8.04 six weeks before participating in the study. The findings revealed that before the study, most participants never checked their BP (36.8%). Other participants monitored their BP once to twice a month (28.4%), twice a week, and more than twice a month (10.5%), or once to twice daily (10.2%).
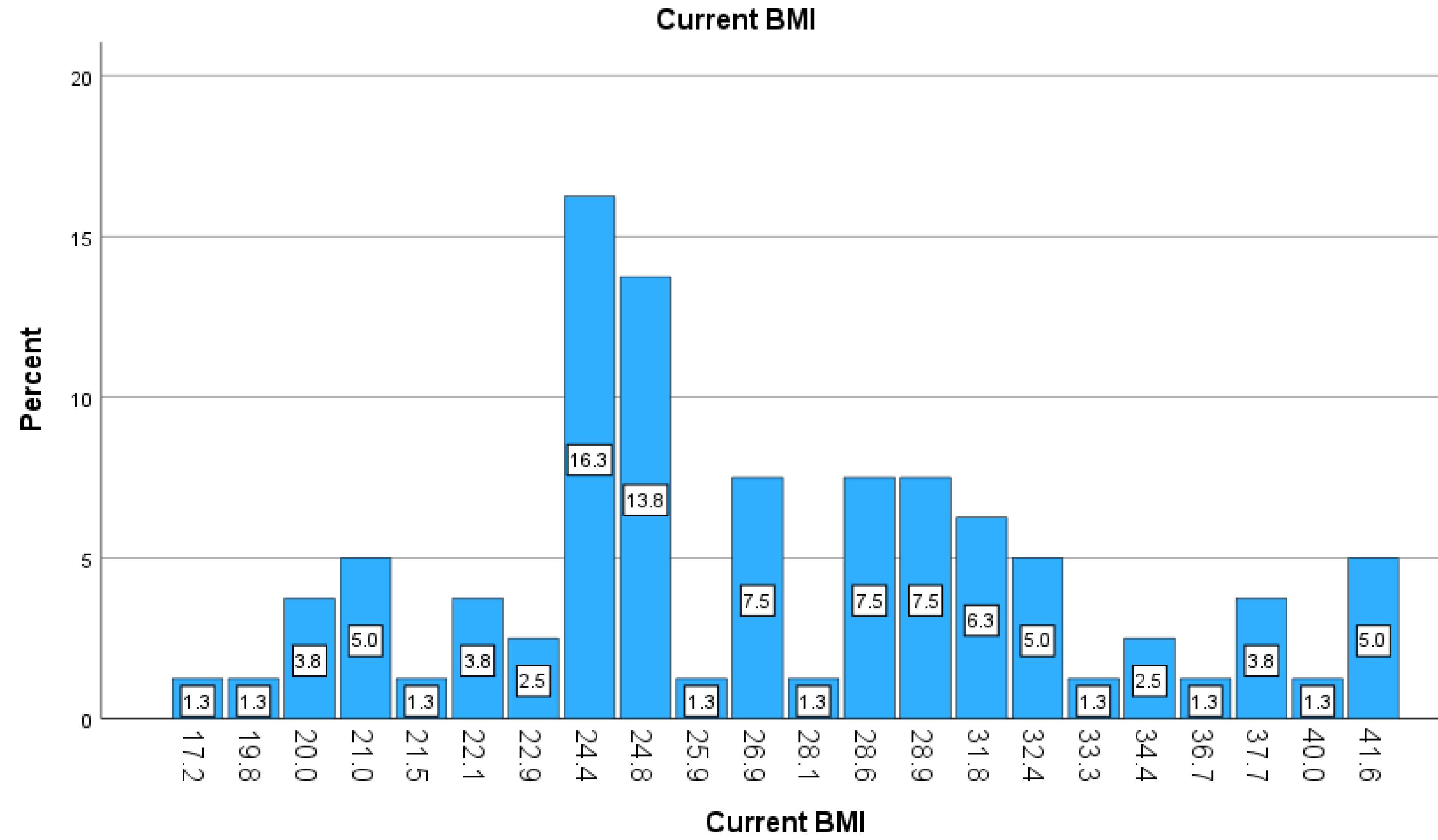
Figure 1.
Current Body Mass Index (BMI) of Participants
.
Current Body Mass Index (BMI) of Participants
The Benefits of Using mHealth Wearable Devices in African-Born Immigrants
The study analyzed the benefits among participants in improving hypertension control using mHealth wearable devices.
Figure 2 shows the responses from group 1 participants about the benefits of using mHealth wearable devices to monitor their BP. Most research participants appreciated the reminder to measure BP promptly (67.4%, n1 = 29) and to perform physical activity (37.2%, n1 = 16). Searching for information about hypertension management and the reminder to take hypertension medications were reported by 20.9% (n1 = 9) each. Recording and synchronizing BP measurement was the least selected benefit (9.3%, n1 = 4).
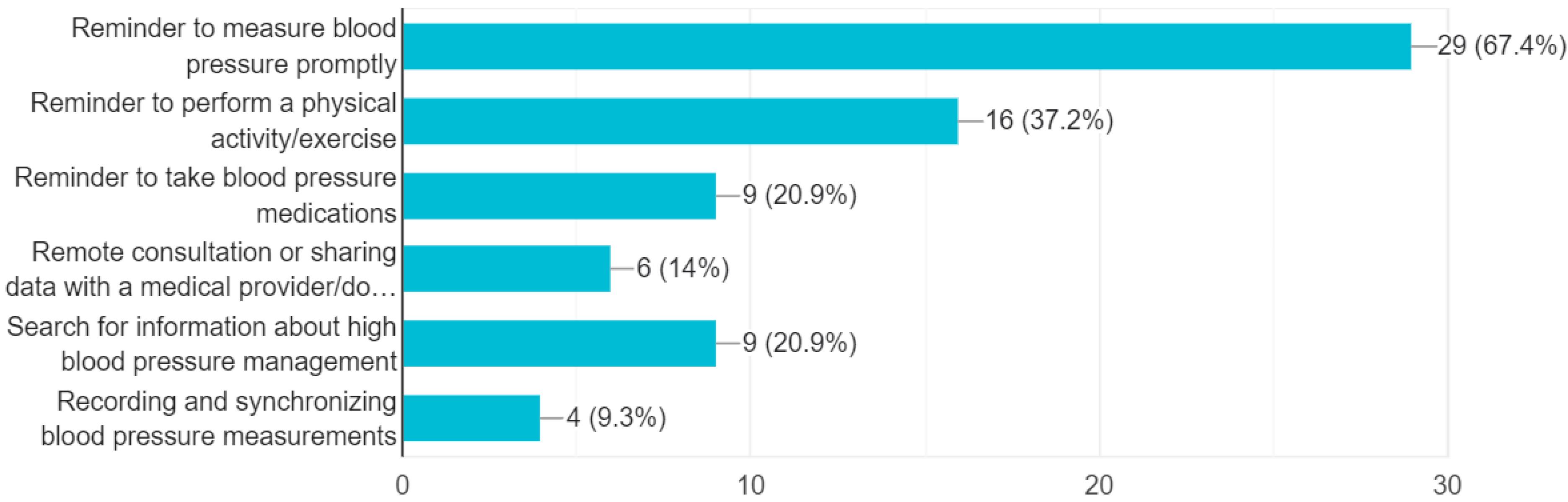
Figure 2.
The Benefits of Using mHealth Wearable Devices in African-born Immigrants
.
The Benefits of Using mHealth Wearable Devices in African-born Immigrants
Approaches for Influencing the Improved Management of mHealth Wearable Devices in African-Born Immigrants
Figure 3 shows different approaches reported by participants in group 1 to influence the improved management of mHealth wearable devices in African-born immigrants. The first two most common approaches included an integrated education for hypertension management focusing on the use of smartwatches (46.9%, n1 = 23) and getting frequent advice from the primary care provider for the better use of smartwatches (46.9%, n1 = 23). The second most common approach reported by research participants (42.9%, n1 = 21) was automated reminders to check BP, exercise, and take medications. Peer support from other patients diagnosed with hypertension (16.3%, n1 = 8) and others (2%, n1 = 1) were the least reported approaches.
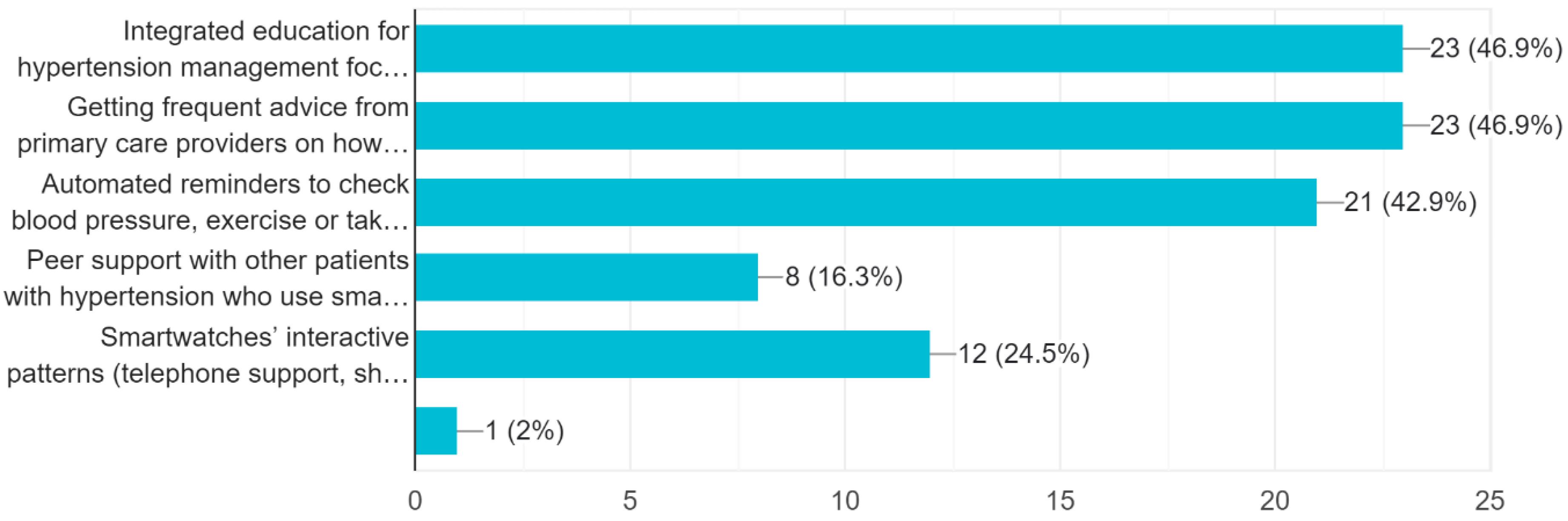
Figure 3.
Approaches for Influencing the Improved Management of mHealth Wearable Devices in African-born Immigrants
.
Approaches for Influencing the Improved Management of mHealth Wearable Devices in African-born Immigrants
Strategies to Make mHealth Wearable Devices More Accessible to African-Born Immigrants
Table 2 shows different strategies reported by research participants to improve the accessibility of mHealth wearable devices for hypertension control in African-born immigrants. The most common strategy was making government-subsidized smartwatches accessible to all low-income group members who need them (33.8%, n1 = 24). The second most common advice was the ability to have free unlimited access to mHealth-based smartwatch data (29.6%, n1 = 21). Ensuring data safety in mHealth applications and devices was another frequent strategy (18.3%, n1 = 13).
Table 2.
Strategies to Make mHealth Wearable Devices More Accessible to African-born Immigrants
|
Advice for More Accessibility of mHealth Wearable Devices Frequencies
|
Responses
|
|
No.
|
Percent
|
| Advice for more accessibility of mHealth wearable devices |
Making Government-subsidized smartwatches accessible to all low-income group members who need them |
24 |
33.8 |
| Ability to have free unlimited access to mHealth-based smartwatch data via web or mobile application (BP, heart rate, and weight) |
21 |
29.6 |
| Ensuring that stored data in mHealth applications and devices is safe |
13 |
18.3 |
| Involvement of my primary care provider/doctor in remote monitoring |
11 |
15.5 |
| Others |
1 |
1.4 |
| N/A |
1 |
1.4 |
| Total |
71 |
100.0 |
Discussion
Most Prevalent Hypertension Risk Factors in African-Born Immigrants
This causal-comparative study revealed the most prevalent risk factors leading to hypertension in African-born immigrants, which aligned with the research question (RQ1). These risk factors included unhealthy diet (21.7%), physical inactivity (21.7%), obesity (12.5%), and elevated BP (9.2%). The majority of the participants (51.6%) were either overweight or obese, with BMI values ranging between 25.9 kg/m2 and 41.6 kg/m2. The above-mentioned findings helped to answer RQ1. These risk factors make the target population feel vulnerable if they develop the disease (6). Hypertension risk factors differ in African-born immigrants and African Americans based on gender and the length of stay in the U.S. (22). African-born immigrants face lower risks of developing hypertension in the first few years of their arrival in the U.S. The longer the African-born immigrants stay in the U.S., the higher the risk of developing hypertension over time (25). Other studies suggest disaggregating data on the prevalence of hypertension by ethnic group and country of origin to inform public health strategies and reduce health disparities in chronic disease management (10).
The most effective evidence-based solution to address hypertension risk factors among African-born immigrants was lifestyle modification targeting obesity, unhealthy diet, and physical inactivity challenges. Using mHealth wearable devices, such as smartwatches (e-wrist watches), fitness trackers, and smart bracelets, is essential to prevent the exacerbation of hypertension. Lifestyle modifications align with the 2022 American Academy of Family Physicians clinical practice guideline on hypertension management in adults, emphasizing diet, healthy eating, and physical activity to prevent and treat hypertension to achieve a recommended BP equal to or lower than 130/80 mm Hg (26,27). In addition to lifestyle modification, the 2020 International Society of Hypertension (ISH) guideline recommends using mobile phones and other electronic devices to improve adherence to medication therapy (28). However, using mHealth devices should go beyond medication adherence to include regular home and ambulatory BP monitoring. In this study, research participants reported several challenges to achieving hypertension control, including limited access to primary care providers and irregular hypertension monitoring. Most research participants never checked their BP (36.8%) or did it once to twice a month (28.4%), probably due to the lack of education or limited access to BP monitoring devices.
The Benefits of mHealth Intervention in Hypertension Management
The identification of the benefits of mHealth wearable devices helped answer the RQ2, which included reminders to measure BP, perform physical activities, take medications promptly, and search for information about hypertension management. Individuals usually consider adopting a healthy lifestyle if it leads to their intended value (29). This study showed that participants in group 1 (who used smartwatches) achieved a lower MAP (99 mm Hg) at the end of six weeks of the study than the participants in group 2 (participants who used non-smart BP monitoring devices) (103 mm Hg) (P < 0.001). The results showed that the use of mHealth devices led to improvement in self-assessment. Research participants in group 1 were more consistent in measuring their BP and keeping it under control than participants in group 2. It was beyond the scope of this study to explore the impact of medication adherence on achieving hypertension control as noted in the limitations.
Participants’ perception of mHealth benefits to achieve hypertension control was central to this study. It entails how people believe their efforts to change behaviors lead to expected positive health benefits. The evidence showed that mHealth devices may be used to reduce hypertension risks. Patients may use interactive voice responses, text messaging with their providers, and various mobile applications to improve lifestyle behaviors (30,31). The results of this study showed that mHealth users from low-resource settings, including African-born immigrants, can benefit from mHealth interventions to improve hypertension management and change lifestyle behaviors. They help mitigate cardiovascular risk factors, such as overweight or obesity, physical inactivity, hypertension, and poor diet, reduce hospital readmissions, and improve cardiac health outcomes (32,33). Studies conducted in more than 30 low-income countries have shown that mHealth technology is feasible and can potentially enhance medication adherence (30).
TheCenters for Disease Control and Prevention (CDC) recommended using mHealth in managing hypertension with a large body of clinical evidence based on meta-analysis and systematic reviews of 27 studies (8). Smart mobile devices are increasingly used for patient education and monitoring of essential vital signs, including BP, blood glucose, pulse, and oxygen saturation. Other benefits of mobile applications or web-based platforms include communicating hypertension levels in real time with primary care providers for medical assistance. The benefits of using mHealth wearable devices far outweigh the risks, such as data safety concerns. Nevertheless, providers should strictly abide by bioethical guidelines to protect the privacy of patients’ identifiable information.
Strategies to Make mHealth Wearable Devices More Accessible to African-born Immigrants
The study participants prioritized making government-subsidized smartwatches accessible to all low-income group members who need them (33.8%). Additionally, having free unlimited access to data of mHealth-based smartwatches and ensuring the safety of their data were the most common strategies from respondents, which helped to answer RQ3. Most participants resided in low-income MUAs of Maricopa county (23). For improved management of mHealth wearable devices, participants prioritized integrating education on using smartwatches and getting frequent advice from primary care providers (46.9%). These approaches would address the participants’ challenge of limited education in using mHealth wearable devices. This study showed that 32% of research participants were unemployed, students, or retirees. Even 20% of self-employed participants did not have stable incomes, as they worked in informal sectors. Therefore, African-born immigrants would significantly benefit from federal and local government subsidies to afford smartwatches and subscription fees to the paid mHealth applications.
It was noted that 16.3% of the participants appreciated peer support networks and social accountability initiatives as resourceful strategies to make mHealth wearable devices more accessible and improve hypertension management. African-born immigrants still need guidance from their primary care providers and health coaches to select secure mHealth applications to ensure the safety of their BP and other vital data. Other studies also emphasized personalization or tailoring the mHealth content to the needs of individual users, reminders in the form of push notifications, stability of application design, and personal support (34,35). Other relevant approaches include ensuring data safety and transparency in reporting, external validation in diverse population groups, providing proactive counseling for people who use such devices, providing financial incentives, and creating low-cost devices (36,37). These results are similar to the findings of this study and would make mHealth wearable devices more accessible to African-born immigrants. Based on the results, 20.9% of respondents hoped to benefit from searching for hypertension management information using smartwatches.
The implications of this study for clinical settings include enhancing family physicians, nurses, and public health researchers’ understanding of hypertension risk factors in African-born immigrants. Healthcare professionals would benefit from the findings of this study tailoring mHealth interventions to the specific health needs of African-born immigrants for better hypertension control. They can customize hypertension education programs based on particular risk factors and low-resource settings. Family physicians and nurses can develop individualized care plans involving African-born immigrants with hypertension in BP monitoring using mHealth wearable devices. They can help monitor uncontrolled hypertension promptly after receiving mHealth-based notifications from African-born immigrants. Future research would investigate the role of healthcare professionals in educating African-born immigrants about the effective use of mHealth wearable devices to manage hypertension. It would consist of using mixed methods to better understand various hypertension risk factors such as environmental and interpersonal risk factors experienced by African-born immigrants. Future research would also examine the impact of smart wearable devices on adherence to antihypertensive medications.
The study has notable limitations, including the lack of exploration of environmental and interpersonal risk factors such as social group, which also contribute to hypertension. It was beyond its scope to explore the impact of mHealth wearable devices on medication compliance. Despite its limitations, this study has the potential to promote hypertension monitoring, education, and behavioral changes using mHealth wearable devices in African-born immigrants and other minority groups in the United States. The study contributed to strategies that local government and public health officials can use to support mHealth interventions for hypertension management in African-born immigrants.
Conclusion
This study contributed to the existing knowledge about the most prevalent hypertension risk factors and challenges of African-born immigrants in Maricopa county, Arizona, in managing hypertension. The study showed that most research participants living in MUAs struggle with sedentary lifestyles, including obesity or being overweight, physical inactivity, and an unhealthy diet (23). African-born immigrants are not often included in major studies as a distinct population group with specific health characteristics (38). This study showed that African-born immigrants could benefit from using mHealth wearable devices to prevent the exacerbation of hypertension and improve their BP monitoring and control. During the six weeks of the study, participants monitored their BP twice daily. Based on the results, there was a significant improvement in the MAP of group 1 participants (99 mm Hg) compared to group 2 participants (103 mm Hg) (P < 0.001). Making government-subsidized smartwatches accessible to all low-income group members, giving them free unlimited access to mHealth data, and ensuring the safety of their data would increase their access to mHealth wearable devices. African-born immigrants can achieve hypertension control if they understand the rationale for monitoring their BP, receive tailored education resources, and improve relationships with primary care providers and nurses. Overall, the benefits of using mHealth wearable devices far outweigh the risks, such as data safety concerns.
Acknowledgements
The authors are very grateful to Dr. Keith Pelletier, PhD, Dr. Chloè Fields, PhD, and Dr. Daniel Gochenour, DHSc, for their guidance and professional support. The authors are also indebted to the African-born immigrants who participated in the study.
Competing Interests
The authors have no competing interests associated with the material presented in this paper.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethical Approval
The study was approved by the Institutional Review Board of Liberty University (IRB-FY23-24-253). All participants signed a written consent before participating in the study (see Supplementary C). They agreed to participate voluntarily without coercion.
Funding
None.
Supplementary Files
Supplementary file 1 contains sections A (Recruitment Flyer), B (Consent Form to Participate in the Study), C (Blood Pressure Form for Group 1), D (Blood Pressure Form for Group 2), E (Questionnaire for Group 1), F (Questionnaire for Group 2).
(pdf)
References
- Maaß L, Freye M, Pan CC, Dassow HH, Niess J, Jahnel T. The definitions of health apps and medical apps from the perspective of public health and law: qualitative analysis of an interdisciplinary literature overview. JMIR Mhealth Uhealth 2022; 10(10):e37980. doi: 10.2196/37980 [Crossref] [ Google Scholar]
- Taylor HA Jr, Francis S, Evans CR, Harvey M, Newton BA, Jones CP. Preventing cardiovascular disease among urban African Americans with a mobile health app (the MOYO app): protocol for a usability study. JMIR Res Protoc 2020; 9(7):e16699. doi: 10.2196/16699 [Crossref] [ Google Scholar]
- Stampe K, Kishik S, Müller SD. Mobile health in chronic disease management and patient empowerment: exploratory qualitative investigation into patient-physician consultations. J Med Internet Res 2021; 23(6):e26991. doi: 10.2196/26991 [Crossref] [ Google Scholar]
- Dhingra LS, Aminorroaya A, Oikonomou EK, Nargesi AA, Wilson FP, Krumholz HM. Use of wearable devices in individuals with or at risk for cardiovascular disease in the US, 2019 to 2020. JAMA Netw Open 2023; 6(6):e2316634. doi: 10.1001/jamanetworkopen.2023.16634 [Crossref] [ Google Scholar]
- Garner SL, George CE, Young P, Hitchcock J, Koch H, Green G. Effectiveness of an mHealth application to improve hypertension health literacy in India. Int Nurs Rev 2020; 67(4):476-83. doi: 10.1111/inr.12616 [Crossref] [ Google Scholar]
- Voorheis P, Zhao A, Kuluski K, Pham Q, Scott T, Sztur P. Integrating behavioral science and design thinking to develop mobile health interventions: systematic scoping review. JMIR Mhealth Uhealth 2022; 10(3):e35799. doi: 10.2196/35799 [Crossref] [ Google Scholar]
- Chandrasekaran R, Katthula V, Moustakas E. Patterns of use and key predictors for the use of wearable health care devices by US adults: insights from a national survey. J Med Internet Res 2020; 22(10):e22443. doi: 10.2196/22443 [Crossref] [ Google Scholar]
- Centers for Disease Control and Prevention (CDC). High Blood Pressure Symptoms and Causes. 2023. Available from: https://www.cdc.gov/bloodpressure/about.htm. Accessed February 28, 2024.
- Abrahamowicz AA, Ebinger J, Whelton SP, Commodore-Mensah Y, Yang E. Racial and ethnic disparities in hypertension: barriers and opportunities to improve blood pressure control. Curr Cardiol Rep 2023; 25(1):17-27. doi: 10.1007/s11886-022-01826-x [Crossref] [ Google Scholar]
- Henry Osokpo O, James R, Riegel B. Maintaining cultural identity: a systematic mixed-studies review of cultural influences on the self-care of African immigrants living with non-communicable disease. J Adv Nurs 2021; 77(9):3600-17. doi: 10.1111/jan.14804 [Crossref] [ Google Scholar]
- Arizona Department of Health Services (ADHS). Arizona Medically Underserved Areas: Biennial Report. Phoenix: ADHS; 2022.
- National Centre for Health Statistics. National Health and Nutrition Examination Survey. Available from: https://www.cdc.gov/nchs/about/factsheets/factsheet_nhanes.htm. Accessed March 28, 2024.
- Maraboto C, Ferdinand KC. Update on hypertension in African-Americans. Prog Cardiovasc Dis 2020; 63(1):33-9. doi: 10.1016/j.pcad.2019.12.002 [Crossref] [ Google Scholar]
- Lu X, Yang H, Xia X, Lu X, Lin J, Liu F. Interactive mobile health intervention and blood pressure management in adults. Hypertension 2019; 74(3):697-704. doi: 10.1161/hypertensionaha.119.13273 [Crossref] [ Google Scholar]
- Ali SH, Islam NS, Commodore-Mensah Y, Yi SS. Implementing hypertension management interventions in immigrant communities in the US: a narrative review of recent developments and suggestions for programmatic efforts. Curr Hypertens Rep 2021; 23(1):5. doi: 10.1007/s11906-020-01121-6 [Crossref] [ Google Scholar]
- Mao Y, Lin W, Wen J, Chen G. Impact and efficacy of mobile health intervention in the management of diabetes and hypertension: a systematic review and meta-analysis. BMJ Open Diabetes Res Care 2020; 8(1):e001225. doi: 10.1136/bmjdrc-2020-001225 [Crossref] [ Google Scholar]
- Cao W, Milks MW, Liu X, Gregory ME, Addison D, Zhang P. mHealth interventions for self-management of hypertension: framework and systematic review on engagement, interactivity, and tailoring. JMIR Mhealth Uhealth 2022; 10(3):e29415. doi: 10.2196/29415 [Crossref] [ Google Scholar]
- Aggarwal R, Chiu N, Wadhera RK, Moran AE, Raber I, Shen C. Racial/ethnic disparities in hypertension prevalence, awareness, treatment, and control in the United States, 2013 to 2018. Hypertension 2021; 78(6):1719-26. doi: 10.1161/hypertensionaha.121.17570 [Crossref] [ Google Scholar]
- Shan R, Ding J, Plante TB, Martin SS. Mobile health access and use among individuals with or at risk for cardiovascular disease: 2018 Health Information National Trends Survey (HINTS). J Am Heart Assoc 2019; 8(24):e014390. doi: 10.1161/jaha.119.014390 [Crossref] [ Google Scholar]
- Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 2016; 134(6):441-50. doi: 10.1161/circulationaha.115.018912 [Crossref] [ Google Scholar]
- Chappell LC, Tucker KL, Galal U, Yu LM, Campbell H, Rivero-Arias O. Effect of self-monitoring of blood pressure on blood pressure control in pregnant individuals with chronic or gestational hypertension: the BUMP 2 randomized clinical trial. JAMA 2022; 327(17):1666-78. doi: 10.1001/jama.2022.4726 [Crossref] [ Google Scholar]
- Zilbermint M, Hannah-Shmouni F, Stratakis CA. Genetics of hypertension in African Americans and others of African descent. Int J Mol Sci 2019; 20(5):1081. doi: 10.3390/ijms20051081 [Crossref] [ Google Scholar]
- Ward J, Leitch C, Tu T. Community Health Status Report. 2020. Available from: https://www.maricopa.gov/DocumentCenter/View/66054/2019-Community-Health-Status-Report. Accessed April 18, 2024.
- Qiu L, Wang W, Sa R, Liu F. Prevalence and risk factors of hypertension, diabetes, and dyslipidemia among adults in Northwest China. Int J Hypertens 2021; 2021:5528007. doi: 10.1155/2021/5528007 [Crossref] [ Google Scholar]
- Turkson-Ocran RN, Nmezi NA, Botchway MO, Szanton SL, Golden SH, Cooper LA. Comparison of cardiovascular disease risk factors among African immigrants and African Americans: an analysis of the 2010 to 2016 National Health Interview Surveys. J Am Heart Assoc 2020; 9(5):e013220. doi: 10.1161/jaha.119.013220 [Crossref] [ Google Scholar]
- Chiu N, Chiu L, Aggarwal R, Raber I, Bhatt DL, Mukamal KJ. Trends in blood pressure treatment intensification in older adults with hypertension in the United States, 2008 to 2018. Hypertension 2023; 80(3):553-62. doi: 10.1161/hypertensionaha.122.19882 [Crossref] [ Google Scholar]
- Islam FM, Wong CK, Hosen MA, Bhowmik J. Perception of and practice in salt and fruit consumption and their associations with high blood pressure: a study in a rural area in Bangladesh. Appl Sci (Basel) 2023; 13(3):1622. doi: 10.3390/app13031622 [Crossref] [ Google Scholar]
- Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D. 2020 International Society of Hypertension global hypertension practice guidelines. J Hypertens 2020; 38(6):982-1004. doi: 10.1097/hjh.0000000000002453 [Crossref] [ Google Scholar]
- Vogel EA, Henriksen L, Schleicher NC, Prochaska JJ. Perceived susceptibility to and seriousness of COVID-19: associations of risk perceptions with changes in smoking behavior. Int J Environ Res Public Health 2021; 18(14):7621. doi: 10.3390/ijerph18147621 [Crossref] [ Google Scholar]
- Gong K, Yan YL, Li Y, Du J, Wang J, Han Y. Mobile health applications for the management of primary hypertension: a multicenter, randomized, controlled trial. Medicine (Baltimore) 2020; 99(16):e19715. doi: 10.1097/md.0000000000019715 [Crossref] [ Google Scholar]
- Alzahrani SA, Bin Muammar MF, Bin Muammar AF, Alolah A, Almutawa M. The adoption and acceptance of mHealth interventions for self-management of hypertension among adult patients: a systematic review. Cureus 2022; 14(11):e31584. doi: 10.7759/cureus.31584 [Crossref] [ Google Scholar]
- Khoong EC, Olazo K, Rivadeneira NA, Thatipelli S, Barr-Walker J, Fontil V. Mobile health strategies for blood pressure self-management in urban populations with digital barriers: systematic review and meta-analyses. NPJ Digit Med 2021; 4(1):114. doi: 10.1038/s41746-021-00486-5 [Crossref] [ Google Scholar]
- Hare AJ, Chokshi N, Adusumalli S. Novel digital technologies for blood pressure monitoring and hypertension management. Curr Cardiovasc Risk Rep 2021; 15(8):11. doi: 10.1007/s12170-021-00672-w [Crossref] [ Google Scholar]
- Springer MV, Malani P, Solway E, Kirch M, Singer DC, Kullgren JT. Prevalence and frequency of self-measured blood pressure monitoring in US adults aged 50-80 years. JAMA Netw Open 2022; 5(9):e2231772. doi: 10.1001/jamanetworkopen.2022.31772 [Crossref] [ Google Scholar]
- Li R, Liang N, Bu F, Hesketh T. The effectiveness of self-management of hypertension in adults using mobile health: systematic review and meta-analysis. JMIR Mhealth Uhealth 2020; 8(3):e17776. doi: 10.2196/17776 [Crossref] [ Google Scholar]
- Zinzuwadia A, Singh JP. Wearable devices-addressing bias and inequity. Lancet Digit Health 2022; 4(12):e856-7. doi: 10.1016/s2589-7500(22)00194-7 [Crossref] [ Google Scholar]
- Rinaldi G, Hijazi A, Haghparast-Bidgoli H. Cost and cost-effectiveness of mHealth interventions for the prevention and control of type 2 diabetes mellitus: a protocol for a systematic review. BMJ Open 2019; 9(4):e027490. doi: 10.1136/bmjopen-2018-027490 [Crossref] [ Google Scholar]
- Bains A, Osathanugrah P, Sanjiv N, Chiu C, Fiorello MG, Siegel NH. Diverse research teams and underrepresented groups in clinical studies. JAMA Ophthalmol 2023; 141(11):1037-44. doi: 10.1001/jamaophthalmol.2023.4638 [Crossref] [ Google Scholar]